An Examination of Management Patterns and Perceived Health Status of Patients with Osteoporosis within Bayelsa State
Peter A Owonaro1*, Daughter Awala Owonaro2, Timothy Gilbert3 and Adebukola A Sounyo4
1Department of Clinical Pharmacy & Pharmacy Practice, Faculty of Pharmacy, Niger Delta University, Wilberforce Island, Bayelsa State, Nigeria
2College of Health Technology Otuogidi, Bayelsa State, Nigeria
3Department of Family Medicine, Niger Delta University, Wilber
4Department of Clinical Pharmacy & Pharmacy Practice, Faculty of Pharmacy, Niger Delta University, Nigeria
Submission: November 07, 2023; Published: November 21, 2023
*Corresponding author: Peter A Owonaro, Department of Clinical Pharmacy & Pharmacy Practice, Faculty of Pharmacy, Niger Delta University, Wilberforce Island, Bayelsa State, Nigeria
How to cite this article: Peter A Owonaro*, Daughter Awala Owonaro, Timothy Gilbert and Adebukola A Sounyo. An Examination of Management Patterns and Perceived Health Status of Patients with Osteoporosis within Bayelsa State. Ortho & Rheum Open Access J. 2023; 22(3): 556090. DOI: 10.19080/OROAJ.2023.22.556090
Abstract
Osteoporosis, characterized by diminished bone mass and microarchitectural bone tissue degradation leading to heightened bone fragility and susceptibility to fractures, is a condition that often goes underdiagnosed and undertreated. This cross-sectional survey aimed to assess medication management and the perceived health status among a diverse group of osteoporosis patients, spanning a wide age range (20-80 years), within the general population of Yenagoa, Bayelsa State. The data collection period for this study extended from March 2022 to May 2022, and information was gathered using a questionnaire specifically developed by the researchers. The study population predominantly consisted of females (55%), primarily aged above 40 years, with a substantial proportion possessing technical education (33%). Most participants were married (82%), employed, and exhibited modal body weights within the range of 60-70 kg (25%). A noteworthy portion had a history of vitamin D supplementation (60%), although daily steroid use was less prevalent (56%). While a majority reported adherence to their prescribed medication regimen (64%), they displayed limited awareness of the potential risks associated with non-adherence (64%). Many participants sought treatment for osteoporosis from multiple healthcare facilities. The daily management of the condition was mainly overseen by bone specialists (40%) and local practitioners (34%).
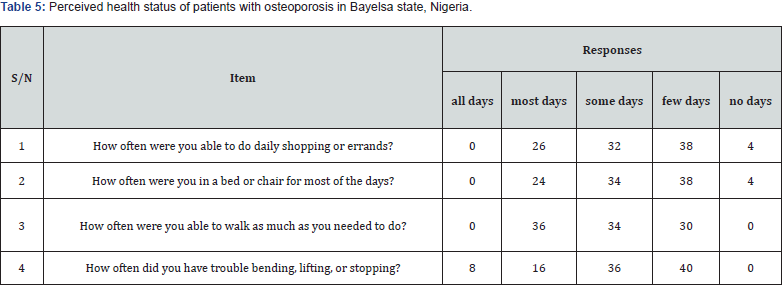
The study revealed several challenges faced by participants, including difficulties with daily shopping (38%), days spent in a sick bed (38%), reduced mobility (36%), limitations in engaging in physical activities (40%), and difficulties in handling fabrics (38%). Nevertheless, most participants expressed confidence in their ability to live independently without assistance (52%). The study findings underscored suboptimal levels of management and a decreased perceived health status, as evident by a decline in physical functioning. Considering these findings, the researcher recommends further exploration of osteoporosis medication management and health-related statuses in this patient population using alternative assessment tools. This approach can provide a more comprehensive insight into their overall health status.
Keywords: Yenagoa; Bayelsa State; Osteoporosis; Kolokuma/ Opokuma, Southern Ijaw; Ogbia; and Imbia
Introduction
Osteoporosis, a systemic ailment characterized by reduced bone mass and microarchitectural bone tissue deterioration, poses a significant public health challenge. It is a condition that leads to heightened bone fragility and an increased susceptibility to fractures in critical anatomical locations such as the hip, spine, and wrist [1]. Osteoporosis is a global concern with far-reaching consequences. According to estimates, the worldwide prevalence of osteoporosis among women aged 50 years and older is projected to be 22% in 2020 [2], and this number is expected to rise in the coming years. Despite its severe consequences and increasing prevalence, osteoporosis remains notably underdiagnosed and undertreated, with a treatment gap ranging from 50% to 80% [3,4]. The magnitude of the problem is further exacerbated by the fact that osteoporosis often remains asymptomatic until a fracture occurs [5]. This makes early diagnosis and intervention even more critical, as fractures have significant implications for patients’ health-related quality of life. Patients who have experienced fractures due to osteoporosis face an increased risk of disability, hospitalization, and mortality [6]. The socio-economic impact of osteoporotic fractures is substantial, with significant healthcare costs and a burden on healthcare systems.
The relationship between medication adherence and healthrelated quality of life in osteoporosis patients is a multifaceted issue that demands scrutiny. Non-adherence to medication regimens can have dire consequences, including a higher risk of fractures, increased healthcare costs, and a diminished quality of life [7,8]. Understanding the factors that contribute to nonadherence is essential to improving the quality of care for osteoporosis patients. Furthermore, assessing the health-related quality of life in these patients is critical to understanding the full extent of the impact of the disease and the treatment regimens on their well-being.
Recent research has indicated that medication adherence in osteoporosis patients is suboptimal, and factors such as the complexity of medication regimens, side effects, and patient beliefs can significantly affect adherence rates [4,7]. These factors underscore the need for a comprehensive examination of the relationship between adherence and health-related quality of life in this patient population. The current study aimed to address this significant gap in knowledge by conducting a crosssectional survey to evaluate medication adherence and assess the health-related quality of life among osteoporosis patients within the general populace of Yenagoa, Bayelsa State. Considering the gravity of osteoporosis as a public health concern and the potential impact of non-adherence on patients’ quality of life, this research contributes valuable insights that may inform strategies for enhancing the care and management of individuals with osteoporosis. It also highlights the need for a more comprehensive understanding of the patient population’s health status, utilizing alternative assessment tools to provide a holistic view of their health needs.
In this context, the present paper aims to explore the medication adherence behaviors and the health-related quality of life among osteoporosis patients in Bayelsa State, offering a more in-depth understanding of the challenges they face and the potential areas for intervention and support.
Method
Study Design and Setting
The research design for this study was a Cross-Sectional Survey design. A cross-sectional survey design involves collecting data from a specific population at a single point in time. The area of the study was Yenagoa metropolis of Bayelsa state of Nigeria. Yenagoa is reported to have an area of 706km3 with a population of 352,285 from the 2016 National census projected to 2017. English language, Ijaw, and Epie-Atissa are the major dialects of the area. The study area shares common boundaries with Kolokuma/ Opokuma, Southern Ijaw, Ogbia, and Imbiama respectively. Occupationally, the people of Yenagoa engage in business, farming, fishing, and civil servants.
Target Population and Sampling
The population of this study used was comprised of male and female osteoporosis patients within the age brackets of 20 and 80 years living in Bayelsa State, from March 2022 to May 2022. A non-probabilistic sampling technique was used for this study. Snowballing was done for the patient population to achieve a possible even distribution of the respondents across the region of the study. Patients were approached at their convenience. For this study, a sample size of one hundred (100) was obtained.
Instrumentation and Measures
A researcher-constructed questionnaire was used in the study. The instrument was made of three sections, section A, section B, and Section C. Section A contained questions about demographic characteristics whereas Section B and Section C contained questions about adherence and health-related quality of life of patients with osteoporosis for the study. A pilot survey with ten (10) copies in a nearby Hospital in Yenagoa having a similar characteristic to the study population, reported a 0.78 Chronbach’s alpha.
Ethical Clearance, Data Collection/Analysis
After receipt of the letter of ethical clearance from the College of Health Technology, Otuogidi, ethical committee, participants of this study were approached at their convenience. The essence of the study was explained, and the instrument was administered. It was usually made sure that the participant filled out the instrument or was helped in filling out the instrument and was retrieved immediately. Data was analyzed using appropriate statistical tools (SPSS 27). Descriptive statistics were run, and results were shown in tables and charts.
Results
Socio-demographic characteristics of patients with osteoporosis in Bayelsa state, Nigeria
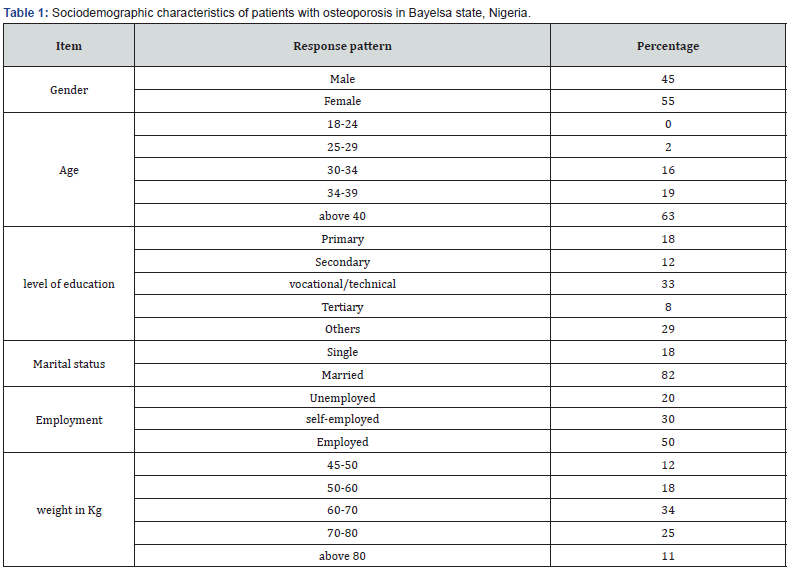
The modal demographic responses in this study were more females (55%) of ages above 40 years with vocational or technical education (33%), married (82%), employed, and having modal body weights of 60-70kg (25%). This is shown in Table 1 below.
Management of Patients with Osteoporosis
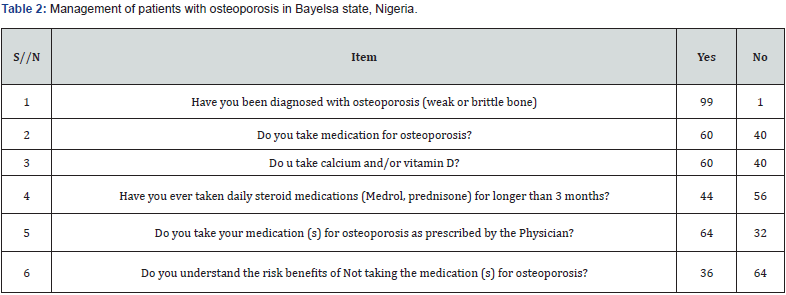
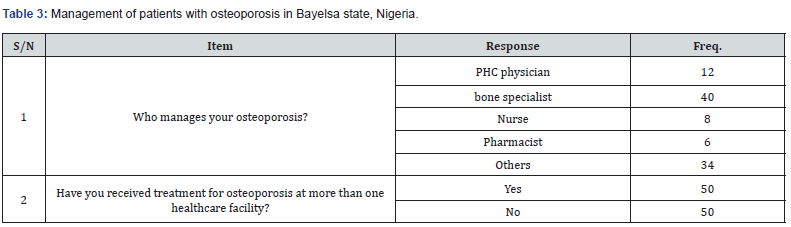
The study reveals that most of the participants in this study have been diagnosed with osteoporosis (99%) and are on vitamin D (60%) but not usually on daily steroids for more than three months before the study (56%). They claim to have been taking their medication as prescribed by the physician (64%) but confess to not understanding the risk of not taking the medication (s) for osteoporosis (64%). The study in the region also revealed that although most of the participants report having received treatment for osteoporosis at more than one healthcare facility, the day-to-day management of osteoporosis is said to be handled by bone specialists (40%) and other local practitioners (34%). This is shown in Tables 2 & 3 below.
Perceived Health Status of Patients with Osteoporosis
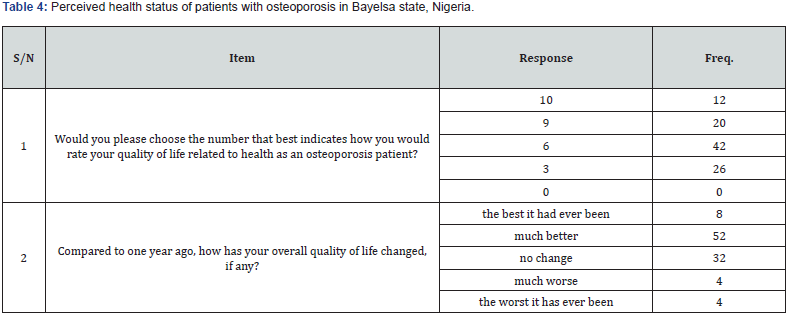
Participants reported a modal self-acclaimed average quality of life which is much better compared to one year ago after taking medications (52%). The practical daily life osteoporosis life quality report was that for a few days, they were able to do daily shopping or errands (38%), they were in a bed or chair for most of the days (38%), for most days they were able to walk as much as needed to do (36%), and for few days they were having trouble bending, lifting or stopping (40%). Participants also reported that they sometimes had problems with changing the type of clothes they wear because of difficulty in dressing (38%) but feel confident that they could live on their own without assistance (52%). Tables 4-6 below contain the above information.

Discussions of Findings
The findings of this study illuminate several key aspects of osteoporosis management and the quality of life among individuals in the study region. Notably, the study revealed an improved awareness of osteoporosis; however, it also identified areas of concern, such as average adherence to osteoporosis management and a lack of knowledge regarding the consequences of not adhering to prescribed medication management.
Medication management adherence
While the study indicates that a significant proportion of participants entrusted the day-to-day management of their osteoporosis to bone specialists (40%) and other local practitioners (34%), it is essential to recognize the importance of adherence to prescribed medication management. This is in line with recommendations from the literature, which underscore the need for early detection, treatment, and patient education to prevent deterioration and disability, improve prognosis, enhance quality of life, and reduce the risk of premature death [3].
It is worth noting that studies have highlighted challenges related to medication management adherence, with a significant proportion of patients failing to adhere to their osteoporosis treatment, particularly in the first three to six months of therapy (Kothawala, 2007). This underscores the need for strategies to improve medication adherence, such as follow-up phone calls or visits, which have shown promise in enhancing compliance (Cramer, 2006). Additionally, research supports alternative dosing regimens, such as weekly bisphosphonate dosing versus daily, or monthly dosing versus weekly, to promote better compliance (Cooper, 2006; Emkey, 2005; Recker, 2005).
Quality of Life
The study also reports a low quality of health status among individuals with osteoporosis, manifesting as physical discomforts related to daily activities, mobility, and clothing preferences. This observation aligns with previous research indicating that individuals with osteoporosis tend to experience a reduced quality of life, even in the absence of fractures [9]. Some studies have identified these differences in significant social activities [10]. It is important to note that osteoporosis itself may not directly affect the quality of life but rather its complications, particularly fractures, emerge as the primary factors contributing to the decline in quality of life [11,12].
Conclusion
These study findings highlight the need for comprehensive interventions that address both medication management adherence and the factors contributing to reduced quality of health status among individuals with osteoporosis. The development of educational programs, follow-up strategies, and alternative dosing regimens may contribute to more effective management and enhanced quality of life for this patient population [13-25].
Public Health Implications and Recommendations
The study’s findings underline the suboptimal management levels and a decreased perceived health status among osteoporosis patients in the Yenagoa region of Bayelsa State [26-30]. The implications of these findings necessitate a comprehensive approach to address the challenges posed by osteoporosis in this This includes:
i. Developing educational programs for healthcare providers to enhance their understanding of osteoporosis, early diagnosis, and treatment strategies.
ii. Establishing patient education initiatives to improve medication adherence and raise awareness of the condition’s significance [30-35].
iii. Integrating a multidisciplinary approach to osteoporosis management, considering both medical and psychosocial aspects.
iv. Conduct further research using alternative assessment tools to gain a more comprehensive understanding of the health status and needs of this patient population.
Contribution to knowledge
In conclusion, the study contributes to the existing body of knowledge by shedding light on the challenges and opportunities for osteoporosis management in the Yenagoa region of Bayelsa State. It emphasizes the importance of a holistic approach to healthcare delivery to improve the quality of life and well-being of individuals affected by osteoporosis [36-40].
References
- World Health Organization (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: Report of a WHO Study Group. World Health Organ Tech Rep Ser 843: 1-129.
- Johnell O, Kanis, JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int17(12): 1726-1733.
- Kanis JA, McCloskey EV, Cooper C, Rizzoli R, Reginster JY, (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24(1): 23-57.
- Siris ES, Modi A, Tang J, Gandhi N (2014) Health-related quality of life and adherence to bisphosphonate therapy in osteoporotic patients. Current Medical Research and Opinion 30(1): 247-253.
- Cosman F, De Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, et al. (2014) Clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int 25(10): 2359-2381.
- Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA (2015) Center, patient, and general practice characteristics are associated with fracture-related hospitalization in general practice. Osteoporos Int 26(1): 155-161.
- Gold DT, Horne R (2010) Psychological and behavioral factors in patients with osteoporosis. Rheumatic Disease Clinics of North America 36(4): 707-719.
- Hiligsmann M, Salas M, Hughes DA, Manias E, Gwadry-Sridhar F, et al. (2012) Interventions to improve osteoporosis medication adherence and persistence: A systematic review and literature appraisal by the ISPOR Medication Compliance & Persistence Special Interest Group. Osteoporos Int 23(12): 2903-2913.
- Compston JE, Flahive J, Hooven FH, Anderson Jr FA, Adachi JD, et al. (2014) Obesity, health-care utilization, and health-related quality of life after fracture in postmenopausal women: Global Longitudinal study of Osteoporosis in Women (GLOW). Calcif Tissue Int 94(2): 223-231.
- Hassanzadeh J, Nasimi B, Ranjbar-Omrani GH, Moradi-Nazar M, Mohammadbeigi A (2012) Evaluating the Quality of Life of osteoporotic postmenopausal women (Persian). Iranian Journal of Endocrinology and Metabolism 14(3): 234-240.
- Borgström F, Zethraeus N, Johnell O, Lidgren L, Ponzer S, et al. (2005) Costs and quality of life associated with osteoporosis-related fractures in Sweden. Osteoporosis Int 17(5): 637-650.
- Dempster DW (2011) Osteoporosis and the burden of osteoporosis-related fractures. Am J Manag Care 17(6): 164-169.
- Altindag O, Soran N (2014) Osteoporosis significantly reduces the quality of life. Gaziantep Med J 20(3): 217-220.
- Aziz ZadehForouzi M, Haghdoost A, Saidzadeh Z, Mohamadalizadeh S (2009) Study of knowledge and attitude of Rafsanjanian female teachers toward prevention of osteoporosis (Persian). J Birjand University of Med Sci 16(1): 71-77.
- Bagheri P, Haghdoost A, DortajRabari E, Halimi L, Vafaei Z, et al. (2011) Ultra analysis of the prevalence of osteoporosis in Iranian women “A Systematic Review and Meta-analysis” (Persian). Iranian Journal of Endocrinology & Metabolism 13(3): 315-325.
- Cook DJ, Guyatt GH, Adachi JD, Epstein RS, Juniper EF, et al. (1999) Development and validation of the mini-Osteoporosis Quality of Life Questionnaire (OQLQ) in osteoporotic women with back pain due to vertebral fractures. Osteoporosis Quality of Life Study Group. Osteoporos Int 10(3): 207-213.
- De Oliveira Ferreira N, Arthuso M, Da Silva R, Pedro AO, Neto AMP, et al. (2009) Quality of life in women with postmenopausal osteoporosis: Correlation between Qualeffo 41 and SF-36. Maturitas 62(1): 85-90.
- Deo P, Nayak R, Rajpura J (2013) Women’s attitudes and health beliefs toward osteoporosis screening in a community pharmacy. J Osteoporos 2013: 1-8.
- DoostiIrani A, Poorolajal J, Khalilian A, Esmailnasab N, Cheraghi Z (2013) Prevalence of osteoporosis in Iran: A meta-analysis. J Res Med Sci 18(9): 759-766.
- El-Shazly S, Mahmoud N (2007) Measuring the Quality of Life among elderly with osteoporosis. Alexandria Scientific Nursing J 6(2): 23-37.
- EsmaeiliShahmirzadi S, Shojaeizadeh D, Azam K, Tol A (2013) A survey on Quality of Life in the elderly with osteoporosis (Persian). Health Sys Res 8(7): 1180-1189.
- Gil KM, Gibbons HE, Hopkins MP, Jenison EL, VonGruenigen VE (2007) Baseline characteristics influencing the quality of life in women undergoing gynecologic oncology surgery. Health QualLife Outcomes 5(25): 1-7.
- Ha JY, Choi EY (2013) Health perception, health concern, and health promotion behavior of the elders (Korean). J Korean Gerontological Nursing 15(3): 277-285.
- Keramat A, Patwardhan B, Larijani B, Chopra A, Mithal A, Chakravarty D, et al. (2008) The assessment of osteoporosis risk factors in Iranian women compared with Indian women. Comparative Study, BMC Musculoskelet Disorder 9: 28.
- Korkmaz N, Tutoğlu A, Korkmaz I, Boyacı A (2014) The relationships among vitamin D level, balance, muscle strength, and quality of life in postmenopausal patients with osteoporosis. J Phys Ther Sci 26(10): 1521-1526.
- (2015) KSBMR. Osteoporosis health information: What osteoporosis.
- Kuru P, Akyuz G, PeynirciCersit H, Celenlioglu AE, Cumhur A, et al. (2015) Fracture History in osteoporosis: Risk factors and its effect on quality of life. Balkan Med J 31(4): 295-301.
- Lee SH (2014) A Study on regional bone mineral density by osteoarthritis grade of the knee data from 2010–11 Korea national health and nutrition examination survey [MSc. thesis]. Seoul: The Graduate School of Public Health Seoul National University.
- Lips P, Cooper C, Agnusdei D, Caulin F, Egger P, et al. (1999) Quality of life in patients with vertebral fractures: Validation of the Quality-of-Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO). Osteoporos Int 10(2): 150-160.
- Malgo F, Appelman-Dijkstra NM, Termaat MF, Van Derheide HJ, Schipper IB, et al. (2016) High prevalence of secondary factors for bone fragility in patients with a recent fracture independently of BMD. Arch Osteoporos 11(1): 12.
- Monshipour SM, MokhtariLakeh N, Rafat F, KazemnezhadLeyli E (2016) Related factors to menopausal women’s Quality of Life in Rasht (Persian)]. Holistic Nursing and Midwifery J 26(1): 80-88.
- Munch S, Shapiro S (2006) The silent thief: Osteoporosis and women’s health care across the life span. Health Soc Work 31(1): 44-53.
- Murrell P, Todd CJ, Martin A, Walton J, Lips P, Reeve J (2001) Postal administration compared with nurse-supported administration of the QUALEFFO-41 in a population sample: Comparison of results and assessment of psychometric properties. Osteoporos Int12(8): 672-679.
- NobakhtMotlagh F, KhaniJihoni A, Haidarnia A, Kave M, Hajizadeh E, et al. (2013) Prevalence of osteoporosis and its related factors in women referred to Fasa's densitometry Center (Persian)]. Scientific Journal of Ilam University of Medical Sci 21(4): 150-158.
- Saag KG, Sambrook P, Watts NB (2008) Osteoporosis. In: Klippel JH, Stone JH, Crofford LJ, White PH, editors. Primer on Rheumatic Diseases. New York: Springer.
- Shojaezadeh D, Sadeghi R, Tarrahi MJ, Asadi M, Lashgarara B (2012) Application of health belief model in the prevention of osteoporosis in volunteers of Khorramabad city health centers, Iran (Persian). J Health Sys Res 8(2): 183-192.
- Solomon DH, Johnston SS, Boytsov NN, McMorrow D, Lane JM, et al. (2014) Osteoporosis medication use after hip fracture in U.S. patients between 2002 and 2011.Journal of Bone and Mineral Res 29(9): 1929-1937.
- Stetzer E (2011) Identifying risk factors for osteoporosis in young women and practice.Internet Journal of Allied Health Sciences and Practice 9(4): 1-8.
- Strom O, Borgstrom F, Kanis JA, Compston J, Cooper C, McCloskey EV, et al. (2011) Osteoporosis: Burden, health care provision and opportunities in the EU: A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 6(1-2): 59-155.
- Wilson S, Sharp CA, Davie MWJ (2012) Health-related quality of life in patients with osteoporosis in the absence of vertebral fracture: A systematic review. Osteoporos Int 23(12): 2749-2768.






























