Contemporary Tendencies in Surgical Treatment and Biopsy of Sentinel Lymph Nodes in Malignant Melanoma of the Skin
Strahil Strashilov1, Veselin Kirov2, Angel Yordanov3* and Vasil Nanev4
1Department of Plastic Restorative, Reconstructive and Aesthetic Surgery, Europe
2Department of Oncodermatology, University Hospital “Dr. Georgi Stranski”-Pleven, Europe
3Clinic of Gynecologic Oncology, University Hospital “Dr. Georgi Stranski”-Pleven, Europe
4Department of Surgical Oncology, Medical University Pleven, Europe
Submission: September 24, 2017; Published: October 05, 2017
*Corresponding author: Angel Yordanov, Clinic of Gynecologic Oncology, University Hospital "Dr. Georgi Stranski”-Pleven, Bulgaria, Europe, Tel: 359887 671520; Email: angel.jordanov@gmail.com
How to cite this article: Strahil S, Veselin K, Angel Y, Vasil N. Contemporary Tendencies in Surgical Treatment and Biopsy of Sentinel Lymph Nodes in Malignant Melanoma of the Skin. Open Access J Surg. 2017; 6(2): 555685. DOI: 10.19080/OAJS.2017.06.555685
Abstract
The malignant melanoma is a fairly rare, but very malignant tumor, emanative from epidermal melanocytes, that affects the skin in above 95% of cases. Unlike other tumors, it is encountered in younger age and can metastasize in early stages of the disease. This tumor is with highest rate of morbidity increase - 5% of newly diagnosed oncological conditions in men and 6% in women. The surgical treatment includes biopsy of the primary lesion, sentinel biopsy of regional lymph nodes with possible following lymph disection, wide radical excision of the primary site and surgical removal of distant methastases in the advanced stages of the disease
Keywords: Malignant melanoma of the skin; Contemporary surgical treatment; Sentinel lymph biopsy
Introduction
The malignant melanoma (MM) is a fairly rare, but very malignant tumor, originating from the epidermal melanocytes. Its highest incidence is in the caucasian population of Australia and New Zealand, where the morbidity is above 40/100 000 people per year. In the USA its 10/100000, in Western Europe's women it's 12/100 000, while for men it's 7/100000. For Bulgaria the morbidity is 3.0-3.5/100 000. Unlike other tumors, it affects younger age and can metastasize in early stages of the disease. MM is the tumor with highest rate of morbidity increase - 5% of newly diagnosed oncological conditions in men and 6% in women [1,2].
Contemporary surgical treatment of MM of the skin, including sentinel biopsy of regional lymph nodes, is very important and is a main part of the complex treatment, generally defining the outcome of the disease. The main components of the complex treatment are:
a) biopsy of the primary lesion (incisional or excisional)
b) pathological examination of the biopsy material with description of the thickness of the tumor based on Breslow and the invasion depth, based on Clark
c) radical reexcision of the tumor bed
d) performing sentinel biopsy of the regional lymph nodes if indicated
e) lymph disection of regional lymph nodes if indicated
f) histopathological serial immunohistochemical analysis of sentinel lymph nodes and/or usual one for the rest of the lymph nodes [3-5]
g) staging the disease with the TNM classification
h) undertaking adjuvant non-surgical treatment, if needed
i) observation
j) Exposition
A. Biopsy of the primary lesion: it can be incisional, where a piece of bigger tumors is taken, or excisional, where the melanoma is removed with visibly healthy halo of unchanged skin with size between 1 and 3 mm. The reason to not go straight for radical excision of the tumor site is that it would cut off lymph pathways, which directly drain the location, and that would vitiate the biopsy of the sentinel lymph node, which is with a specific area of lymph drainage.
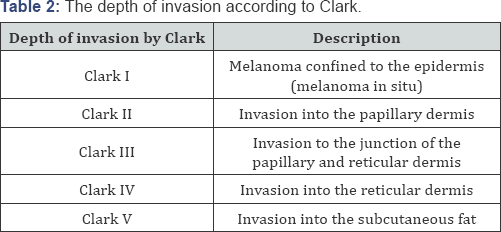
B. Pathological examination of the biopsy material: it gives a description of the tumor thickness according to Breslow scale (Table 1) and of the depth of invasion according to Clark (Table 2) [6].

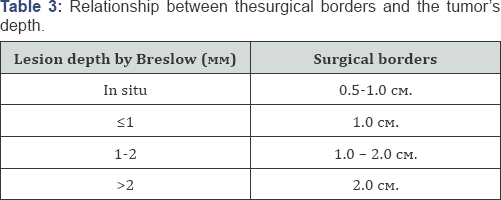
C. Radical reexcision of the tumor bed: it is performed 4-6 weeks after diagnosing [7]. Part of the skin in the area around the primary tumor is surgically removed after performing a sentinel biopsy (if such is done). The distance of the reexcisional line on both sides from the cicatrix from the previous biopsy of the melanoma or from itself is correlative to the tumor's depth, established with the pathological examination (Table 3) [8-13].
D. Performing sentinel biopsy of the regional lymph nodes: According to the data from the most recent and wide studies (MSLT 1 and 2) sentinel biopsy of lymph nodes is a foundation in the complex treatment of the disease. They prove mainly four things: first - the result of the biopsy is one of the strongest prognostic factors, second - the execution of total lymphadenectomy after positive sentinel biopsy in patients with some thin, all intermediate and thick melanomas, significantly increases the survival rate in good health, third - the result of the biopsy is base for an effective adjuvant therapy and fourth - sentinel biopsy is very gentle surgical intervention [14,15]. Sentinel biopsy is the removal of the first lymph node(s) that receive the methastases of a malignant process. Histological examination of that node gives accurate prognosis about the affecting of the remaining lymph node chain [16,17]. Introducing biopsy of the sentinel lymph nodes in cases of malignant melanoma of the skin is done by Donald Morton et al. in 1992 to avoid common postoperative complications of the previously routinely used elective lymph disection and the lack of effect by it on negative lymph nodes [18,19].
i. Indications for performing sentinel biopsy:
a. clinically negative regional lymph nodes
b. tumor thickness over 1 mm
c. for tumors between 0.76 and 1 mm, performing the intervention must be discussed and it must be precise
d. for tumors with thickness under 0.75 mm sentinel lymph node biopsy is performed only by exception and in the presence of additional factors, such as tumor ulcerations, higher mitotic index, young age, etc [20-23].
ii. Contraindications against performing sentinel biopsy:
a. most tumors with thickness under 0.75mm
b. clinically and puncture-biopsy positive regional lymph nodes
c. previous lymph biopsy of that region
d. performed wide-bordered primary site biopsy
e. lack of a team of prepared specialists [24].
I. Technique for performing sentinel lymph node biopsy
Nowadays we use the following methodology: biopsy of sentinel lymph nodes in case of MM is performed after the initial injection of radiopharmaceutical 99Tc sulfur colloid at 4 intradermal spots around the scar of a previous diagnostic excision of the pathological lesion in doses of 0.28 to 10 |iCi. After testing the patient in a gamma camera, showing the regional lymph drain, existance of possible intransitive lymph nodes, localisation and number of sentinel lymph nodes, a lymphoscintigraphic map is made [18,25-28]. Next, in the surgery room, a lymphotropic dye Patent Blue V is injected in 1 ml dose in roughly 10 intradermal locations on the same place. After 6 to 10 minutes of waiting time, a surgical incision is done at the places, marked by the lymphoscintigraphic map, and the search for a sentinel lymph node begins.
A sentinel lymph node is considered one that is colored in blue and topographically fits on the lymphoscintigraphic map. That node is removed after disturbing the afferent and efferent lymph vessels and is then sent for histological search of methasthases [29,30]. By this method we reached 98% success in finding the sentinel lymph node. There is another widely used method for sentinel biopsy - after doing the lymphoscintigraphic map, a search for the lymph node is performed with manual intraoperative gamma camera. There is also an option to use just the latter pre- and intraoperative, without making a lymphoscintigraphic map [31]. The success rate of those methods is similar to ours, but our method is significantly cheaper and economically efficient, and therefore a method of choice.
E. Lymph disection of regional lymph nodes: it is the standart surgical removal of the corresponding lymph nodes, if those are affected by metastatic process, which is found histologically or citologically after a sentinel biopsy, clinical or apparatus suspicion [32]. According to the data from the most recent and wide studies on sentinel biopsy and lymph disection in case of MM of the skin (MSLT 1 and 2), performing the disection immediately after finding a positive sentinel lymph node increases the survivability of patients in good health, compared to those, where lymph disection is performed after the clinical finding of metastases in the lymph nodes [14,15].
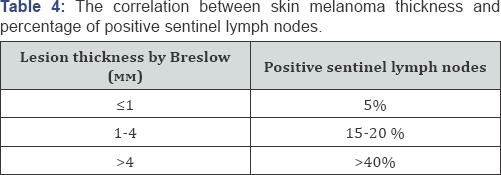
F. Histopatological examination of the removed sentinel and other lymph nodes: after removing the sentinel lymph nodes they are tested with serial section immunohistochemistry with markers, specific for the melanoma cells (S100, Melan A, HMB-45) for the presence of metastases, micrometastases or isolated tumor cells [33-36]. The correlation between skin melanoma thickness and percentage of positive sentinel lymph nodes is shown in table 4 [37]. Lymph nodes, removed by disection, are also subjected to standart or immunohistochemical histopatological examination for metastases.
G. Disease staging: it is performed after all said procedures, with the TNM system, in 4 clinical stages. It is a very important step in the treatment of malignant melanoma of the skin, because the success of the following treatment depends on it.
H. Adjuvant treatment: all other therapies are included here, besides the surgical (immunotherapy, target therapy, vaccinotherapy, chemotherapy, radiotherapy, etc)
I. Observation: it's a very important part of the treatment of malignant melanoma of the skin. It's periodical and constitutes of all clinical, laboratory and instrumental tests of the patients with found disease. If there are deviations in any of them, corresponding additional surgical and/or non- surgical treatment is included. The additional surgical treatment includes removal of distant metastases from different organs, local recidives, etc.
Conclusion
Success in treating malignant melanoma of the skin is correlevant to following most contemporary tendencies. Contemporary surgical treatment is primary in the total treatment of MM. The result of sentinel lymph biopsy is one of the strongest prognostic factors. Performing total lymphadenectomy after positive sentinel biopsy in patients with some thin, all intermediate and thick melanomas significantly improves survival in good health. The result of sentinel lymph node biopsy is base for effective adjuvant therapy. Sentinel biopsy is a very gentle surgical intervention.
References
- БaЛaбaOBa M, CЪЛaeBa M, MaИnrHeH MeГЛHOM, MeДИHФo (2016) 04: 24-29
- Fitzpatrick's Color Atlas and Synopsis of Clinical Dermatology Sixth Edition Ebook.
- Coit DG, Andtbacka R, Bichakjian CK, Dilawari RA, Dimaio D, et al. (2009) Melanoma J Natl Compr Canc Netw 7: 250-275.
- (2008) Australian Cancer Network New Zealand Guidelines Group Cancer Council Australia New Zealand Ministry of Health. Clinical practice guidelines for the management of melanoma in Australia and New Zealand evidence-based best practice guidelines. Sydney N.S.W Australian Cancer Network.
- Rigel DS, Friedman R, Kopf AW (1985) Surgical margins for the removal of dysplastic nevi. J Dermatol Surg Oncol 11: 745.
- Balch CM, Soong SJ, Gershenwald JE, Thompson JF, Reintgen DS, et al. (2001) Prognostic factors analysis of 17,600 melanoma patients Validation of the American Joint Committee on Cancer melanoma staging system. Journal of clinical oncology 19(16): 3622-3634.
- Claus Garbe, Ketty Peris, Axel Hauschild, Philippe Saiag, Mark Middleton, et al. (2016) On behalf of the European Dermatology Forum (EDF) the European Association of Dermato-Oncology (EADO) and the European Organisation for Research and Treatment of Cancer (EORTC) Diagnosis and treatment of melanoma European consensus-based interdisciplinary guideline e Update. European Journal of Cancer 63: 201-217.
- Lens MB, Nathan P, Bataille V (2007) Excision margins for primary cutaneous melanoma updated pooled analysis of randomized controlled trials. 142: 885-893.
- Veronesi U, Cascinelli (1991) N Narrow excision (1-cm margin) a safe procedure for thin cutaneous melanoma. 126: 438-441.
- Veronesi U, Cascinelli N, Adamus J, Balch C, Bandiera D, et al. (1988) Thin stage I primary cutaneous malignant melanoma. Comparison of excision with margins of 1 or 3 cm. N Engl J Med 318:1159-1162.
- McKenna DB, Lee RJ, Prescott RJ, Doherty VR (2004) A retrospective observational study of primary cutaneous malignant melanoma patients treated with excision only compared with excision biopsy followed by wider local excision. Br J Dermatol 150: 523-530.
- Cascinelli N (1998) Margin of resection in the management of primary melanoma. Semin Surg Oncol 14: 272-285.
- Khayat D, Rixe O, Martin G, Soubrane C, Banzet M, et al. (2003) Surgical margins in cutaneous melanoma (2 cm versus 5 cm for lesions measuring less than 2.1-mm thick). Cancer 97(8): 1941-1946.
- Spillane A, Read R, Thompson J (2015) Sentinel node biopsy should be the standard of care for patients with intermediate and thick melanomas. Aust Fam Physician 44(8): 604-606.
- Morton D (2012) On behalf of the MSLT Study Group Over view and update of the phase III Multicenter Selective Lymphadenectomy Trials (MSLT-I and MSLT-II) inmelanoma. Clin Exp Metastasis 29(7): 699-706.
- Balch CM, Gershenwald JE, Soong SJ (2009) J Clin Oncol 27(36): 61996206.
- Sondak VK, Zager JS, Messina JL, Thomas JM (2007) Sentinel lymph node biopsy as the standard of care for cutaneous melanoma. Clin Adv Hematol Oncol 5(6): 483-490.
- БaЙЧeB Г. БИoΠИяa Ha ceHTИHeЛHИ ЛИmФИh bЪзЛТ ПpИ MaЛИГHeH MeЛaHOM; My surgery.bg; 28.09.2011
- Morthon DL, DR Wen, Wong JH ,economou, et al (1992) Technical details of Intraoperative lymphatic mapping for early stage melanoma. Arch Surg 127(4): 392-399.
- Gershenwald JE, Mansfield PF, Lee JE, Ross MI (2000) Role for lymphatic mapping and sentinel lymph node biopsy in patients with thick (> or = 4 mm) primary melanoma. Ann Surg Oncol 7(2): 160-165.
- Ferrone CR, Panageas KS, Busam K, Brady MS, Coit DG (2002) Multivariate prognostic model for patients with thick cutaneous melanoma: importance of sentinel lymph node status. Ann Surg Oncol 9(7): 637-645.
- Gajdos C, Griffith KA, WongSL, JohnsonTM, ChangAE, et al. (2009) Is there a benefit to sentinel lymph node biopsy in patients with T4 melanoma. Cancer 115(24): 5752-5760.
- Gutzmer R, Satzger I, Thoms KM, Volker B, Mitteldorf C, et al. (2008) Sentinel lymph node status is the most important prognostic factor for thick (> or = 4 mm) melanomas. J Dtsch Dermatol Ges 6(3): 198-203.
- (2007) National Comprehensive Cancer Network. Melanoma: Clinical Practice Guidelines in Oncology. National Comprehensive Cancer Network.
- Morton DL, Thompson JF, Essner R, Elashoff R, Stern SL, et al. (1992) Validation of the accuracy of intraoperativelymphatic mapping and sentinel lymphadenectomy for earlystagemelanoma: a multicenter trial. Ann Surg 230(4): 453-465.
- Mattsson J, Bergkvist L, Abdiu A, Aili Low JF, Naredi P, et al. (2008) Sentinel node biopsy in malignant melanoma:Swedish experiences 1997-2005. 47(8): 1519-1525.
- Rossi CR, De Salvo GL, Trifiro G, Mocellin S, Landi G, et al. (2006) The impact of lymphoscintigraphy technique on theoutcome of sentinel node biopsy in 1,313 patients withcutaneous melanoma: an Italian multicentric study (SOLISMIMI). J Nucl Med 47: 234-241.
- Testori A, De Salvo GL, Montesco MC, Trifiro G, Mocellin, et al. (2009) Clinical considerations on sentinel node biopsyin melanoma from an Italian multicentric study on 1,313patients (SOLISM-IMI). Ann Surg Oncol 16(7): 2018-2027.
- Essner R (2003) Surgical treatment of malignant melanoma. Surg Clin N Am 83(1): 109-156.
- Annette H, Chakera, Birger Hesse, Zeynep Burak, James R, et al. (2009) EANM-EORTC general recommendations for sentinel node diagnostics in melanoma. Spinger 36(10): 1713-1742.
- Marcelo T, Sapienza, Marcia G M, Tavares, Irene S Endo, Guilherme C Campos Neto, et al. (2004) The role of sentinel node mapping in malignant melanoma: experience with 99mTc-phytate and a review of the literature 79(2).
- Morton DL, Wanek L, Nizze JA, Elashoff RM, Wong JH (1991) Improved long-term survival after lymphadenectomy of melanom metastatic to regional nodes. Analysis of Prognostic factorsin 1134 patients from the John Wayne Cancer Clinic. Ann Surg 214(4): 491-499.
- Byron E Wright, Randall P Scheri, Xing Ye, Mark Faries, Roderick R Turner, et al. (2006) The Prognostic importance of sentinel lymph node biopsy in patients with thin melanoma. Annals of Surgical Oncology 13(7): 927-932.
- Carson KF, Wen DR, Li PX, Lana AM, Bailly C, et al. (1996) Nodal nevi and cutaneous melanomas. Am J Surg Pathol 20(7): 834-840.
- Ohsie SJ, Sarantopoulos GP, Cochran AJ, Binder SW (2008) Immunohistochemical characteristics of melanoma. J Cutan Pathol 35: 433-444.
- Trejo O, Reed JA, Prieto VG (2002) Atypical cells in human cutaneous re-excision scars for melanoma express p75NGFR, C56/N-CAM and GAP-43: evidence of early Schwann cell differentiation. J Cutan Pathol 29(7): 397-406.
- Lens MB, Dawes M, Newton-Bishop JA, Goodacre T (2002) Tumour thickness as a predictor of occult lymph node metastases in patients with stage I and II melanoma undergoing sentinel lymph node biopsy. Br J Surg 89(10): 1223-1227.






























