A Study of Surgical Approach to Typhoid Ileal Perforation at a Tertiary Care Hospital of South Gujarat
Archana Nema*
Department of surgery, Veer Narmad South Gujarat University, India
Submission: March 13, 2018;Published: May 21, 2018
*Corresponding author: Archana Nema, Department of surgery, Veer Narmad South Gujarat University, Icon hospital, India, Tel: 9825415006; Email: archana.nema@yahoo.in
How to cite this article: Archana Nema. A Study of Surgical Approach to Typhoid Ileal Perforation at a Tertiary Care Hospital of South Gujarat. Open Access J Surg. 2018; 9(2): 555757. DOI: 10.19080/OAJS.2018.09.555757.
Abstract
Introduction: Even with variety of procedures, typhoid (enteric) perforation still has a high rate of morbidity and mortality. The aim of the present study is to study clinical presentations, to evaluate management pattern of typhoid ileal perforation, to determine mortality and morbidity of perforation and to study the re-exploration rate and causes of re-exploration and its effect on mortality and morbidity.
Methods: This prospective observational study was conducted in the Departments of Surgery at Surat Municipal Institute of Medical Education & Research, Surat during June 2008 till October 2010. A total 45 patients with typhoid ileal perforation were included in the study. Among them, 32 cases (71%) undergone the simple primary closure of the perforation and peritoneal lavage after refreshing the edge, 7 cases (16%) undergone exploratory laparotomy with proximal loop ileostomy with primary closure and 6 (13%) were operated by exploratory laparotomy with resection anastomosis.
Results: Mean duration of the stay for patient undergone PC+PL was 10.20 days and for ileostomy it was 18.4 days and for RA + PL it was 18.6 days. Total 37 incidences of complications were found in 45 cases. Among them wound infection was presented in 16 (43%) and burst abdomen presented in 2 (5%) cases. Fecal fistulae, post-operative collection and pneumonitis were present in 4 (11%) cases each.
Conclusion: The overall mortality was found nearly 4 percent in our study. The typhoid ileal perforation should be always treated surgically. There are many operative techniques to deal with but no one is full proof.
Keywords: Ileal perforation; Typhoid fever; Enteric fever; Ileostomy; Resection anastomosis
Introduction
Typhoid fever also known as enteric fever is caused by a gram negative bacteria Salmonella typhi; it is a major public health problem in developing countries of Africa and Asia. The incidence of typhoid in Asia is around 274/100,000 persons per year [1]. India has highest incidence worldwide [2]. This disease is transmitted by faeco-oral route and it exists as an endemic disease, where water supply and sanitation is poor. Around 1% of population up-to the age of 17 years in India yearly suffers once from this disease. The statistical data shows that, there were approximately 1.03 million cases and 421 deaths in 2009 [3], with many more under-reported cases from rural area makes this picture bit serious. With the emergence of multi-drug resistant strains, there are high incidences of morbidity and mortality [4]. Intestinal hemorrhage has been reported between 0.8% to 18%, which is most common complication of typhoid fever, ileal perforation continues to be the most frequent reason behind high morbidity and mortality, especially in remote areas where there is lack of good medical facility [5].
Generally, hemorrhage and perforation occurs at terminal ileum secondary to necrosis of Peyers’ patches [6]. The risk of perforation is higher in males, patients with leucopenia, short duration of disease, emergence of multidrug resistant strains and incomplete antibiotic treatment [7]. The management of typhoid intestinal perforation poses a unique challenge to treating surgeon because of late presentation due to various reasons; late diagnosis, treatment by quacks initially, injudicious use of steroids, poor awareness, poverty, lack of transport facility and poor medical facility [8].
Mortality in cases of perforation is around 9%-22% in developing world, when compared to developed world (0%- 2%). In the past, enteric perforation was considered almost fatal as most surgeon up till 1960 remains with conservative management [9]. 1970 onwards most surgeons favoured surgical intervention in typhoid perforation [10]. Various operative procedure were advocated by different authors such as simple repair of perforation, repair of perforation with ileo-transverse colostomy, primary ileostomy, single layer repair with Omentum patch and resection and anastomosis, two layer closure and tube ileostomy [11].
Even with such a variety of procedure, enteric perforation still has a high rate of morbidity and mortality. The aim of the present study is to study clinical presentations, to evaluate management pattern of typhoid ileal perforation, to determine mortality and morbidity of perforation and to study the reexploration rate and causes of re-exploration and its effect on mortality and morbidity.
Methods
This prospective observational study was conducted in the Departments of Surgery at Surat Municipal Institute of Medical Education & Research, Surat during June 2008 till October 2010. A total 45 patients were included in the study after approval of institutional ethical committee and consent from the participants. Patients of all age group and both sex who presented with acute abdomen, and having the terminal ileal antimesenteric perforation with fever for two weeks were included in this study. The data of each patient was collected on a Performa designed for this study, including demographic details, clinical features, interval between onset of symptoms and hospital admission, operative findings, procedure performed, postoperative complications and duration of stay in hospital.
All the admissions were carried as cases of acute abdomen and were resuscitated with intravenous fluids, nasogastric tube to decompress the stomach and urethral catheter to monitor urine output. Blood complete picture, blood urea, serum electrolytes, abdominal & chest radiographs and abdominopelvic ultrasound were carried out. Bacterial culture from the perforated ulcer, S. Widal test and blood culture were tested within 24 hours of presentation. After hemodynamically stabilizing the patient all cases were operated by exploratory laparotomy and perforation was managed according to site, size of perforation and amount of contamination and condition of bowel. Site and size of perforation was noted and condition of bowel was assessed. According to above findings the perforation was managed.
Cases with less contamination, small perforation and good bowel condition were operated by simple primary closure of the perforation with peritoneal lavage with warm normal saline. Simple primary closure was done in transverse axis, first layer was taken with absorbable suture material (Polyglaction 910) and second layer was taken as interrupted Lambert sutures burying the first layer with silk 2/0. Cases with higher peritoneal contamination and perforation close to ileocecal junction were operated by primary closure of perforation with proximal loop ileostomy.
The cases where large sized perforation and bed bowel condition were managed by resection of involved segment and anastomosis of both ends. At first the 4th layer is taken in continuous interlocking or interrupted manner with silk 3/0 then third layer is taken which is continued as second layer and completed by taking Connell sutures with absorbable material (Polyglactin 910). Then first layer is taken as continuation of fourth layer. Mesenteric gap is also approximated to prevent herniation of contents. In all cases 2 abdominal drains were kept 1 in pelvis and other in Morrisons pouch.
In all cases margins of perforation were trimmed and tissue was taken from the margins and sent for bacterial culture and histopathology examination. The abdomen was closed in single layer with Polypropylene No 1 and skin was closed with Polyamide Black 2/0. The variables studied in the post-operative period were wound infection, wound dehiscence enterocutaneous fistula, residual abscess, mortality, hospital stay. The statistical analysis was done by using Chi-square test and fischer exact test.
Results
In present study, age group ranged from 13-75 years. Minimum age was 13 years and maximum age 75 years. Mean age was 30.91 years. In the present study 41(91%) cases were male while 4 (9%) were female. Male patients are 10 times more affected than the female patient in typhoid ileal perforation. Pain in abdomen is present in almost all 45 cases it was generalized and the next symptoms was vomiting. It was present in 96% case it is followed by fever which was present in 73% cases and rests of the symptoms were distension in 40% cases and diarrhea in 13% cases.
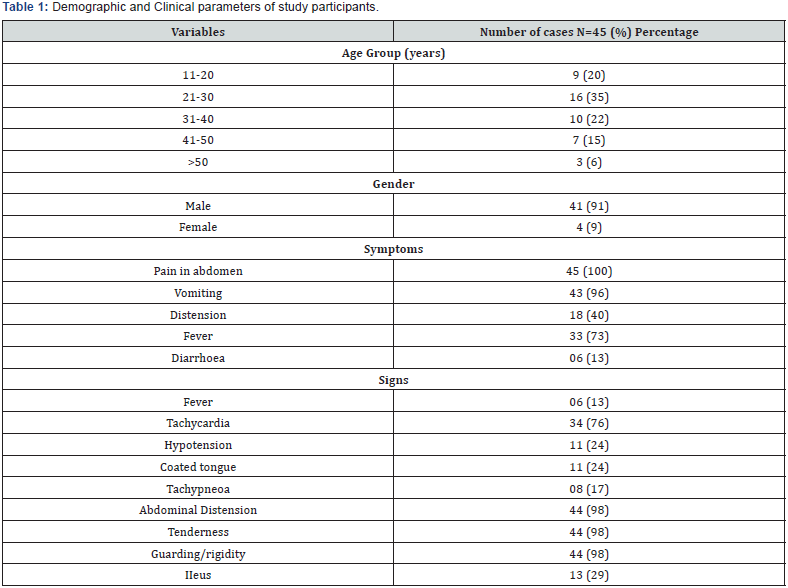


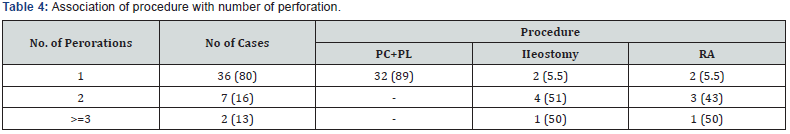
Out of 45 cases, 98% cases showed the abdominal tenderness, guarding and rigidity with abdominal distension. Tachycardia was present in 34 cases (76%) and 11 cases (24%) presented with signs of hypovolemia like hypotension (Table 1). In present study out of 44 cases 40 cases 91% showed the gas under diaphragm on the X ray abdomen standing and 4 (9%) showed the AFL. 1 cases of pregnant patient was not undergone the x-ray examination. Total 23 cases undergone preoperative on USG Abdomen on USG the most consistent finding was various degree of free fluid with internal echoes. Bacterial culture from biopsy specimen was positive in 33 cases (73%). S. Widal was positive in 16 cases (36%) whereas blood culture was positive in 7 cases (16%) (Table 2). All cases had undergone the exploratory laparotomy. Among them, 32 cases (71%) undergone the simple primary closure of the perforation and peritoneal lavage after refreshing the edge. 7 cases (16%) undergone exploratory laparotomy with proximal loop ileostomy with primary closure and 6 (13%) were operated by exploratory laparotomy with resection anastomosis (Table 3 & 4).
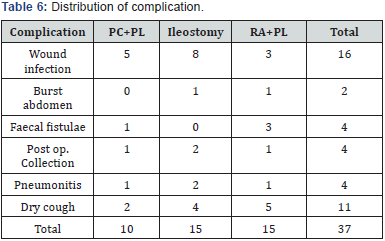
Total of 54 perforations present in 45 cases within 45cm from ileocecal junction out of this 23 perforation found within 21-30cm followed by 19 perforation found within 11-20cm. So, it is suggestive that ileal perforation in typhoid most commonly involved distal 1/3rd of ileum (Table 5). The study showed the hospital stay ranging from 7 days to 45 days. Mean duration of the stay for patient undergone PC+PL was 10.20 days and for ileostomy it was 18.4 days and for RA + PL it was 18.6 days. According to Table 6, total 37 incidence of complications were found in 45 cases. Among them wound infection was presented in 16 (43%) and burst abdomen presented in 2 (5%) cases. Fecal fistulae, post-operative collection and pneumonitis were present in 4 (11%) cases each (Table 6).

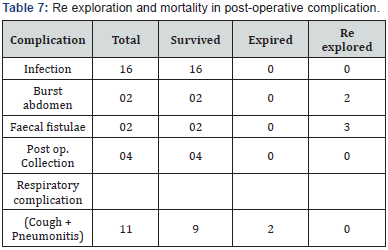
Out of total 5 cases (11%) which were re-explored, 2 had burst abdomen and 3 had faecal fistulae on the exploration 2 cases showed the new perforation 15cm proximal and 10cm distal to previous perforation and 1 case showed the anastomotic leak and in 2 cases of localized abscess were reported. There was no mortality present in above complications except respiratory complication in which 2 cases were expired due to pneumonitis (Table 7).
Discussion
Typhoid perforation is common in the 2nd and 3rd decades of life [12]. In present study age group were ranged from 13- 75 years in 45 cases. Maximum age group affected was in range of 21-30 years followed by 31-40 years. Male: Female ratio is 10.2:1. That is more than the ratio of 5.25:1 [13] and 4:1 [14] reported by other studies. This is due to the fact that males possibly have more exposure for infection. So, the disease and its complication as perforation are seen commonly in adult male.
Abdominal pain, fever and signs of peritonitis were most frequent symptoms and signs in this study, as also shown in various studies [15,16]. Gas under diaphragm in x-ray abdomen standing is an important finding in any intestinal perforation and helpful in diagnosis. Our study demonstrated free gas under the diaphragm in around ninety percent (91%) of cases which is consistent with other studies [17,18]. Free gas under the diaphragm on x-ray film readily clinches the diagnosis, but its absence does not exclude the diagnosis if peritoneal signs are present. In our study, 23 cases undergone preoperative on USG Abdomen on USG the most consistent finding was various degree of free fluid with internal echoes. A study shows that abdominal USG was superior to plain radiographs in the diagnosis of free intra-peritoneal air [19].
There is wide range of frequency of widal positivity in various studies. Widal test shown positive in 46.1% of patients with typhoid perforation by Santillana M [20], 30% by Kaul BK [21] and 88% of cases by Vaidyanathan S [22]. In our study serum widal test was found positive in 36% of cases. In our study, all the perforation was found within 2 feet of terminal ileum. In contrary to it, it was reported as 87% and 13% by Beniwal US [23].
In the present study, total 37 incidence of complications were found in 45 cases. Among them wound infection was presented in 16 (43%) and burst abdomen presented in 2 (5%) cases. Fecal fistulae, post-operative collection and pneumonitis were present in 4 (11%) cases each. Typhoid perforations are associated with a high morbidity rate with literature reports between 24.5% and 81%. It was reported overall complication rate of 51.6% [20]. In the present study, fecal fistula developed in 11% patients, which was almost similar to 10% as reported by Khan SH et al. [17] and 8% as reported by Talwar S [24]. Overall mortality is seen in 4.44% patients in this study, which was significantly low as compared with various other studies [15,25].
In present study, Mean duration of the stay for patient undergone PC+PL was 10.20 days. Average hospital stay of the patients was longer in Resection anastomosis (18.6 days) than Ileostomy (18.4 days) again due to its complication related to formation of fecal fistula. This finding was similar to finding of study done by Talwar et al. [24]. In which the average hospital stay of the patients was slightly longer in case of ileostomy (16.5 days) in comparison with other procedures (15 days).
Conclusion
The typhoid perforation still carries high morbidity and mortality. The overall mortality was found nearly 4 percent in our study. The typhoid ileal perforation should be always treated surgically. There are many operative techniques to deal with but no one is full proof. Regardless of the operative techniques, surgery within 24 hours with adequate and aggressive resuscitation is a way to decrease morbidity and mortality.
References
- Crump JA, Luby SP, Mintz ED (2004) The global burden of typhoid fever. Bull World Health Organ 82(5): 346-353.
- Siddiqui FJ, Rabbani F, Hasan R, Nizami SQ, Bhutta ZA (2006) Typhoid fever in children: some epidemiological considerations from Karachi, Pakistan. Int J Infect Dis 10(3): 215-222.
- Govt. of India (2010) National health profile 2009, DGHS, Ministry of Health and Family Welfare, India.
- WHO (2008) Weekly Epidemiological Record (WER). 93(15): 185-200.
- Osifo OD, Ogiemwonyi SO (2010) Typhoid ileal perforation in children in Benin city. African Journal of Paediatric Surgery 7(2): 96-100.
- Hosoglu S, Aldemir M, Akalin S, Geyik MF, Tacyildiz IH, et al. (2004) Risk factors for enteric perforation in patients with typhoid Fever. Am J Epidemiol 160(1): 46-50.
- Kotan C, Kosem M, Tuncer I, Kisli E, Sonmez R, et al. (2000) Typhoid intestinal perforation: Review of 11 cases. Kolon Rektum Hast Derg 11: 6-10.
- Atamanalp SS, Aydinli B, Ozturk G, Oren D, Basoglu M, et al. (2007) Typhoid intestinal perforations: twenty-six year experience. World J Surg 31(9): 1883-1888.
- Huckstep RL (1960) Recent advanced in surgery of typhoid fever. Ann Roy Coll Surg Engl 26: 207-280.
- Kim JP, Oh SK, Jarret F (1975) Management of ideal perforation due to typhoid fever. Ann surg 181(1): 88-91.
- Singh S, Singh K, Grover AS, Kumar P, Singh G, et al. (1995) Two-layer closure of typhoid ileal perforations: a prospective study of 46 cases. Br J Surg 82(9):1253.
- Olurin EO, Ajavi OO, Bohrer SP (1972) Typhoid perforations. J Roy Coll Surg Edinb 17: 353-363.
- Swadia ND, Trivedi PM, Thakkar AM (1979) Problem of enteric ileal perforation. Indian J Surg 41: 643-651.
- Adesunkanmi ARK, Ajao OG (1997) Prognostic factors in Typhoid ileal perforation: a prospective study in 50 patients. JR Coll Surg Edinb 42(6): 395-399.
- Adesunkanmi ARK, Badmas TA, Fadiora FO, Agbakwuru EA (2005) Generalised peritonitis secondary to typhoid ileal perforation: assessment of severity using modified APACHE II score. Indian Journal of Surgery 67(1): 29-33.
- Chatterjee H, Jagdish S, Pai D, Satish N, Jayadev D, et al. (2001) Changing trends in outcome of typhoid ileal perforations over three decades in Pondicherry. Trop Gastroentoral 22(3): 155-158.
- Khan SH, Aziz SA, Ul Haq MI (2011) Perforated peptic ulcers: A review of 36 Cases. Professional Med J 18(1): 124-127.
- Lee CW, Yip AW, Lam KH (1993) Pneumogastrogram in the diagnosis of Perforated peptic ulcer. Aust N Z J Surg 63(6): 459-461.
- Chen SC, Yen ZS, Wang HP, Lin FY, Hsu CY, et al. (2002) Ultrasonography is superior to plain radiography in the diagnosis of pneumoperitonium. Br J Surg 89(3): 351-354.
- Santillana M (1991) Surgical complications of typhoid fever: enteric perforation. World J Surg 15(2): 170-175.
- Kaul BK (1975) Operative management of typhoid perforation in children. Int Surg 60(8): 407-410.
- Vaidyanathan S (1986) Surgical management of typhoid ileal perforation. Ind J Surg 335-341.
- Beniwal US, Jindal D, Sharma J, Jain S, Shyam G (2003) Comparative study of operative procedures in typhoid perforation. Indian Journal Surg 65(2): 172-177.
- Talwar S, Sharma RK, Mittal DK, Prasad P (1997) Typhoid enteric perforation. Aust N Z J Surg 67(6): 351-353.
- Singh KP, Singh K, Kohli JS (1991) Choice of surgical procedure in typhoid perforation: Experience in 42 cases. J Indian Med Assoc 89(9): 255-256.






























