Case Report: 58 yr. Old Male Patient Known Case of DM, HT, With Fever for Two Days
Sushila Ladumor1* and Adham Darweesh2
1Consultant Radiologist, Clinical Imaging Department, Hamad Medical Corporation, HGH, Doha, Qatar, Assistant Professor in Clinical Radiology, Weil Cornel Medical College, Qatar (WCMC-Q)
2Senior Consultant Radiologist, Clinical Imaging Department, Hamad Medical Corporation, HGH, Doha, Qatar, Assistant Professor in Clinical Radiology,
Submission: September 12, 2017; Published: September 19, 2017
*Corresponding author: Sushila Ladumor B, Consultant Radiologist, Clinical Imaging Department, Hamad Medical Corporation, HGH, Doha, Qatar, Assistant Professor in Clinical Radiology, Weil Cornel Medical College, Doha, Qatar (WCMC-Q), E-mail: drsbladumor@yahoo.com
How to cite this article: Sushila L, A Darweesh. Case Report: 58 yr. Old Male Patient Known Case of DM, HT, With Fever for Two Days. Open Access J Surg. 2017; 6(1): 555678. DOI: 10.19080/OAJS.2017.06.555678
Abstract
Pneumonia is one of the major infectious diseases responsible for significant morbidity and mortality throughout the world. Community- acquired pneumonia (CAP) is a serious illness with a significant impact on individual patients and society as a whole. Community acquired pneumonia (CAP) is a clinical term to refer to pneumonia acquired outside of the hospital setting. Streptococcus pneumoniae is considered the most common bacterial etiology. Pulmonary infections are the most common reason for obtaining a chest radiograph. Chest radiography with clinical history and examination is usually enough to reach the diagnosis of CAP, whereas computed tomography is required to suggest specific pathogens and to discriminate from other noninfectious diseases. Mycoplasma pneumoniae pneumonia, tuberculosis, Pneumocystis carinii pneumonia (PCP) and some cases of viral pneumonia sometimes show specific imaging findings. There are few tips to effectively make use of imaging examinations in the diagnosis and management of CAP.
Keywords: Community-acquired pneumonia; Computed tomography; Infection, Pneumonia, Lung disease
Abbreviations: CAP: Community-acquired pneumonia; CT scan: Computed tomography
Clinical History
58 yr. old male patient known case of DM, HT, came with fever for two days (Figure 1).
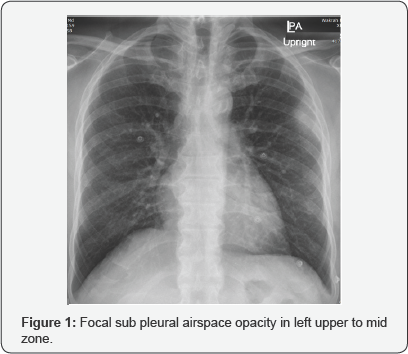
Impression: of Figure 1
Focal sub pleural airspace opacity in left upper to mid zone.
Need to compare with previous exam if available. No previous exam
D/D of focal air space opacity
Consolidation,
Focal lung nodule,
Pleural based nodule
Sub pleural mass
In view of clinical history of fever, likely airspace consolidation, for treatment and follow-up.
B. Patient did not follow advice of treating Physician and did not take any medicine. Came back after 6days with fever and cough
Impression: of Figure 2
Interval significant increase in airspace disease in left lung, and development of minimal left pleural effusion.
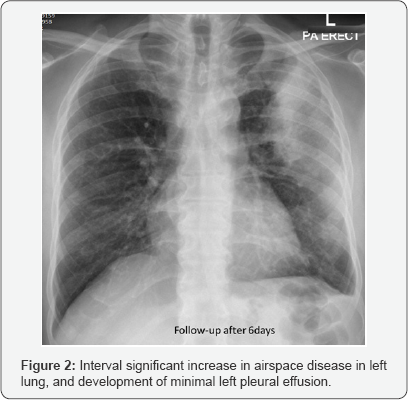
More in favor of infection in view of short term increase.
Diagnosis: From Physician note
Community acquire pneumonia as no history of hospitalization as well no history of any contact with tuberculous patient.
C. CT recommended to exclude underlying pathology /further evaluation considering patient age (Figure 3).
Impression: of Figure 3
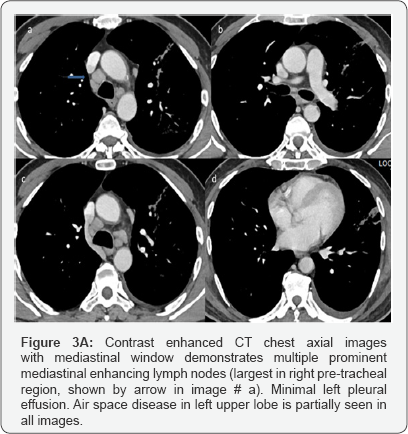
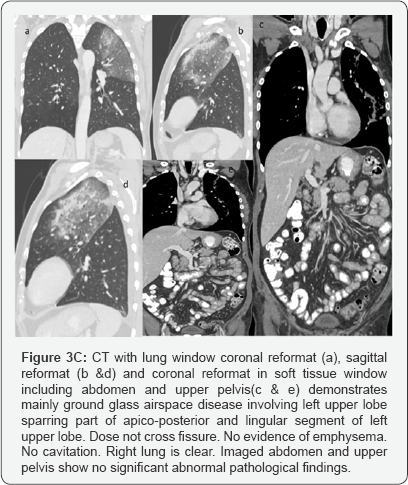
CT with Contrast done after 4days of second X-ray chest.
Large area of consolidation seen involving left upper lobe with central area of ground glass opacity surrounded by rim of more density mainly at anterior aspect representing incomplete reversed halo sign.
Multiple prominent enhancing mediastinal lymph nodes. Minimal left pleural effusion. Right lung is clear.
In short term worsening and in view of history, likely community acquired pneumonia.
No mass.
Recommendation
Follow-up after antibiotic.
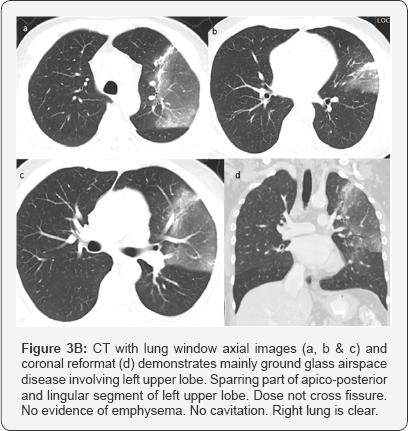
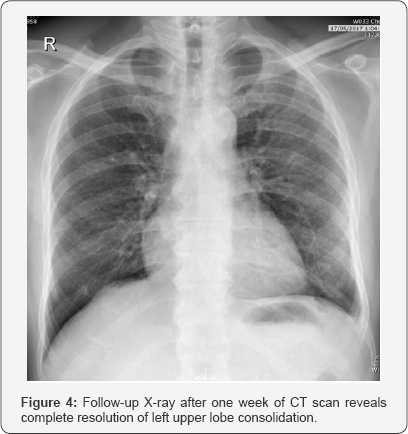
Patient given Antibiotics after second X-ray and follow-up x-ray after one week of CT recommended (Figure 4).
Introduction
The etiology of CAP varies widely according to the different analysis. It is influenced by the geographic area, the population studied and the diagnostic methods used. Community-acquired pneumonia (CAP) is defined as infectious pneumonia that is acquired in the social community [1]. This term is opposed to hospital-acquired pneumonia (synonym for nosocomial pneumonia), which is infected in the hospital (24 h later after the hospitalization) [2]. The third term, nursing home acquired pneumonia that is acquired in the nursing home, has recently been proposed, which has intermediate characteristics between community-acquired and hospital-acquired pneumonia [3] . The pathogens of CAP include a wide variety of microbes, including not only ordinary bacteria but also mycobacteria, viruses or fungi [3]. They manifest as pneumonia in various forms, and their imaging findings are often nonspecific [3]. However, characteristic imaging findings of several pathogens are sometimes suggestive of the diagnosis of specific pneumonia (5). In addition, imaging examinations sometimes offer clues for the differentiation between infectious pneumonia and noninfectious diseases. The chest radiograph is often regarded as the reference standard for the diagnosis of CAP. CT is used to characterize complex pneumonias, look for complications, or reveal underlying disease within lung or mediastinum. CT can also detect some pneumonias that are not visible on chest radiograph. CT with contrast plays an important role in differentiating lung abscess from empyema.
Imaging Findings of CAP
Patterns of imaging findings.
CAP has classically been divided mainly into three distinctive patterns on imaging examinations (1).
i. Consolidation (alveolar/lobar pneumonia)
ii. Peribronchial nodules (bronchopneumonia)
iii. Ground-glass opacity (GGO) [4].
iv. The fourth, a unique uncommon pattern of CAP is random nodules, suggestive of hematogenous pulmonary infection or granulomatous infection.
In fact, many pathogens can cause pneumonia with more than one pattern. In addition, consolidation, peribronchial nodules and GGO can often coexist in a case of pneumonia although one of these findings usually predominates. Virulence, amount or size of pathogens, affinity to certain cells, and immune response of hosts may relate to the different manifestations of CAP on imaging examinations.
a. Consolidation predominant pattern (alveolar/ lobar pneumonia)
Consolidation predominant pneumonia is referred to as alveolar pneumonia. When it affects almost an entire lung lobe, it is called "lobar pneumonia". This consolidation is believed to be formed by the spread of inflammation through pores of Kohn or canals of Lambert at the periphery of the lung. Thus, it usually appears in a nonsegmental consolidation in the early stage of disease. Most bacterial pneumonias exemplified by Streptococcus and Klebsiella pneumonia appear in consolidation predominant pattern.
Discussion
There is no imaging finding that is 100% specific for infectious pneumonia. Consolidation and GGO are virtually nonspecific. However, peribronchial nodules, especially tree-in-bud appearance are fairly specific for infection [3]. When viewed with CT, consolidation, GGO and peribronchial nodules are coexistent in most cases of infectious pneumonia. Therefore, peribronchial nodules can often be a diagnostic clue for infectious pneumonia. Imaging examinations also play a complementary role for the evaluation of treatment effects of antibiotics although treatment effects may be determined based solely on clinical findings [1]. It is generally difficult to determine specific pathogens of infectious pneumonia based only on the imaging findings. However, as characteristic imaging findings of several pathogens have been reported, they may help choose subsequent examinations or first antibiotics.
Detailed clinical assessment is the first step for the diagnosis of CAP. Patients with CAP usually complain of fever, cough, sputum, difficulty breathing or chest pain [1,5]. Chest pain is usually associated with pleuritic. Heckerling et al. [1] proposed 5 criteria that suggest infectious pneumonia: temperature > 37.8 °C, pulse > 100 beats/min, crackles, decreased breath sounds and the absence of asthma. According to their nomogram for determining the probability of having pneumonia, when assuming a 10% prevalence of pneumonia in the patient population, if these five criteria are met, the probability of pneumonia reaches 70% [1].
When clinical findings are suggestive of CAP, blood test, various tests for determining the causative pathogen and chest radiography are performed. Laboratory data usually show an elevation of white blood cell count, C reactive protein and erythrocyte sedimentation rate. Tests for pathogens include sputum culture, blood culture (in case of suspected sepsis), various antigen tests including pharyngeal swab test for influenza viruses or urine antigen tests for Legionella pneumophila and Streptococcus pneumoniae, antibody tests, gram stain, paired serum tests and cold agglutination test.
Thoracic malignancy, atypical infection, and other nonmalignant pulmonary diseases such as atypical infection, organizing pneumonia, sarcoidosis, and bronchopulmonary sequestration may appear similar to community-acquired pneumonia on chest radiography (3). Although practice varies, many clinicians and radiologists recommend follow-up chest radiography to confirm clearing of a radiographic opacity suspected to represent community-acquired pneumonia. The rationale for this practice is to ensure that the patient's symptoms and radiographic findings are in fact due to community-acquired pneumonia rather than another disease (4).
Air Bronchogram
Air bronchogram refers to the phenomenon of air-filled bronchi (dark) being made visible by the opacification of surrounding alveoli (grey/white). It is almost always caused by a pathologic airspace/alveolar process, in which something other than air fills the alveoli. Air bronchograms will not be visible if the bronchi themselves are opacified (e.g. by fluid) and thus indicate patent proximal airways. Air bronchograms can be seen in:
i. Pulmonary consolidation
ii. Pulmonary edema: especially with alveolar edema
iii. Non-obstructive atelectasis
iv. Severe interstitial lung disease
v. Neoplasms: bronchioloalveolar carcinoma; pulmonarylymphoma
vi. Pulmonary infarct
vii. Pulmonary hemorrhage
viii. Rarely normal expiration
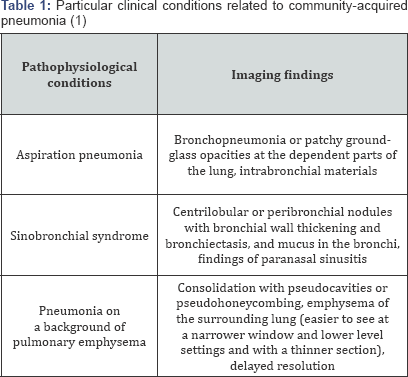
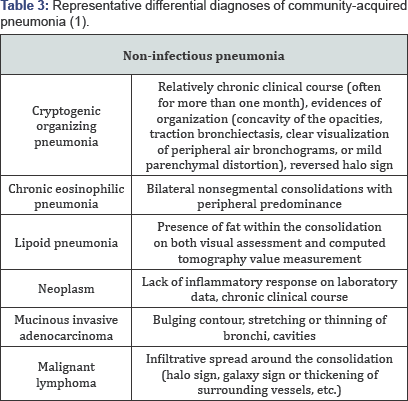
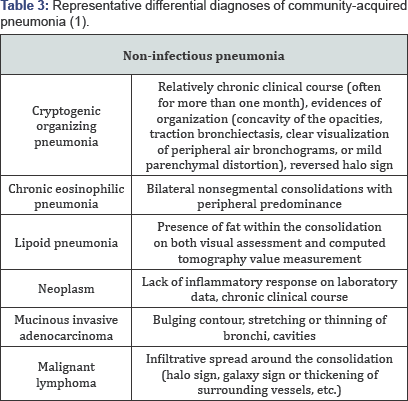
Air bronchograms that persist for weeks despite appropriate antimicrobial therapy should raise the suspicion of a neoplastic process. CT may be planned in such cases (Tables 1-3).
Conclusion
Imaging findings of CAP are varied and often nonspecific. However, some characteristic findings are sometimes suggestive of specific pathogens. In addition, imaging examinations, especially CT, can offer clues to the differentiation between infectious pneumonia and noninfectious diseases. To accomplish this differentiation, familiarity with imaging characteristics of CAP as well as those of noninfectious diseases is indispensable. Chest radiography is usually enough to confirm the diagnosis of pneumonia and to evaluate treatment effects.
References
- Atsushi Nambu, Katsura Ozawa, Noriko Kobayashi, Masao Tago (2008) Imaging of community-acquired pneumonia: Roles of imaging examinations, imaging diagnosis of specific pathogens and discrimination from noninfectious diseases, World J Radiol 6(10): 779-793.
- T Franquet (2001) Imaging of pneumonia: trends and algorithms. European Respiratory Journal 2001 18: 196-208.
- Brent P Little, Matthew D Gilman, Kathryn L Humphrey, Tarik K Alkasab, Fiona K Gibbons, et al. (1995) Outcome of Recommendations for Radiographic Follow-Up of Pneumonia on Outpatient Chest Radiography.
- Lionel A Mandell (1995) Community-Acquired Pneumonia 108(2): 35S-42S.
- Christopher M Walker, Gerald F Abbott, Reginald E Greene, Jo-Anne O Shepard, Dharshan Vummidi et al. (2010) Imaging Pulmonary Infection: Classic Signs and Patterns.






























