Severity of Hip Displacement in Relation to Subtypes and Motor Function in Cerebral Palsy- Role of Hip Surveillance
Kunju PAM*, Gisi Shibu and Amruthalal
Professor and Head Dept of Pediatric Neurology, Medical college, India
Submission: August 28, 2018;Published: September 07, 2018
*Corresponding author: Kunju PAM, Professor and Head Dept of Pediatric Neurology, Medical college, Trivandrum, Kerala, India.
How to cite this article: Kunju PAM, Gisi Shibu, Amruthalal. Severity of Hip Displacement in Relation to Subtypes and Motor Function in Cerebral Palsy - Role of Hip Surveillance. Ortho & Rheum Open Access J 2018; 12(5): 555848. DOI: 10.19080/OROAJ.2018.12.555848.
Abstract
Background: Hip dislocation in children with cerebral palsy (CP) is a common and often over looked problem by the treating pediatricians. Though it can be diagnosed early by using radiographs, knowledge about the standardized methodology and need for periodic surveillance is lacking among primary care pediatricians. Hip surveillance by X-ray pelvis can identify early hip dislocation and it is shown that early intervention may prevent the need for surgery [1].
Methods: The study was done in a tertiary care hospital as a onetime radiological evaluation of children with CP between the age group of 4-9 yrs. One hundred and one children with CP formed our study population.Clinical evaluation for details regarding CP type and assessment of motor ability by gross motor function classification system (GMFCS) was done. A hip X-ray was done for calculation of, migration index for establishing or ruling out hip displacement. Migration percentage (MP) in relation to CP subtypes and GMFCS grades were done.
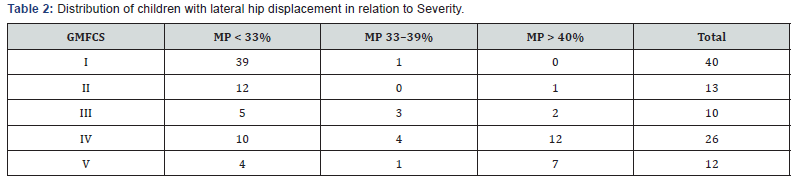
Results: There were 48 boys and 53 girls (mean age 4.80 years). 12 children were Gross Motor Function Classification System (GMFCS) level 5, while 26 were GMFCS level 4. Out of 36 hemiplegic CP only one had MP > 40. out of 6 children with spastic quadriplegia, 5 (83%) had MP > 40%. Spastic diplegic and choreoathetotic subtypes showed MP >40% in 9 out of 43 and 7 out of 16 respectively.According to the gross motor function classification system, GMFCS level I had no child with MP > 40%. Whereas 50% of children in GMFCS level IV and V had MP > 40% compared to only 4.76% in GMFCS I and II put together.
Conclusion: All the children in this study did not undergo a hip X-ray prior to this study. 22 out of 101 children had severe degree of hip displacement. The maximum number of hip displacements was seen in children with spastic quadriplegia; Spastic diplegic and choreoathetotic subtypes showed intermediate risk of hip displacement and hemiplegia had very low risk. According to the gross motor function classification system,GMFCS level I had no child with MP > 40%. Whereas 50% of children in GMFCS level IV and V had MP > 40%. The study showed the relationship between the CP subtypes and the severity of the motor involvement. It also emphasized the need for early hip surveillance.
Keywords: Hip dislocation; Cerebral palsy; Lateral Displacement; Hip surveillance
Introduction
In children with spastic cerebral palsy reduced activity of the hip abductor muscles in comparison to the spastic adductors leads to diminished growth of the greater trochanter of femur results in pathologic deformities of the hips-femoral anteversion and coxa valga antetorsa [2]. If untreated, dislocation of the hip typically occurs at age 2–7 years with a maximum at the age of 6 years. The incidence of hip displacement in cerebral palsy is related to the severity of involvement; varying from 1% in children with spastic hemiplegia, up to 75% in those with spastic quadriplegia [2,3]. So periodic evaluation of hip function is essential for early intervention and preventive measures.
Hip surveillance is defined as: “The process of monitoring and identifying the critical early indicators of hip displacement” [4].Hip displacement refers to the displacement of the femoral head laterally out of the acetabulum and is measured using a migration percentage (MP). Hip subluxation refers to hip displacement where the femoral head is partially displaced from under the acetabulum while hip dislocation refers to hip displacement where the femoral head is completely displaced from under the acetabulumn [5,6].Hip surveillance is important, to prevent morbidity of spastic hip disease-The aim of the management in children with spastic hip displacement is to maintain flexible, well-located and painless hips with a symmetrical range of movement. The key to achieving this goal is early identification and intervention.
Periodic hip surveillance also helps to reduce the need for extensive surgical procedures which is highly specialized area of orthopedics which may not be available in every center. So primary care pediatrician has a role for hip surveillance and timely referral.
Patients and Methods
The study was done in a pediatric neurology department of a tertiary care hospital as a onetime radiological evaluation of children with CP between the age group of 4-9 yrs prior to the referral to orthopedics. One hundred and one children between the age group of 4-9 yrs. with the diagnosis of CP formed our study population.A pediatric neurologist and physiotherapist in the department examined the children and completed an assessment form. Clinical evaluation for details regarding CP subtype and assessment of motor ability by gross motor function classification system (GMFCS) [6] was done. Winters, Gage, Hicks (WGH) gait type was determined, in addition to inquiring regarding pain during history taking. Orthopedic consultations done whenever required.
Radiographic Examination
Decision for referral for surgery depends on the degree of displacement of the femoral head and acetabular dysplasia. The migration percentages as described by Reimers and the acetabular index described by Hilgenreiner are the conventional measurements of displacement of the hip and acetabular dysplasia in young children with cerebral palsy.Radiographic assessment consists of measurement of migration percentage (MP) from a supine AP pelvis radiograph with standardized positioning [7] (Figure 1). Reimers Hip Migration Percentage is the percentage of body width of femoral capital epiphysis displaced out of the acetabulum (which falls lateral to perkins line) [8].Measurement of migration percentage of femoral head was done as given in the (Figure 2).

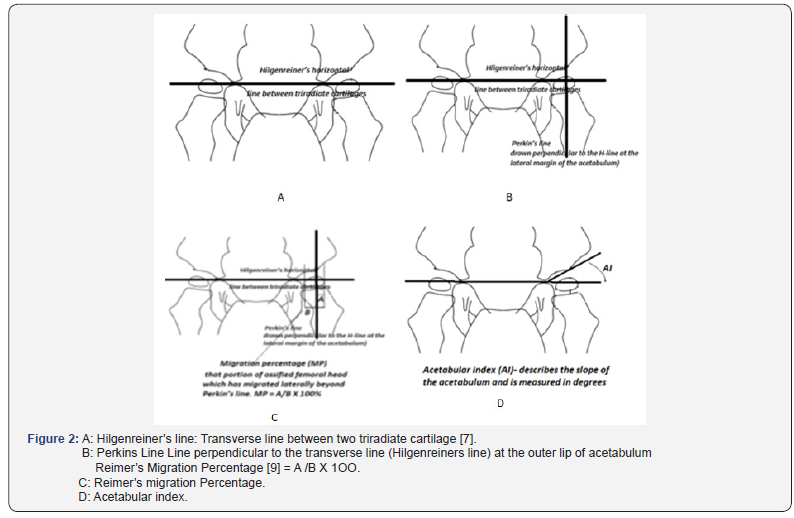
In the adult or older child, where the triradiate cartilages are fused and therefore inapparent, the inferior margin of the pelvic teardrop is used instead.The acetabular angle using Hilgenreiner’s line should be less than 28°at birth. The angle should become progressively shallower with age and should measure less than 22° at and beyond 1 year of age.
Present study an anteroposterior (AP) pelvic radiograph at the time of first visit was done. Any decrease in the range of movement at the hip or presence of scoliosis was a definite indication for further detailed radiological examination & immediate referral. In the present study 101 children were assessed between 4 and 9 years of age. Children with MP > 33% and > 40% were compared in relation to those with MP below these limits. Migration percentage (MP) in relation to CP subtypes and GMFCS grades were done.
Results
There were 48 boys and 53 girls (mean age 4.80 years). Distribution of Cerebral Palsy sub types were as follows. Hemiplegic 36 (35.64%), Quadriplegic 6(5.94%), Diplegic 43(42.57%) and Choreo athetotic 16(15%). 12 children were Gross Motor Function Classification System (GMFCS) level 5, while 26 were GMFCS level 4. Results of hip displacement by radiography as measured by MP in relation to CP subtypes and motor severity are presented in (Tables 1&2) and (Figure 3).
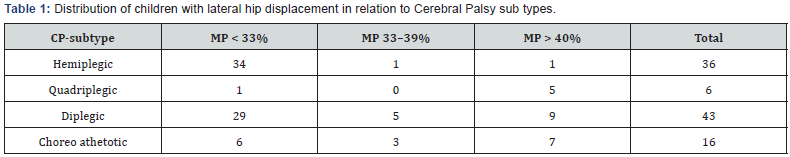
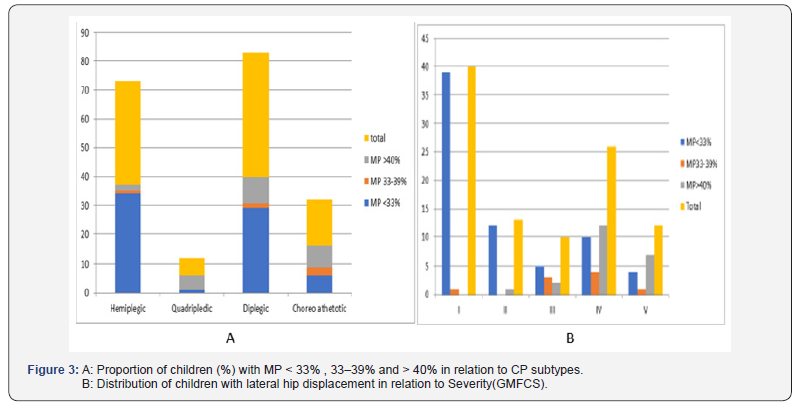
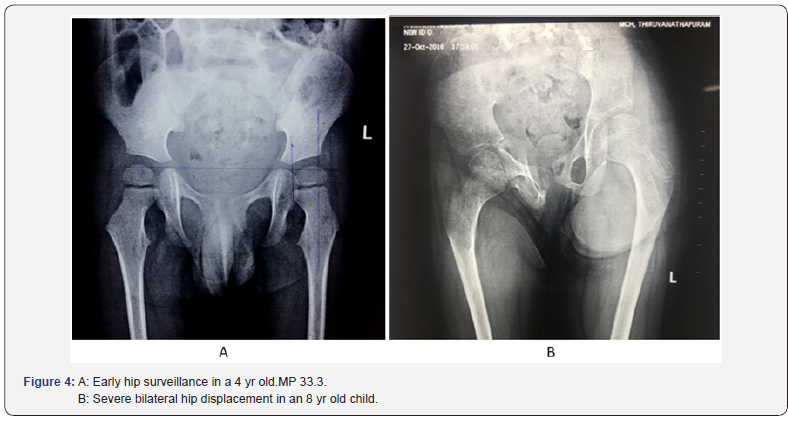
Only one child out of 36 children with spastic hemiplegia developed MP > 40%. The maximum number of hip displacements was seen in children with spastic quadriplegia, where 5 of 6 children (83%) had MP > 40%. Spastic diplegic and choreoathetotic subtypes showed intermediate risk of hip displacement (9 out of 43 and 7 out of 16 respectively had MP >40%). In the present study onset of hip displacement could not be assessed as hip surveillance was not done in a periodic basis. Figure 4 shows x-ray hip of 4-year-old with very minimal displacement (MP 33.33%) and Figure 4 shows severe hip displacement in an 8-year-old child.
According to the gross motor function classification system, GMFCS level I had no child with MP > 40%. Whereas 50% of children in GMFCS level IV and V had MP > 40% compared to only 4.76% in GMFCS I and II put together.
Discussion
The natural history of spastic hip disease of CP is progressive lateral displacement of the hip secondary to spasticity and muscle imbalance in the major muscle groups around the hip. Displacement may progress to severe subluxation, secondary acetabular dysplasia, deformity of the femoral head, dislocation and painful degenerative arthritis [4,5]. The long-term effects of dislocation of the hip can be disastrous for individual patients leading to pain and loss of the ability to sit comfortably in up to 50% of cases [6]. Other problems include difficulty with perineal care and personal hygiene, pelvic obliquity and scoliosis, poor sitting balance and loss of the ability to stand and walk [7-11].
A hip is usually considered to be subluxed,if the migration is equal to or greater than 33%. Reimers [17] found that among normal, the 90th gentile for migration percentage at four years was 10% with spontaneous migration of less than 1% per year. An unstable migration percentage is when progression is greater than or equal to 10% over 1 year [12-16]. Present study has shown that even a single radiological evaluation could identify hip displacement in children after the age of 4 yrs. Majority of (5 out of 6) quadriplegic CP, had severe type of hip displacement compared to hemiplegic CP (1 out of 36). Compared to other bilateral types of CP diplegia had lower rate of hip displacement (9 out of 43). This may be because of the less motor function impairment. So GMFCS may be a better predictor for early prediction of hip structural impairment. It is seen that there is direct correlation between the GMFCs class and severe hip displacement. According to the gross motor function classification system, GMFCS level I had no child with MP > 40%. Whereas 50% of children in GMFCS level IV and V had MP > 40% compared to only 4.76% in GMFCS I and II put together.
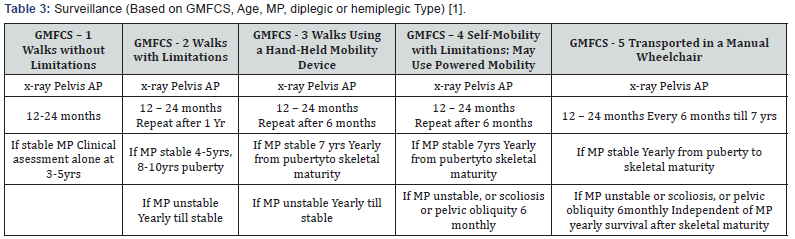
Subtyping of CP may have a role in predicting occurrence of severe hip displacement as shown by the almost complete occurrence in quadriplegic CP. However, a mere clinical examination and subtyping will not help in identifying severe hip disease in other type of CP. So, a systematic analysis of GMFCS is required for intensified screening of hip dysfunction. Moreover, as described in various guide lines periodic hip surveillance is mandatory for better ambulation and avoidance of surgery. This can be attained by early intervention measures. Figure 4 itself shows the importance of early surveillance. AACPDM - (American Academy for Cerebral Palsy and developmental medicine) recommends following schedule of hip surveillance (Table 3).
Conclusion
Need for hip evaluation in children with CP is emphasized by this study. All the children in this study did not undergo a hip Xray prior to the study. 22 out of 101 children had severe degree of hip displacement. The maximum number of hip displacements was seen in children with spastic quadriplegia and hemiplegia had very low risk. According to the gross motor function classification system, GMFCS level I had no child with MP > 40%. Whereas 50% of children in GMFCS level IV and V had MP > 40 %. The study showed the relationship between the CP subtypes and the severity of the motor involvement in producing hip displacement. Referral to an orthopedic surgeon with experience in treating hip displacement in children with CP is recommended when there is presence of hip pain on history and/or physical examination. Periodic hip surveillance is mandatory for early detection of hip displacement. When the migration percentage is greater than 30% and/or there is less than 30 degrees of hip abduction with or without other findings, referral to an orthopedic surgeon is recommended [1,17].
References
- Iizuka Y, Iizuka H, Tsutsumi S, Nakagawa Y, Nakajima T, et al. (2009) Foot drop due to lumbar degenerative conditions: Mechanism and prognostic factors in herniated nucleus pilposus and lumbar canal stenosis. J Neurosurg Spine 10(3): 260-264.
- Kertman H, Gurer B, Yimaz ER, Sekerci Z (2015) Acute bilateral isolated foot drop: Report of two cases. Asian J Neurosurg 10(2): 123-125.
- Kershenbaum A, Jaffa T, Zeman A, Boniface S (1997) Bilateral foot drop in patient with anorexia nervosa. Int J Eat Disord 22(3): 335-337.
- Bhansali A, Chandran V, Ramesh J, Kashyap A, Dash RJ (2000) Acute myxoedema: An unusual presenting manifestation of hypothyroid myopathy. Postgrad Med J 76: 99-100.
- Gabriella SE, Gunashekhar NP (1994) Bilateral foot drop, weight loss and rectal bleeding as an acute presentation of crohn’s disease. Postgrad Med J 70(828): 762-763.
- Wilbers J, Idema A, Gijtenbeek A (2010) A bilateral foot drop due to neuroschistosomiasis. J Neurol 257(5): 853-855.
- Eskandary H, Hamzei A, Yasamy MT (1995) Foot drop following brain lesion. Surg Neurol 43(1): 89–90.
- Chang HS, Nakagawa H, Mizuno J (2000) Lumbar herniated disc presenting with cauda equine syndrome. Long term follow up of four cases. Surg Neurol 53(2): 100-105.
- Vigasio A, Marcoccio I, Patelli A, Mattiuzzo V, Prestini G. New tendon transfer for correction of drop-foot in common peroneal nerve palsy. Clin Orthop Relat Res 466: 1454-1466.
- Yeganeh MM (2016) Triple tendon transfer for correction of foot deformity in common peroneal nerve palsy. Foot Ankle Int 37(6): 665- 669.
- Ober FR (1933) Tendon transplantation in the lower extremity. N Engl J Med 209: 52-59.
- Watkins MB, Jones JB, Ryder CT Jr, Brown TH Jr (1954) Transplantation of the posterior tibial tendon. J Bone Joint Surg Am 36: 1181-1189.
- Anderson JG (1963) Foot drop in leprosy and its surgical corrections. Acta Orthop Scand 33: 151-171.
- Richard BM (1989) Interosseous transfer of tibialis posterior for common peroneal nerve palsy. J Bone Joint Surg Br 71(5): 834-837.
- Srinivasan H, Mukherjee SM, Subramaniam RA (1968) Two-tailed transfer of tibialis posterior for correction of foot-drop in leprosy. J Bone Joint Surg Br 50(3): 623-638.
- Lipscomb PR, Sanchez JJ (1961) Anterior transplantation of the posterior tibial tendon for persistent palsy of the common peroneal nerve. J Bone Joint Surg Am 43(1): 60-66.
- Ozkan T, Tuncer S, Ozturk K, Aydin A, Ozkan S (2007) Surgical restoration of drop foot deformity with tibialis posterior tendon transfer. Acta Orthop Traumatol Turc 41(4): 259-265.






























