Introduction
Background: Cerebral cavernous malformations CCM are rare but considered among the important cerebral condition that associated with risk of intracranial hemorrhage, focal neurological deficits and seizure from CCM change in pregnant women. Yet there is a paucity of information in the medical literature relating to the perinatal outcomes, in particular conservative approach.
Objective: To evaluate the perinatal outcome of pregnant patients diagnosed with seizure-related to CCM managed conservatively. Also, to conduct a systematic review on the risk of intracranial hemorrhage ICH and focal neurological deficits FND from Cerebral Cavernous Malformations lesion during pregnancy and its implication on the timing and mode of delivery.
Methods: (1) Present a clinical case whose diagnosed with supratentorial lobar CCM and treated conservatively. (2) Conducted a systematic review for publications on cavernous malformation during pregnancy in PubMed database. The search term used were “cavernous malformation in pregnancy” and “epileptic seizure of cavernomas”. A16 related articles and 32 case reports were found.
Result: The first case with CCM-related seizure was well-controlled on antiepileptic drugs AED while the other case of CCM was associated with no seizure symptomatology and managed conservatively without anticonvulsant treatment, both cases had good perinatal outcomes. Although, there is no available reports to support the approaches to not using antiepileptic drugs in pregnant patient with CCM? There is some studies that have reported that the initiations of conservative management (no surgical intervention) during antepartum or postpartum period may be used in the cases with asymptomatic or mildly symptomatic lesions but not in the cases with severe symptoms where neurosurgical intervention is warranted.
Conclusion: Pregnant patients with CCM who’s unable to compliance on their antiepileptic medication and willing to carry the risk of cerebral bleeding; (1) they may eventually stop the antiepileptic medication prior to the conception and managed conservatively and (2) they may have favorable perinatal outcome (3) based on the available reports there is no increased risk for cerebral hemorrhage during pregnancy and Cesarean section is indicated for obstetrical condition rather than to be performed as preferred mode of delivery for CCM.
Keywords:Cerebral cavernous malformations; Anti-epileptic drugs (AED); Epileptic seizures; Maternal and fetal outcomes
Abbreviations: ICH: Intracranial Hemorrhage; FNDs: Focal Neurological Deficits; MRI: Magnetic Resonance Imaging; GA: gestational age; H: Hemorrhage; S: Seizures; D: Diplopia; FNS: Focal Neurological Deficit; HE: Hemiparesis; CS: Cesarean Section; VD: Vaginal Delivery; TOP: Termination of Pregnancy; CCMs: Cavernous Malformation; N/R: Not Reporting; Term: Term gestation more than 37 weeks
Abstract
Cerebral cavernous malformations CCM is characterized by vascular malformations in the brain and spinal cord comprising closely clustered, enlarged capillary channels (caverns) with a single layer of endothelium without mature vessel wall elements or normal intervening brain parenchyma [1]. These vessels account for 8% to 15% of all cerebrovascular malformations and exhibit distinct features of angioarchitecture and biological mechanisms of genesis and progression [1]. Though the CCM is a rare lesion with a prevalence of 0.4%-0.5% of the population, it considered among the important condition of cerebral haemorrhage in pregnant women as it may results in epileptic seizures, stroke, symptomatic intracranial haemorrhage ICH, new focal neurological deficit FND and carry more obstetrical problems during pregnancy [2]. Although seizure has been the most common neurological manifestation of symptomatic CCMs during pregnancy that can be managed by antiepileptic drug AED regimen, but this raises a concern on its safety and the adverse fetal risk that may associated with. In view of the limited data on the most appropriate obstetric management of cavernous malformations during pregnancy. Our aim was (1) to present our successful experience on managing the pregnant women with CCM conservatively, hoping to add useful, if possible, a reasonable practical point to our obstetrical management of pregnancy associated with CCM (2) to evaluate the impact of, based on the literature data, the management approaches for these lesions during pregnancy and delivery on the perinatal outcomes.
Introduction
These CCM lesions can occur throughout the central venous system with a prevalence of 0.4%-0.5% [2]. CCM have variable presentations ranging from headache, Intracranial Hemorrhage (ICH) presenting with acute new Focal Neurological Deficits (FNDs) and epileptic seizures [3]. These lesions historically exhibited more benign features compared to their arteriovenous counterparts [4]. Because of the risk of morbidity and/or mortality due to severe hemorrhagic events and progressive neurological deterioration during pregnancy the consideration of the delivery time and mode is crucial [5]. The knowledge of these risks is useful for decision making regarding the treatment approaches in pregnant women. Neither of conservative management or neurosurgical excision options has been assessed in a randomized trial, and the use of neurosurgical excision remains controversial and challenging [6]. In view of the limited data on the most appropriate obstetric management of cavernous malformations during pregnancy. We sought to address these through (1) presented our successful conservative management for discontinuing AEDs in pregnant women with CCM. (2) conducting a systematic review to evaluate the available literature data on the implications of management approaches for these lesions during pregnancy and delivery on the perinatal outcomes.
Methods
1. Described perinatal outcomes for two cases of patients
who have cerebral cavernous malformations and managed
conservatively during the pregnancy.
a) Case 1: a healthy 28-year-old woman (gravida 2,
abortion 1). The fetal anatomy scan at 20 weeks’ gestation was
normal. The woman’s routine antenatal blood tests were all
within normal. At 23 weeks’ and 4 days gestation she presented
with unwell symptoms like lethargy, fatigue and excessive
daytime sleepiness. During the physical assessment the patient
develops a generalized type of seizure for 2-3 minutes. The attack
was accompanied by white-like foam spat from her mouth, but
no eyeball turnover, no tongue bite or urinary incontinence was
observed. The patient was suffering from dizziness and headache
after the seizure ceased. After ten minutes, another attack of
seizure occurred and lasted for 15 minutes with gradual regaining
of consciousness. The diagnosis of status epilepticus was made.
Management involves controlling the seizures by Diazepam.
The patient was intubated and admitted to intensive care unit
ICU. Laboratory test; revealed normal maternal glycaemia
and complete blood count; no electrolyte disturbances. Serum
calcium, magnesium levels and liver function tests were all within
normal limits. Further investigations after stabilization; the fetal
heart was normal. Cranial magnetic resonance imaging (MRI)
scan performed and shows hypointense lesion (size: measuring
up to 7 mm) on T2 involving the medial aspect with central
area of hyperintensity in the left frontal lobe. Fluid‑attenuated
inversion recovery FLAIR showed high signal intensity on T2, and
diffusion‑weighted imaging DWI showed isointensity on T1.
No obvious edema was found in adjacent brain parenchyma. The adjacent cortical sulci were not significantly widened. The patient was diagnosed with intracranial space‑occupying lesion, likelihood cavernous hemangioma. Over the course of the admission there were no seizures episodes, the patient was stable, her consciousness and speech were normal. Considering the fetal age and the potential side effects of seizure on the perinatal outcome, whether neurosurgical procedures are needed and to decide on safety mode of the delivery on patient and fetus. The multidisciplinary team proposed that neurosurgical intervention was not necessary, and the patient managed conservatively. She was started on anti-epileptic drugs AED and her neurological symptoms remained stable during the period of pregnancy. During the 40th weeks of gestation, she delivered vaginally, and the outcome was a healthy baby girl with good Apgar score of 9, 10 at 1 and 5 min, weighing 3350g. The patient was maintained on AED treatment with no relapses of seizure and a repeated neuroimaging MRI showed no significant changes in the lesion size, signal and morphology of the left frontal lobe cavernous malformation.
b) Case 2: Five years later, the patient was planning to conceive and decided to discontinue her anticonvulsant medication. Therefore, based on her neurological status at that time; no seizures, no neurological dysfunction symptoms related to cerebral cavernous malformations and maintained stable left frontal lobe CCM features on MRI images, the decision was made to continue conservative management during pregnancy. Fetal scan at 20 weeks showed normal anatomy. Pregnancy has been uneventful thus far, there were no symptoms of neurological deficits FND. At completed 39 weeks’ gestation, patient was delivered vaginally without major complications a baby girl with an Apgar score of 10, weighing 3601 g and discharged in satisfactory condition.
2) A systematic review was performed to identify all reports published in English till 2020 using search for “cavernous malformation during pregnancy or puerperium’’. Inclusion criteria were articles published in English with the primary topic being CCMs complicated with pregnancy and clear descriptions of the clinical presentation, management, and outcomes. Reference lists of the eligible articles were examined to identify other relevant articles. Articles that did not clearly describe the clinical presentation, management, and outcomes were excluded.
Results
a) CCM was diagnosed after the first new onset of seizure
during pregnancy of patient first child at 23 weeks of gestation.
This patient had undergone neurological management on AED.
The second pregnancy was unremarkable. The patient was safely
discontinuing AED therapy prior to conception and managed
conservatively with no seizure’s attacks through the entire period
of pregnancy. The mode of delivery was spontaneous vaginal
delivery during term weeks of gestation.
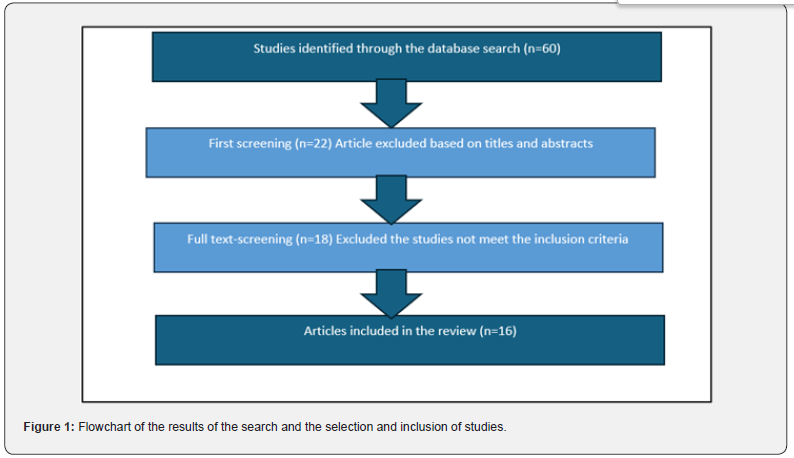
b) Analyzing the published studies of cavernous
malformation of central nervous system during pregnancy and/
or puerperium revealed 60 related publications. 22 articles based
on title/abstract assessment and 18 based on full-text assessment
were found eligible. Of these articles, 18 were selected, resulting
in the inclusion of 16 articles and 32 single case reports published
until 2020. Figure 1: Flowchart of the results of the search
and the selection and inclusion of studies. Of the 16 articles,
14 included only one to three cases, one article included five
cases, and another included six cases [7,8]. The clinical data on
management of symptomatic CCM in pregnancy, gestational age
at presentations and mode of delivery were listed in the (Table 1),
which summarizes the obstetrical outcome of 16 published cases
from the literature.

Discussion
According to the literature majority of patients with symptomatic CCMs occurred during their course of pregnancy or period of (puerperium) 6-week postpartum. Out of the 32 patients reported in single case reports, the gestational age at the time of presentation of symptomatic CCMs has been documented for 22 (79%) patients. Of these 22 patients, 16 presented with symptomatic CCM antepartum (second or third trimesters). However, four patients (18%) showed early onset of CCM symptoms in the first trimester (6 weeks of gestation), and two showed delayed onset in the postpartum period. The 32 patients showed clinical presentations of symptomatic CCMs ranging from acute ICH and onset or worsening of neurological symptoms, including seizures, FNDs, diplopia, and hemiparesis. Notably, 19 of these 32 patients (59%) had ICH. New onset or exacerbation of seizures occurred in 10 patients (31%), and other 10 patients (31%) showed progressive symptoms of hemiparesis. Further, 13 of the 32 patients (40%) exhibited symptoms of FNDs, and other nine patients (28%) had a history of worsening symptomatic hemiparesis with diplopia. As regards the information on the obstetrical mode of delivery and gestational age at delivery was available only for 24 of the 32 patients (75%). Two of these 24 patients underwent abortion on each 20 weeks of gestation who showed worsening of neurological symptoms due to bulbar CCMs and required therapeutic termination, and the other at 10 weeks of pregnancy for obstetric indication due to severe preeclampsia. Of the 24 patients, nine pregnant women (31%) with symptomatic CCMs had uncomplicated vaginal delivery. The gestational age at the time of delivery was not reported for five of these nine patients, whereas three patients delivered successfully at term gestation and one patient required preterm delivery at 33 weeks because of severe preeclampsia symptoms. Of these nine patients, two underwent neurosurgical intervention after uncomplicated pregnancy and delivery; one at 7 weeks postpartum and another at 10 years after her last pregnancy [7]. The first patient had focal seizure episodes involving the right face and arm and underwent successful resection of left insular CCMs after pregnancy at 7 weeks. The second patient underwent surgery for CCMs in the cervical medullary junction because of progressive right-sided weakness 10 years after her last pregnancy [9,10].
Thirteen of the 24 patients (45%) underwent Cesarean delivery: six at term gestation, four at preterm gestation, and the gestational age at delivery was unreported for the remaining three cases. Of these 13 patients, eight underwent Cesarean delivery because of concerns over CCMs and to reduce the risks of bleeding, one underwent Cesarean delivery because of dystocia at 40 weeks, and the indication for Cesarean delivery was unreported in the remaining of three cases. Neurosurgical resection of CCMs was performed in 4 of the 13 patients who underwent Cesarean delivery. Two of these patients had symptomatic CMMs in the pons, one of whom underwent surgery at 27 weeks of gestation and another at 29 weeks of gestation [11- 22]. Burkhardt et al. [19] reported three patients who underwent neurosurgical interventional during and after pregnancy; One patient underwent Ponto-mesencephalic CCM resection during 12 weeks of gestation and 2 weeks after the uncomplicated delivery of her second child, this patient underwent complete resection of this lesion with favorable outcomes. The other two patients underwent CCM resection postpartum: one patient at 1week postpartum and the other at 3 months postpartum [19]. Although, a great knowledge has been gained in understanding of clinical presentation, imaging features of these complex lesions and their potential complications during pregnancy and puerperium, but their pathogenesis during pregnancy remain uncertain.
Gestational hormone attributed to symptomatic hemorrhage in CCM has received increasing attention in the last decades but the exact mechanism for bleeding from these lesions during pregnancy is not fully recognized. In this dissertation, there are some studies that have emphasized that the increased production of steroid hormones during pregnancy are associated with an increased risk of hemorrhage from CCMs. Other studies showed that pregnancy not only “estrogen and progesterone”, but also vascular growth factors including vascular endothelial growth factor VEGF were upregulating during pregnancy and has been proposed to be the main cause of increasing growth in the size and angiogenesis of CCM [7]. This has been compatible with Kaya et al. [23] observation which showed that there is a different pathway mediating the process of symptomatic hemorrhage during the pregnancy than flux of gestational hormone effects [23]. Our review revealed that only one patient who had severe symptomatic lesions underwent abortion because of the worsening of neurological symptoms at 20 weeks of gestation. However, the practice of choosing an elective Cesarean delivery, with the knowledge that vaginal delivery increases the risk of ICH, to reduce the risks of hemorrhage has been revised. With limited number of reported cases of CCMs in pregnancy, it appears that the risk of hemorrhage from CCMs remains similar antepartum and postpartum. In addition, no strong evidence is available showing that the mode of delivery influences the risk of hemorrhage from CCMs; hence, we believe that the decisions regarding the management of labor and mode of delivery should be based on obstetric indications. Witiw et al. [20] reported three cases of symptomatic hemorrhages that occurred during pregnancy. All three women delivered healthy newborns; one via vaginal delivery and the other two via Cesarean delivery because of neurological indication (hemifacial weakness, mild hemisensory symptoms, and diplopia).
Notably, all these patients recovered well from their
hemorrhagic events. Seizures are the most frequent clinical
manifestations of cerebral cavernous malformation, and it has
been suggested to affect only a small group of pregnant women.
This is compatible with our observation which showed CCMrelated
seizure was incidentally diagnosed after a first seizure in
the first case and had associated with reduction risk of recurrence
during the subsequent pregnancy [19]. According to the available
data, the lifetime risk for developing a new onset of epileptic
seizures is higher in patient with CCM in cortical location, and
the risk is approximately as high as 70% with supratentorial
involvement [11]. Information on the obstetrical management of
cases complicated with seizures were thought to be caused by CCM
is very limited. According to the literature, a number of authors
have been recommended that the conservative treatment with
anti-epileptic drugs AED, regular neurological follow up, having
clinical information about the auras symptoms that may represent
seizure activity and re-evaluation post- delivery is an appropriate
approach [11]. Regarding surgical intervention, there is no
conclusive data for use this approach during pregnancy. However,
treatment decisions must consider not only the epileptogenicity of
a specific CCM lesion, but also must be weighed against maternal
and fetal complications. There are some studies suggested that
lesionectomy in cases of a life- threatening situation or rapidly
progressive clinical symptoms must be performed right away,
especially in the first week of gestation [19]. According to some
other studies, postponed surgery after the delivery in patients
have a minor symptoms or slowly progressive pattern within the
second or third trimester may be a reasonable option [19]. Hence
no available data or clinical experience to date on the potential risk
of discontinuation of AED preconceptionally in stable patient with
pre-existing CCM and whether discontinue AED would increase
their seizure risk during the pregnancy? Therefore, in parallel
with our understanding of the natural history of this lesion and
using the common sense in this area along with regards to expert’s
viewpoint, we presented our management in patient with frontal
lobe CCM who desire to conceive and stopped AED. Our decision
to manage the patient conservatively was made based on
1) patient being preconceptionally asymptomatic without
experiencing any neurological concerns (remaining seizure free)
and the stability of lesion size with approximate size of 1.7 cm on
MRI appearance [24]
2) respecting the patient’s strong desire to stop the antiepileptic
medication along with understanding and willing to
carry any adverse risk associated with discontinuing taking AEDs
during pregnancy. To the best of our knowledge, this is the first
case reported on perinatal outcome of patient with CCM who
discontinue AED through pregnancy and had an uneventful vaginal
delivery and experienced no pregnancy or delivery complications.
Conclusion
Cerebral cavernous malformations are more common than generally realized. Medical management must be tailored to everyone based on the specific circumstances. Pregnant patients harboring CCM lesion clinically asymptomatic and their neuroimaging study remains stable can be managed conservatively. Overall, pregnancy appears not has harmful effect on cavernomas course. We generally suggested, based on retrieved data and shared decision between the clinician and patient, that women with CCMs can be managed safely during trial of labor without a significant risk of adverse perinatal outcomes, and consideration needs to be given to planned Cesarean section in patients with symptomatic CCMs or when prolonged labor anticipated.
Disclosure
Conflicts of interest: None
References
- Aiba T, Tanaka R, Koike T, Kameyama S, Takeda N, et al. (1995) Natural history of intracranial cavernous malformations. J Neurosurg 83(1): 56-59.
- Zabramski JM, Wascher TM, Spetzler RF, Johnson B, Golfinos J, et al. (1994) The natural history of familial cavernous malformations: results of an ongoing study. J Neurosurg 80(3): 422-432.
- Washington CW, McCoy KE, Zipfel GJ (2010) Update on the natural history of cavernous malformations and factors predicting aggressive clinical presentation. Neurosurg Focus 29(3): E7.
- Rigamonti D, Drayer BP, Johnson PC, Hadley MN, Zabramski J, et al. (1987) The MRI appearance of cavernous malformations (angiomas). J Neurosurg 67(4): 518-524.
- Bateman BT, Schumacher HC, Bushnell CD, Pile Spellman J, Simpson LL, et al. (2006) Intracerebral hemorrhage in pregnancy: frequency, risk factors, and outcome. Neurology 67(3): 424-429.
- Safavi-Abbasi S, Feiz-Erfan I, Spetzler RF, Kim L, Dogan S, et al. (2006) Hemorrhage of cavernous malformations during pregnancy and in the peripartum period: causal or coincidence? Case report and review of the literature. Neurosurg Focus 21(1): e12.
- Kalani MY, Zabramski JM (2013) Risk for symptomatic hemorrhage of cerebral cavernous malformations during pregnancy. J Neurosurg 118(1): 50-55.
- Simonazzi G, Curti A, Rapacchia G, Gabrielli S, Pilu G, et al. (2014) Symptomatic cerebral cavernomas in pregnancy: a series of 6 cases and review of the literature. J Matern Fetal Neonatal Med 27(3): 261-264.
- Warner JE, Rizzo JF, Brown EW, Ogilvy CS (1996) Recurrent chiasmal apoplexy due to cavernous malformation. J Neuroophthalmol 16(2): 99-106.
- Pozzati E, Acciarri N, Tognetti F, Marliani F, Giangaspero F, et al. (1996) Growth, subsequent bleeding, and de novo apparance of cerebral cavernous angiomas. Neurosurgery 38(4): 662-670.
- Awada A, Watson T, Obeid T (1997) Cavernous angioma presenting as pregnancy-related seizures. Epilepsia 38(7): 844-866.
- Hoeldtke NJ, Floyd D, Werschkul JD, Calhoun BC, Hume RF (1998) Intracranial cavernous angioma initially presenting in pregnancy with new-onset seizures. Am J Obstet Gynecol 178(3): 612-613.
- Flemming KD, Goodman BP, Meyer FB (2003) Successful brainstem cavernous malformation resection after repeated hemorrhages during pregnancy. Surg Neurol 60(6): 545-547.
- Haque R, Kellner CP, Solomon RA (2008) Cavernous malformations of the brainstem. Clin Neurosurg 55: 88-96.
- Aladdin Y, Gross DW (2008) Refractory status epilepticus during pregnancy secondary to cavernous angioma. Epilepsia 49(9): 1627-1629.
- Ramı´rez-Zamora A, Biller J (2009) Brainstem cavernous malformations: a review with two case reports. Arq Neuropsiquiatr 67(3B): 917-921.
- Cohen-Gadol AA, Friedman JA, Friedman JD, Tubbs RS, Munis JR, et al. (2009) Neurosurgical management of intracranial lesions in the pregnant patient: a 36-year institutional experience and review of the literature. J Neurosurg 111(6): 1150-1157.
- Nossek E, Ekstein M, Rimon E, Kupferminc MJ, Ram Z, et al. (2011) Neurosurgery and pregnancy. Acta Neurochir (Wien). 153(9): 1727-1735.
- Burkhardt JK, Bozinov O, Nurnberg J, Shin B, Woernle CM, et al. (2012) Neurosurgical considerations on highly eloquent brainstem cavernomas during pregnancy. Clin Neurol Neurosurg 114 (8): 1172-1176.
- Witiw CD, Abou-Hamden A, Kulkarni AV, Silvaggio JA, Schneider C, et al. (2012) Cerebral cavernous malformations and pregnancy: hemorrhage risk and influence on obstetrical management. Neurosurgery 71(3): 626-630.
- Xu Y, Song Y, Zhou X, Qi Q, Liu J (2017) Case Report Pregnancy combined with epilepsy and cerebral cavernous hemangioma: a case report and literature review. Int J Clin Exp Med 10(3): 5705-5710.
- Rothbart D, Awad IA, Lee J, Kim J, Harbaugh R, et al. (1996) Expression of angiogenic factors and structural proteins in central nervous system vascular malformations. Neurosurgery 38(5): 915-925.
- Kaya AH, Ulus A, Bayri Y, Topal A, Gun S, et al. (2009) There are no estrogen and progesterone receptors in cerebral cavernomas: a preliminary immunohistochemical study. Surg Neurol 72(3): 263-265.
- Brown RD, Flemming KD, Meyer FB, Harry J Cloft, Bruce E Pollock, et al. (2005) Natural history, evaluation, and management of intracranial vascular malformations. Mayo Clin Proc 80(2): 269-281.






























