An Overview of Delirium in Hospitalized Adults: Prevention, Identification, and Management
Aishwarya Yannamani1, Sofia Flores2, Sarbagya Manandhar3, Bijan Kadel3, David Rodríguez Falla4, Jhon Navarro Gonzalez5, Marcellina Nwosu6, Robert Araujo Contreras7, Syeda Hafsa Kazmi8, Tanya Paul9, Mayra Rebeca Dominguez de Ramirez10, Ashryata Manandhar3, Abdulgafar Dare Ibrahim11 and Maria Isabel Gomez12*
1Kasturba Medical College, Manipal, India
2Department of Psychiatry, University of Medicine and Health Sciences, Saint Kitts
3Nepal Medical College, Nepal
4Universidad Privada Antenor Orrego, Peru
5Universidad del Zulia, Venezuela
6American University of Integrative Sciences School of Medicine, Barbados. El Paso Pain Center, USA
7Department of Neurology, Boston Medical Center, USA
8Dr. VRK Women’s Medical College, India
9Avalon University School of Medicine, Curaçao
10Universidad de El Salvador, El Salvador. Larkin Community Hospital, USA
11Georgia State University, USA
12Global Clinical Scholars Research Training, Harvard Medical School, USA
13Universidad del Valle, México
Submission: June 20, 2023;; Published: June 30, 2023
*Corresponding author: Maria Isabel Gomez, Universidad del Valle de Mexico, 154 Samson Rd, Frisco, TX, 76081, Mexico
How to cite this article: Aishwarya Y, Sofia F, Sarbagya M, Bijan K, David Rodríguez F, et al. An Overview of Delirium in Hospitalized Adults: Prevention, Identification, and Management. Open Access J Neurol Neurosurg 2023; 18(2): 555984. DOI: 10.19080/OAJNN.2023.18.555984.
Abstract
ADelirium is described as an acute cognitive and attentional disorder that occurs over a short period. A rigorous cognitive evaluation and an acute history of symptoms are required for a diagnosis. It affects up to 50% of hospitalized patients above 65 years of age, costing well over US$164 billion in the USA and more than $182 billion in 18 different European nations combined yearly. Delirium can be prevented by taking necessary precautions. Promising preventive measures, including cognitive stimulation, early mobilization, and medication review, have shown efficacy in reducing the incidence and severity of delirium. However, further research is warranted to deepen our understanding of the intricate interplay of risk factors and to develop precise interventions for effectively preventing and managing delirium. In this comprehensive overview, we explain the significance of early recognition of delirium by identifying the signs, symptoms and how it can be prevented and treated. Specifically, searches were conducted in PubMed and Google Scholar for systematic reviews, meta-analyses, and reviews related to the above information. The pathophysiology of delirium is complex and multifactorial. Understanding the pathophysiology of delirium involves considering various contributing factors, including neurotransmitter imbalances, inflammation, oxidative stress, and neuronal network dysfunction. While several causes exist, up to 39% of delirium episodes are due to adverse drug effects. The diagnosis is based on a comprehensive assessment that integrates clinical history, physical examination, mental status examination, laboratory investigations, and, in some cases, neuroimaging. Several differential diagnoses should be considered when evaluating a patient with delirium, such as dementia, psychosis, and mood disorders. Management of delirium requires a multidimensional approach which includes addressing underlying causes, non-pharmacological and pharmacological interventions. Future research should focus on evaluating the long-term effects of different treatment modalities and identifying personalized approaches for specific patient populations.
Keywords: : Delirium; Acute confusional state; Hospital-acquired delirium, Diagnosis; Differentials; Treatment
Abbreviations: ICU: Intensive care unit; GABA: Gamma-aminobutyric acid; CAM: Confusion Assessment Method; DRS: Delirium Rating Scale; EEG: Electroencephalogram; COPD: Chronic Obstructive Pulmonary Disease; MDD: Major Depressive Disorder; GAD: Generalized Anxiety Disorder; PTSD: Post-Traumatic Stress Disorder; ARDS: Acute Respiratory Distress Syndrome; ASA: American Society of Anesthesiologists; CNS: Central Nervous System; ROS: Reactive Oxygen Species; DNA: Deoxyribonucleic Acid; CBC: Complete Blood Count; CT: Computed Tomography; MRI: Magnetic Resonance Imaging; MMSE: Mini-Mental Status Examination; POD: Postoperative Delirium
Introduction
Delirium is defined as the presence of an acute and fluctuating disturbance of consciousness and cognition that develops over a short period of time [1]. It is a common condition, especially among older adults. Its prevalence varies depending on the setting, with higher rates reported in hospital and intensive care unit (ICU) populations. Estimates suggest that delirium affects approximately 15-30% of hospitalized patients and up to 80% of critically ill patients in the ICU. Delirium is associated with increased morbidity, mortality, and healthcare costs [2,3]. This neurologic syndrome is commonly caused by underlying medical conditions, medication side effects, or drug withdrawal. Several risk factors contribute to the development of this condition. Advanced age is a significant risk factor, as older adults are more susceptible to delirium due to physiological changes, multiple comorbidities, and polypharmacy. Other risk factors include pre-existing cognitive impairment, sensory impairment, severe illness, immobilization, and infections or systemic inflammation [1,4]. Delirium's physiopathology is multifactorial and involves a complex interplay of neurotransmitter imbalances, neuroinflammation, oxidative stress, and disrupted cerebral metabolism. Contributing factors include dysregulation of acetylcholine, dopamine, and gamma-aminobutyric acid (GABA) systems, as well as alterations in the glutamate and serotonin pathways. Additionally, systemic inflammation and immune response activation play a significant role in the pathogenesis of delirium [5].
Delirium is clinically characterized by impaired attention, awareness, and cognitive function, often accompanied by perceptual disturbances, disorganized thinking, and an altered sleep-wake cycle. Moreover, patients may exhibit agitation with restlessness or hypoactivity with withdrawn behavior. Diagnosing this condition requires a comprehensive assessment considering the patient's clinical presentation, medical history, and cognitive function. Validated tools such as the Confusion Assessment Method (CAM) or the Delirium Rating Scale (DRS) might aid the diagnosis [5,6]. Additionally, laboratory tests, neuroimaging, and electroencephalogram (EEG) may be performed to identify underlying causes and rule out other conditions mimicking delirium. Prompt recognition and accurate diagnosis are crucial for appropriate management. The treatment of delirium involves addressing underlying causes and providing supportive care. Strategies include managing medical conditions, discontinuing, or adjusting medications contributing to delirium, ensuring a safe and calm environment, promoting orientation and cognitive stimulation, and optimizing sensory input. Non-pharmacological interventions, such as reorientation techniques, maintaining sleep-wake cycles, and involving family or caregivers, are commonly emphasized [3,7]. In severe cases, pharmacological interventions may be considered, including low-dose antipsychotics or sedative-hypnotics, although their use is cautious due to potential side effects [7]. This narrative review aims to provide a clear and comprehensive overview of delirium, a highly prevalent yet often underdiagnosed condition in hospitalized adults. By shedding light on the key aspects of delirium, this article strives to promote timely recognition, accurate diagnosis, and effective management strategies to improve patient outcomes and reduce the burden of this condition in hospital settings.
Epidemiology & Risk factors
Delirium is a common neuropsychiatric syndrome characterized by acute cognitive impairment and a fluctuating course. The morbidity, mortality, and healthcare costs associated with delirium underscore the importance of understanding its epidemiology and risk factors for effective prevention and management. The incidence and prevalence of delirium vary across healthcare settings, with hospital-based studies reporting incidence rates ranging from 11% to 51% among hospitalized patients[5]. Mainly high rates are observed in intensive care units and postoperative settings. In contrast, prevalence rates ranging from 10% to 31% have been documented in hospitalized patients, with rates exceeding 50% in elderly populations residing in long-term care facilities [5,8]. Patients with delirium have been found to have a mortality rate of approximately 22%, compared to around 10% for patients without delirium[9].
Understanding the epidemiology and risk factors of delirium enables the implementation of targeted preventive strategies tailored to address these factors. By identifying high-risk individuals, healthcare professionals can intervene early and mitigate the delirium burden. Lundström et al. (2014) conducted a study that revealed a clear association between delirium and an increased risk of functional decline and extended hospital stays. Specifically, patients with delirium experienced an average of 6.8 additional hospital days compared to those without delirium [10]. Furthermore, Leslie et al. (2008) estimated that delirium has a significant economic impact, amounting to approximately $143 billion annually in the United States alone. These costs can be attributed to more extended hospital stays, increased utilization of medical resources, and subsequent rehabilitation requirements[11].
Promising preventive measures, including cognitive stimulation, early mobilization, and medication review, have shown efficacy in reducing the incidence and severity of delirium [12]. However, further research is warranted to deepen our understanding of the intricate interplay of risk factors and to develop precise interventions for effectively preventing and managing delirium.
Delirium can manifest as a common complication at various stages of the surgical process, including the preoperative, intraoperative, and postoperative periods, with a three-fold increased risk of postoperative complications compared to those without delirium[13]. Recognizing the specific risk factors associated with each stage is crucial for identifying high-risk individuals and implementing preventive strategies accordingly. Certain preoperative circumstances may influence the likelihood of experiencing an episode of delirium. These include:
Medications: Certain medications, such as benzodiazepines, anticholinergic drugs, and antipsychotic drugs, are more likely to increase the risk of delirium [8,14-16]. Assessing the necessity of these medications and considering alternative options can help reduce the risk. Furthermore, a retrospective cohort study conducted by Kurisu Ken et al. found that patients prescribed and taking more than six medications were more susceptible to developing delirium, with 55% of the patients experiencing such episodes [17].
Cognitive Impairment & Dementia: Identifying and addressing pre-existing cognitive impairment or dementia through cognitive stimulation programs and appropriate management strategies may decrease the probability of delirium[17].
Comorbid Medical Conditions: Pre-existing medical conditions, particularly cardiovascular and respiratory diseases, can increase the risk of delirium in the preoperative period[15,18]. Additionally, hypertension has been a coexisting condition in around 34%, Diabetes Mellitus in 19%, COPD in 15%, and ischemic heart disease in 8% [19]. Sensory impairment, including vision or hearing loss, has been identified as a potential contributor to the development of delirium. Impaired vision and hearing can disrupt sensory input and lead to difficulties in perceiving and interpreting environmental cues, which may contribute to confusion and disorientation, common features of delirium [20]. Studies have shown that individuals with sensory impairment are more susceptible to delirium during hospitalization or in long-term care settings[21,22]. These conditions may exacerbate the physiological stress of surgery and impair cognitive function.
Pre-existing psychiatric conditions: Including Major Depressive Disorder (MDD), Generalized Anxiety Disorder (GAD), Bipolar disorder, Schizophrenia, and post-traumatic stress disorder (PTSD). A retrospective study by Kalra et al. found that 49.2% of patients with ARDS and a comorbid pre-existing psychiatric condition experienced ICU delirium, compared to 34% of ARDS patients experiencing delirium with no prior psychiatric condition [23].
Hyponatremia: It has been seen in around 34% of delirious patients. Correcting this electrolyte imbalance immediately and aggressively is recommended to prevent or lower the chances of developing delirium [24].
Comprehensive Preoperative Assessment: Conduct a thorough preoperative assessment that includes evaluating the patient's functional status, nutritional status, sensory impairments, and psychosocial factors (e.g., social support, depression) to identify potential risks and develop appropriate interventions [15]. A history of alcohol abuse can also contribute to delirium development. Psychosocial factors like social isolation, depression, and high-stress levels have been linked to an elevated risk of delirium [8].
By addressing and modifying these preoperative risk factors through a comprehensive preoperative assessment, healthcare professionals can work towards minimizing the occurrence of delirium and improving patient outcomes. Additionally, certain preoperative risk factors for delirium are non-modifiable and inherent to the patient's characteristics or medical history. These include:
Age & Gender: Advanced age is a significant risk factor for delirium, with older adults being more susceptible [12,25]. As individuals age, physiological changes occur, rendering them more vulnerable to cognitive impairment and delirium. This vulnerability affects approximately one in three hospitalized individuals aged 70 and above [26]. Furthermore, there is evidence suggesting that the male gender plays a significant role in the occurrence of delirium, with a higher prevalence observed among males (38%) compared to females (21%) [27].
Preexisting Cognitive Impairment or Dementia: Individuals with preexisting cognitive impairment, such as a history of stroke or dementia, are at a higher risk of developing delirium [8,17]. Dementia at a rate of around 20% [24]. Concluding that the presence of underlying cognitive deficits increases susceptibility to delirium episodes.
History of Delirium or Dementia: Previous episodes of delirium or a history of dementia contribute to an increased risk of delirium in the preoperative period [1,28]. These conditions may make individuals more vulnerable to delirium recurrence.
American Society of Anesthesiologists (ASA) Physical Status Classification: A higher ASA physical status classification assesses the patient's overall health status and has been associated with an increased risk of delirium [29]. Patients with poorer physical health may be more vulnerable to delirium.
While these risk factors cannot be modified, their identification allows healthcare professionals to implement appropriate strategies to minimize the impact of delirium in high-risk patients.
Intraoperative risk factors for delirium encompass various factors, including the type and duration of surgery, blood loss, use of anesthetics (particularly volatile anesthetics), and intraoperative hypotension [15]. Prolonged surgical duration, higher blood loss, and exposure to specific anesthetic agents have been associated with an increased incidence of delirium. Closely monitoring hemodynamic parameters, minimizing blood loss, and judicious use of anesthetics can reduce the risk of intraoperative delirium.
Lastly, postoperative risk factors for delirium involve factors such as pain, immobility, sleep disturbances, medication side effects (such as opioids), and the presence of postoperative complications like infections or electrolyte imbalances [30]. Effective pain management, early mobilization, optimization of sleep patterns, and vigilant monitoring for and prompt treatment of postoperative complications.
Delirium Physiopathology
Delirium is a complex and multifactorial neuropsychiatric syndrome commonly occurring in hospitalized adults and elderly individuals, particularly those in intensive care units or postoperative settings. Understanding the pathophysiology of delirium involves considering various contributing factors, including neurotransmitter imbalances, inflammation, oxidative stress, and neuronal network dysfunction [31].
Delirium has been associated with alterations in various neurotransmitter systems. Cholinergic deficiency is a well-established mechanism in delirium, resulting from decreased acetylcholine synthesis and activity. Studies have shown that reduced cholinergic activity leads to impaired attention and cognitive function. Additionally, imbalances in other neurotransmitters, such as dopamine, serotonin, and gamma-aminobutyric acid (GABA), have been implicated in delirium, although their specific roles and interactions are still being investigated [31,32]. Moreover, inflammatory processes play a significant role in the pathophysiology of delirium. Systemic inflammation, often triggered by infection or other physiological insults, can lead to the production and release of pro-inflammatory cytokines and other immune mediators. These mediators can cross the blood-brain barrier and activate inflammatory pathways within the central nervous system (CNS). The resulting neuroinflammation disrupts neuronal function and alters neurotransmitter activity, contributing to the development of delirium [33].
Increased oxidative stress is another important mechanism in delirium. Oxidative stress occurs when there is an imbalance between the production of reactive oxygen species (ROS) and the body's antioxidant defense mechanisms. ROS can cause damage to cellular components, including lipids, proteins, and DNA. Studies have demonstrated elevated levels of oxidative stress markers in delirious patients, suggesting that oxidative damage may contribute to the pathogenesis of delirium [33-35].
Lastly, delirium is characterized by abnormal neuronal network activity and disrupted connectivity within the brain. Electroencephalography (EEG) studies have shown patterns of diffuse slowing and decreased connectivity in delirium, indicating impaired communication between different brain regions. This disruption of standard neural circuits leads to cognitive deficits, attentional disturbances, and altered consciousness [36]. In addition to the pathophysiological mechanisms discussed above, several physiological changes contribute to the development of delirium in adults and elderly hospitalized individuals. These changes involve alterations in the sleep-wake cycle, disrupted circadian rhythms, and impaired cerebral perfusion. The latter changes further exacerbate cognitive dysfunction and contribute to the development and persistence of delirium [35-37].
Surgery, anesthesia, substance use/withdrawal, hepatic failure, hypoxia, infections, hypoglycemia, and acute worsening of chronic illnesses are all leading factors that can result in delirium. In patients with severe dementia, even minor disruptions such as dehydration, inadequate sleep, urinary retention, and constipation can induce delirium[38]. Cholinergic and noradrenergic neural tissues deteriorate with dementia and advancing age. Additionally, aging and neurodegeneration disrupt the connection among neurons, so there is cognitive decline, inflammation, impaired plasma protein transport, and blood flow into the brain, and it also exposes the brain to peripheral inflammatory cytokines through a compromised blood-brain barrier [39].
An increase in serum levels of TNF‐α (a major inflammatory cytokine) and a 2-time higher risk of cognitive decline over 6 months were both linked to acute systemic inflammatory events, according to a recent study that examined the impact of acute and chronic inflammation on cognitive decline in patients with Alzheimer's disease. Compared to those with low TNF‐α levels, those with greater baseline TNF‐α levels had a 4 times greater risk of cognitive impairment during a 6-month period and were more likely to have delirium [40].
While several causes exist, up to 39% of delirium episodes are due to adverse drug effects [38]. Benzodiazepines, opioids, antihistamines, and dihydropyridines are believed to carry the most significant risk for inducing delirium [39].A 2020 meta-analysis of 33 studies about medical inpatients found an overall delirium occurrence of 23% among elderly patients [39]. Since the elderly are at high risk for delirium, the American Geriatric Society has released the "2019 Updated AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults'' for clinicians to decrease the potential for delirium. Another useful resource is the website "ACBcalc.com," which offers both drug substitutes with decreased anticholinergic activity and the complete anticholinergic effects of the patient medications so clinicians can optimize patient safety[38].
Even though the duration of delirium is brief in nature, the episode can continue for extended periods in susceptible patients. According to a systematic review, hospital delirium remained until discharge in 45% of patients and lasted one month later in 33% of cases [38]. Patients who exhibit specific delirium symptoms but do not meet all diagnostic criteria have been called "subsyndromal delirium" [39]. Delirium is a severe condition. It can be preventable if the signs are detected early, and appropriate safety measures are taken. Delirium in the ICU is linked to a 2 to 4-fold more significant risk of mortality, and there is a 70% increased risk of death in six months in patients who report to the emergency department with delirium [38].
It is important to note that the pathophysiology of delirium is complex and multifactorial, and not all cases of delirium follow the exact same mechanisms. The interplay between various physiological, biochemical, and neurobiological factors contributes to the heterogeneity of delirium in clinical settings.
Clinical Presentation
Delirium should always be considered when there is a new onset or an acute or subacute decline in behavior, cognition, or function, particularly in old, demented, or depressed individuals [41]. Delirium symptoms often appear gradually over a few hours or days. Symptoms may come and go but worsen in dark and unfamiliar environments and worsen more severely in unfamiliar environments, such as hospitals [42-44]. Inattention, temporary disturbances of consciousness, and a sharp shift from baseline in psychotic symptoms are the main characteristics of delirium. Additionally, there might be additional cognitive issues, including memory loss, confusion, language problems, visual hallucination, or emotional problems [42,44]. Sleep-wake cycle problems, speech and language issues, affective lability, perceptual abnormalities (hallucinations, illusions, etc.), and delusions are some of the non-cognitive symptoms of delirium. Disruptions to the sleep-wake cycle can vary from naps and nocturnal disturbances to a severe breakdown of the circadian rhythm [44].
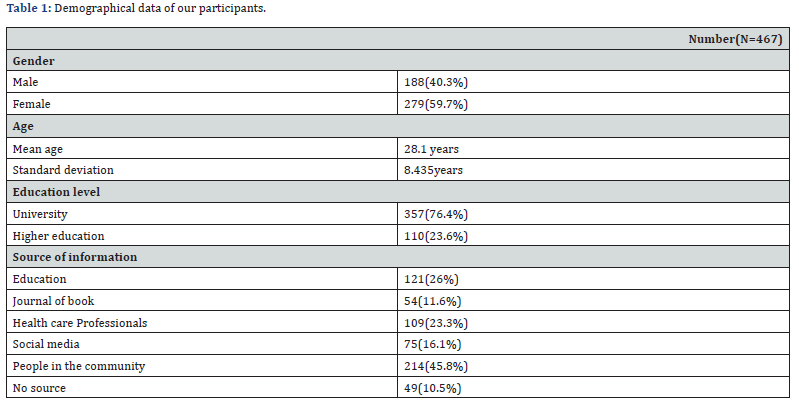
Delirium is frequently divided into three categories depending on clinical presentations. Patients that are hyperactive display elevated agitation and sympathetic activity. They may exhibit hallucinations, delusions, and aggressive or disobedient conduct on rare occasions. Increased somnolence and reduced alertness are symptoms of hypoactive patients. Hypoactive delirium is harmful as it frequently goes undiagnosed or is confused with lethargy or sadness. Higher rates of illness and death are linked to it. Lastly, between hyperactive and hypoactive presentation, patients might swing [41,43-45]. The differences between the subtypes of delirium are shown in Table 1.
Delirium Identification
In order to diagnose delirium in an adult hospitalized with a chronic illness, several diagnostic approaches can be employed. Delirium is a complex neuropsychiatric syndrome characterized by acute onset and fluctuations in attention and cognition. It is crucial to promptly identify and diagnose delirium in hospitalized patients as it is associated with increased morbidity, mortality, and healthcare costs [1,37]. The diagnosis of delirium begins with a thorough clinical assessment, including a detailed medical history and physical examination. The medical history should focus on the onset and duration of symptoms, any potential precipitating factors (e.g., recent surgery, medication changes, infections), and the presence of comorbidities that may contribute to delirium development (e.g., dementia, substance use disorders). Physical examination helps to identify any underlying medical conditions or signs of infection, neurologic abnormalities, or medication side effects. A mental status examination is vital to the diagnostic process [1,4]. It involves assessing the patient's level of consciousness, attention, orientation, memory, language, and executive functions. Observational tools, such as the Confusion Assessment Method (CAM) or the CAM for the Intensive Care Unit (CAM-ICU), are commonly used to evaluate delirium systematically. These tools involve structured assessments of attention, fluctuation in mental status, disorganized thinking, and altered levels of consciousness [12-14].
Laboratory investigations are crucial in diagnosing delirium and identifying any underlying medical conditions. Blood tests, including complete blood count (CBC), electrolyte levels, renal and liver function tests, blood glucose, thyroid function tests, and infection markers (e.g., C-reactive protein, procalcitonin), are commonly ordered. These tests help detect electrolyte imbalances, metabolic derangements, infections, and other systemic abnormalities that can contribute to delirium [37]. Moreover, neuroimaging studies, such as computed tomography (CT) or magnetic resonance imaging (MRI) of the brain, may be indicated to rule out structural abnormalities, intracranial hemorrhage, or other focal lesions causing delirium. These studies are typically reserved for patients with atypical features, focal neurologic deficits, or when there is a concern for an underlying structural brain lesion [1,29].
Collaboration with other specialties is often necessary in the diagnostic process. Consultation with a psychiatrist or neurologist can provide further insight into the patient's mental status and aid in differentiating delirium from other neuropsychiatric disorders. Additionally, consultation with other medical specialties may be required to address and manage any underlying medical conditions contributing to delirium [37]. Lastly, it is important to note that no single diagnostic test can definitively confirm the diagnosis of delirium. Instead, the diagnosis is based on a comprehensive assessment that integrates clinical history, physical examination, mental status examination, laboratory investigations, and, in some cases, neuroimaging. Utilizing these diagnostic methods makes it possible to identify and manage delirium promptly, leading to improved patient outcomes.
Several differential diagnoses should be considered when evaluating a patient presenting with delirium, as its clinical presentation may resemble other neuropsychiatric conditions such as dementia, psychosis, and mood disorders. These are all distinct clinical entities characterized by different sets of symptoms and underlying mechanisms. Understanding the differences between these conditions is crucial for accurate diagnosis and appropriate management.
Delirium is an acute, fluctuating state of confusion and disorientation. An underlying medical condition, such as infection, metabolic disturbances, medication side effects, or substance withdrawal, primarily causes it. Impairments in attention, memory, perception, and thinking characterize delirium. Patients with delirium often experience rapid-onset cognitive dysfunction, hallucinations, and disturbances in the sleep-wake cycle. Delirium tends to resolve once the underlying cause is identified and treated. Dementia, however, is a chronic and progressive syndrome characterized by a cognitive decline that interferes with daily functioning. Unlike delirium, dementia develops slowly over time and is caused by degenerative changes in the brain, such as Alzheimer's disease, vascular dementia, or frontotemporal dementia. Impairments in memory, language, problem-solving, and executive functions characterize dementia. Behavioral and psychological symptoms, including mood changes, may also be present. Dementia is typically irreversible and requires long-term management and support [3].
Psychosis refers to symptoms characterized by a loss of touch with reality. It can occur in various conditions, including schizophrenia, bipolar disorder, or severe depression. Psychosis involves distortions in perception, such as hallucinations (e.g., hearing voices or seeing things that are not there) and delusions (firmly held beliefs that are not based on reality). Psychotic symptoms can significantly affect a person's thoughts, emotions, and behavior, leading to social and occupational impairment [11,12].
Lastly, depression disorder encompasses a range of conditions characterized by persistent sadness, hopelessness, and a loss of interest or pleasure in daily activities. Mood disorders are not limited to temporary emotional states but can significantly impact an individual's quality of life. Symptoms may include changes in appetite and sleep patterns, fatigue, difficulty concentrating, and thoughts of self-harm or suicide. Treatment for mood disorders often involves a combination of medication, psychotherapy, and lifestyle modifications [4-6].
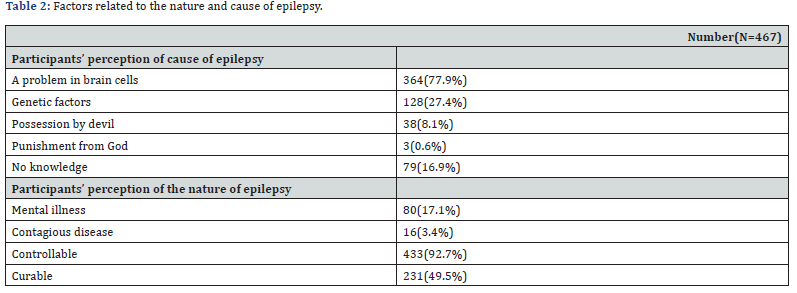
In summary, delirium is an acute confusional state caused by underlying medical conditions, dementia is a chronic and progressive cognitive decline, psychosis involves a loss of touch with reality, and mood disorders involve persistent disturbances in mood and emotional well-being. Each condition has distinct clinical features and underlying causes, requiring tailored approaches to diagnosis and management. A comparison between delirium classical features and other delirium-like disorders can be found inTable 2.
Treatment Strategies
Delirium, characterized by an acute and fluctuating change in cognition and attention, is a common condition among hospitalized patients that leads to poor outcomes [46,47]. Effective screening and prompt treatment are crucial to improve patient outcomes and reduce the risk of complications [48,47]. Management of delirium includes non-pharmacological as well as pharmacological interventions. Non-pharmacological interventions play a substantial role in the management of delirium. The multimodal approach prioritizes patients’ safety and provides supportive measures such as environmental modifications aimed to create a calm and familiar environment, cognitive stimulation with repeated re-orientation, adequate lighting, minimizing noise, and maintaining a consistent daily routine [49]. Promoting sleep-wake cycles is another crucial aspect of it. It involves providing quiet and dimly lit surroundings during the night, encouraging daytime activities and social interaction, and avoiding the use of sedating medications whenever possible [50]. Early mobilization and physical therapy have demonstrated promising results in preventing and managing delirium [51]. In addition to this, family engagement and education are vital components of delirium management. Involving family members in the care process and providing them with information about delirium can enhance patient outcomes and facilitate a smoother transition after discharge [52].
Pharmacological interventions are also being meticulously studied. Antipsychotics such as haloperidol and atypical antipsychotics like olanzapine, quetiapine, and risperidone have shown significant benefits in reducing the severity and duration of delirium episodes, especially in agitated and hyperactive delirious patients [49,53]. But hypervigilance should be exercised due to potential adverse effects, specifically in geriatric patients for the adverse effects such as prolonged QT, arrhythmia, sedation, extrapyramidal symptoms, and increased risk of falls [49]. Although antipsychotics are usually beneficial for treating delirium in hospitalized patients, their efficacy in preventing the episode of cognitive deficit is highly doubtful [54]. Benzodiazepines, on the other hand, typically worsen cognitive function and lead to excessive sedation and therefore are best avoided except in the case of alcohol withdrawal-induced delirium tremens. The role of ramelteon and dexmedetomidine are currently being studied, and the primitive data may suggest these agents may be useful in managing delirium. But further study is required [49].
Simultaneously, identifying the medical causes and managing them adequately is the key to managing the episode. An inclusive medical evaluation beginning with medication review, vitals sign and hydration status, detailed physical and neurological examination, signs of infection and sepsis, bowel and bladder function, and review of the overall system to rule out acute respiratory, hepatic, uremic, neurological, and cardiovascular conditions, perform baseline laboratory and imaging investigations to evaluate electrolyte imbalances, metabolic disturbances, and injury. Addressing these reversible causes with appropriate medical and surgical treatment can significantly contribute to delirium resolution [49].
Given the above, the treatment of delirium in hospitalized patients requires a multidimensional approach. Pharmacological interventions, non-pharmacological strategies, and addressing underlying causes all play a crucial role in managing delirium effectively. A comprehensive care plan that includes family involvement and education can further optimize patient outcomes. Future research should focus on evaluating the long-term effects of different treatment modalities and identifying personalized approaches for specific patient populations.
Prognosis and Complications
Delirium increases mortality in hospitalized elderly patients and has remained unchanged over the last three decades despite the advancement in delirium research [55]. Several hypotheses have been proposed to explain the connection between delirium and death, but its precise nature is still unknown. These hypotheses may overlap and interact to affect mortality.
Delirium is a ubiquitous complication in the postoperative period [56,57]. Studies have shown that elderly hospitalized patients with hip fractures are more likely to develop delirium resulting in increased mortality [58]. In the study by Edelstein et al. [58] out of 921 patients who underwent hip fracture repair developed delirium and had increased mortality in one year [58,59]. They were also less likely to return to the pre-fracture level of function in one year [58]. Thus, postoperative delirium may result in a decline in function by impeding rehabilitation [59].
Delirium can cause brain injury and cognitive deficit due to neuroinflammatory reactions, dysregulation of neurotransmitters, and disturbance of cerebral metabolism, with the potentially fatal sequela of irreversible neuronal death [55]. In the study by Bickel et al. [60] 200 patients over 60 who underwent hip surgery and had no known neurological impairment at baseline were followed for 38 months [60]. The telephone Mini-Mental Status Examination (MMSE) was used to evaluate their cognitive status eight and 38 months after discharge. Cognitive impairment was present in 53.8% of postoperative delirium (POD) patients compared to 4.4% of those without delirium [60]. Other delirium-related complications include aspiration pneumonia, falls, restraint use, pressure ulcers, readmissions, hospital-acquired comorbidities, increased hospital length of stay resulting in higher morbidity and mortality, higher healthcare cost, and increased financial burden to the family and society [56,57,59,61,62]. Delirium is also a risk factor for frailty due to increased morbidities seen in delirious patients [55,58,59,63]. Due to the increased number of diverse frailty and POD assessment tools, it is frequently challenging to characterize the relationship [62].
Depending on the underlying condition, delirious patients may recover wholly or substantially but in a deficient state. The immediate death rate of 25-33% is comparable to that of acute myocardial infarction or sepsis; 25 % of elderly delirious hospitalized patients die around three to four months after diagnosis, with the underlying conditions accounting for only a portion of this excess mortality [63].
The coexistence of delirium and dementia leads to a worse prognostic outcome than the coexistence of metabolic and toxic conditions, with most of these patients admitted to nursing homes. Early detection and treatment of delirium improve outcomes in delirious elderly hospitalized patients, minimizing delirium severity, duration, and its sequelae [63-70].
Conclusion
Delirium is a complex neuropsychiatric syndrome characterized by acute onset and fluctuations in attention and cognition. It represents a challenge in healthcare settings, diagnosis, and management, particularly among hospitalized elderly patients. The clinical presentation of delirium involves a new onset or acute decline in behavior, cognition, or function, often accompanied by disturbances in consciousness, attention, memory, and perception. It can manifest in hyperactive, hypoactive, or mixed forms, further complicating its diagnosis. Diagnostic approaches such as clinical assessments, mental status examinations, observational tools, laboratory investigations, and collaboration with specialists are crucial for accurately diagnosing delirium and ruling out other conditions. Managing delirium requires a multidimensional approach that includes both non-pharmacological and pharmacological interventions. Non-pharmacological strategies, such as environmental modifications, cognitive stimulation, sleep-wake cycle promotion, early mobilization, and family engagement, play a vital role in creating a supportive and familiar environment for patients. Pharmacological interventions, particularly antipsychotics, may be beneficial for reducing the severity and duration of delirium episodes, but careful consideration of potential adverse effects is necessary, especially in geriatric patients. Addressing underlying medical conditions contributing to delirium through comprehensive medical evaluations and appropriate treatment is also essential.
Despite advancements in delirium research, its association with increased morbidity, mortality, and healthcare costs remains a significant concern. Therefore, future research should focus on evaluating the long-term effects of different treatment modalities and identifying personalized approaches for specific patient populations. Additionally, further investigation is needed to understand the precise nature of the connection between delirium and mortality, as well as the impact of delirium on cognitive function and functional decline.
References
- American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (5th). American Psychiatric Publishing.
- Inouye SK, Westendorp RG, Saczynski JS (2014) Delirium in elderly people. The Lancet 383(9920): 911-922.
- Inouye SK (2006) Delirium in older persons. New England Journal of Medicine 354(11): 1157-1165.
- Fong TG, Davis D, Growdon ME, Albuquerque A, Inouye SK (2015) The interface between delirium and dementia in elderly adults. Lancet Neurol 14(8): 823-832.
- Siddiqi N, House AO, Holmes JD (2006) Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing 35(4): 350-364.
- Maldonado JR (2018) Delirium pathophysiology: An updated hypothesis of the etiology of acute brain failure. Int J Geriatric Psychiatry 33(11): 1428-1457.
- Neufeld KJ, Yue J, Robinson TN, Inouye SK, Needham DM (2018) Antipsychotic Medication for Prevention and Treatment of Delirium in Hospitalized Adults: A Systematic Review and Meta-Analysis. J Am Geriatrics Soc 66(4): 602-611.
- Fong TG, Tulebaev SR, Inouye SK (2009) Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol 5(4): 210-220.
- Witlox J, Eurelings LS, de Jonghe JF, Kalisvaart KJ, Eikelenboom P, et al.(2010) Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis JAMA 304(4): 443-451.
- Lundström M, Edlund A, Karlsson S, Brännström B, Bucht G, et al. (2014) A multifactorial intervention program reduces the duration of delirium, length of hospitalization, and mortality in delirious patients. J Am Geriatrics Soc 62(11): 2205-2212.
- Leslie DL, Marcantonio ER, Zhang Y, Leo-Summers L, Inouye SK (2008) One-year health care costs associated with delirium in the elderly population. Arch Intern Med 168(1): 27-32.
- Oh ES, Fong TG, Hshieh TT, Inouye SK (2017) Delirium in older persons: advances in diagnosis and treatment. JAMA 318(12): 1161-1174.
- Marcantonio ER, Goldman L, Orav EJ, Cook EF, Lee TH (1994) The association of intraoperative factors with the development of postoperative delirium. Am J Med 97(6): 469-475.
- Westendorp RG, Saczynski JS, Inouye SK (2014) Delirium in elderly people. The Lancet 383(9920): 911-922.
- Aldecoa C, Bettelli G, Bilotta F, Robert DS, Riccardo A, et al. (2017) European Society of Anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur J Anaesthesiol 34(4): 192-214.
- Kim H, Chung S, Joo YH, Lee JS (2016) The major risk factors for delirium in a clinical setting. Neuropsychiatr Dis Treat 12: 1787-1793.
- Lee HB, Mears SC, Rosenberg PB, Leoutsakos JM, Gottschalk A, et al. (2011) Predisposing factors for postoperative delirium after hip fracture repair in individuals with and without dementia. J Am Geriatr Soc 59(3): 2306-2313.
- Inouye SK, Leslie DL (2011) The importance of delirium: Economic and societal costs. Journal of the American Geriatrics Society, 59(Suppl 2), 59(s2): S241-S243.
- Hashmi M, Ahmed W, Raza SA, Khan MF, Salim B, et al. (2021) Incidence and risk factors of delirium in surgical intensive care unit. Trauma surgery & acute care open 6(1): e000564.
- Fick DM, Agostini JV, Inouye SK (2002) Delirium superimposed on dementia: a systematic review. J Am Geriatrics Soc 50(10): 1723-1732.
- Saczynski JS, Marcantonio ER, Quach L, Fong TG, Gross A, et al. (2012) Cognitive trajectories after postoperative delirium. New England Journal of Medicine 367(1): 30-39.
- LaHue SC, Liu VX (2016) Loud and Clear: Sensory Impairment, Delirium, and Functional Recovery in Critical Illness. American journal of respiratory and critical care medicine 194(3): 252-253.
- Kalra SS, Jaber J, Alzghoul BN, Hyde R, Parikh S, et al. (2021) Pre-Existing Psychiatric Illness Is Associated With an Increased Risk of Delirium in Patients With Acute Respiratory Distress Syndrome. Journal of intensive care medicine 37(5): 647-654.
- Zieschang T, Wolf M, Vellappallil T, Uhlmann L, Oster P, et al.(2016) The Association of Hyponatremia, Risk of Confusional State, and Mortality. Dtsch Arztebl Int 113(50): 855-862.
- Marcantonio ER, Goldman L, Mangione CM, Ludwig L E, Muraca B, et al. (1994) A clinical prediction rule for delirium after elective noncardiac surgery. JAMA 271(2): 134-139.
- (2020) HealthinAging.org.
- Wittmann M, Kirfel A, Jossen D, Mayr A, Menzenbach J (2022) The Impact of Perioperative and Predisposing Risk Factors on the Development of Postoperative Delirium and a Possible Gender Difference. Geriatrics (Basel) 7(3): 65.
- Witlox J, Eurelings LS, de Jonghe JF, Kalisvaart KJ, Eikelenboom P, et al. (2010) Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA 304(4): 443-451.
- Bogardus Jr, Sidney T, Charpentier PA, Leo-Summers L, Acampora D, et al. (1999) A multicomponent intervention to prevent delirium in hospitalized older patients. New England Journal of Medicine 340(9): 669-676.
- Sieber FE, Barnett SR (2011) Preventing postoperative complications in the elderly. Anesthesiol Clin 29(2): 83-97.
- Maclullich AM (2004) The pathophysiology of delirium: advancing the hypothesis of synaptic failure. J Neurol Neurosurg Psychiatry 75(10): 1466-1471.
- Munster BC (2011) The pathophysiological substrate of delirium and its motoric subtypes: a systematic review. J Psychosom Res 71(6): 301-307.
- Jin HH, Wilson A, Ely EW (2010) Delirium in the older emergency department patient: a quiet epidemic. Emerg Med Clin North Am 28(3): 611-631.
- Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, et al. (2013) Long-term cognitive impairment after critical illness. N Engl J Med 369(14): 1306-1316.
- Cerejeira J, Firmino H, Adriano VS, Elizabeta B (2010) The neuroinflammatory hypothesis of delirium. Acta Neuropathol 119(6): 737-54.
- Kotfis K (2019) Brain-heart interactions in delirium: implications for management in the ICU. Intensive Care Med Exp 7(Suppl 1): 25.
- Witlox J, Lisa SM, Jos FM, Kees JK, Piet E, et al. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA 304(4): 443-451.
- Ramírez Echeverría MdL, Schoo C, Paul M (2023) Delirium In: StatPearls. Treasure Island (FL): StatPearls Publishing.
- Wilson JE, Mart MF, Cunningham C, Shehabi Y, Girard TD, et al. (2020) Delirium. Nat Rev Dis Primers 6(1): 90.
- Simone MJ, Tan ZS (2011) The role of inflammation in the pathogenesis of delirium and dementia in older adults: a review. CNS Neurosci Ther 17(5): 506-513.
- Tierney S, Lawlor PG (2017) Clinical assessment and management of delirium in the palliative care setting. Drugs 77(15): 1623-1643.
- Arumugam S, El-Menyar A, Al-Hassani A, Strandvik G, Asim M, et al. (2017) Delirium in the intensive care unit. Journal of emergencies, trauma, and shock, 10(1): 37-46.
- Malas N, Brahmbhatt K, McDermott C, Smith A, Ortiz AR, et al. (2017) Pediatric delirium: evaluation, management, and special considerations. Current psychiatry reports 19(9): 1-14.
- Grover S, Avasthi A (2018) Clinical practice guidelines for management of delirium in elderly. Indian journal of psychiatry 60(Suppl 3): S329.
- Echeverría MDLR, Paul M, Doerr C (2021) Delirium (Nursing). In: StatPearls. StatPearls Publishing.
- Eurelings LS, de Jonghe JF, Kees JK, Piet E, Joost W, et al. (2010) Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA 304(4): 443-451.
- Saczynski JS (2014) Delirium in elderly people. Lancet 383(9920): 911-922.
- House AO, Holmes JD (2006) Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing 35(4): 350-364.
- Grover S, Avasthi A (2018) Clinical Practice Guidelines for Management of Delirium in Elderly. Indian J Psychiatry 60(Suppl 3): S329-S340.
- Beck EJ, Hetmann F (2020) Promoting Sleep in the Intensive Care Unit. SAGE Open Nurs 6: 2377960820930209.
- García SM, Brítez L, Crespo N, Udina C, Pérez LM, et al. (2020) The role of physical exercise and rehabilitation in delirium. Eur Geriatr Med 11(1): 83-93.
- Rosenbloom-Brunton DA, Henneman EA, Inouye SK (2010) Feasibility of family participation in a delirium prevention program for hospitalized older adults. J Gerontol Nurs 36(9): 22-33.
- Page VJ, Ely EW, Gates S, Zhao XB, Alce T, et al. (2013) Effect of intravenous haloperidol on the duration of delirium and coma in critically ill patients (Hope-ICU): a randomised, double-blind, placebo-controlled trial. Lancet Respir Med 1(7): 515-523.
- Neufeld KJ, Yue J, Robinson TN, Inouye SK, Needham DM (2016) Antipsychotic Medication for Prevention and Treatment of Delirium in Hospitalized Adults: A Systematic Review and Meta-Analysis. J Am Geriatr Soc 64(4): 705-714.
- Aung Thein MZ, Pereira JV, Nitchingham A, Caplan GA (2020) A call to action for delirium research: Meta-analysis and regression of delirium associated mortality. BMC Geriatr 20(1): 325.
- Hua Y, Chen S, Xiong X, Lin C, Li D, et al. (2022) Risk factors for postoperative delirium in elderly urological patients: A meta-analysis. Medicine (Baltimore) 101(38): e30696.
- Galyfos GC, Geropapas GE, Sianou A, Sigala F, Filis K (2017) Risk factors for postoperative delirium in patients undergoing vascular surgery. J Vasc Surg 66(3): 937-946.
- Edelstein DM, Aharonoff GB, Karp A, Capla EL, Zuckerman JD, et al. (2004) Effect of Postoperative Delirium on Outcome after Hip Fracture. Clinical Orthopaedics and Related Research 422: 195-200.
- Rizk P, Morris W, Oladeji P, Huo M (2016) Review of postoperative delirium in geriatric patients undergoing hip surgery. Geriatr Orthop Surg Rehabil 7(2): 100-105.
- Bickel H, Gradinger R, Kochs E, Förstl H (2008) High risk of cognitive and functional decline after postoperative delirium. A three-year prospective study. Dement Geriatr Cogn Disord 26(1): 26-31.
- Ayob F, Lam E, Ho G, Chung F, El-Beheiry H, et al. (2019) Pre-operative biomarkers and imaging tests as predictors of post-operative delirium in non-cardiac surgical patients: a systematic review. BMC Anesthesiol 19(1): 25.
- Gracie TJ, Caufield-Noll C, Wang NY, Sieber FE (2021) The Association of Preoperative Frailty and Postoperative Delirium: A Meta-analysis. Anesth Analg 133(2): 314-323.
- Iglseder B, Frühwald T, Jagsch C (2022) Delirium in geriatric patients. Wien Med Wochenschr 172(5-6): 114-121.
- Kurisu K, Miyabe D, Furukawa Y, Osamu S, Kazuhiro Y (2020) Association between polypharmacy and the persistence of delirium: a retrospective cohort study. BioPsychoSocial Med 14(25).
- Hshieh TT, Inouye SK, Oh ES (2018) Delirium in the Elderly. Psychiatr Clin North Am 41(1): 1-17.
- Inouye SK, Westendorp RG, Saczynski JS (2014) Delirium in elderly people. The Lancet 383(9920): 911-922.
- Bottino CMC, de Pádua AC, Smid J, Areza-Fegyveres R, Novaretti T Working Group on Alzheimer’s Disease and Vascular dementia of the Brazilian Academy of Neurology (2011) Differential diagnosis between dementia and psychiatric disorders: Diagnostic criteria and supplementary exams. Recommendations of the Scientific Department of Cognitive Neurology and Aging of the Brazilian Academy of Neurology. Dement Neuropsychol 5(4): 288-296.
- Griswold KS, Del Regno PA, Berger RC (2015) Recognition and Differential Diagnosis of Psychosis in Primary Care. Am Fam Physician 91(12): 856-63.
- Saunders K, Brain S, Ebmeier KP (2011) Diagnosing and managing psychosis in primary care. Practitioner 255(1740): 17-20 P. 2-3.
- Johnson J, Sims R, Gottlieb G (1994) Differential diagnosis of dementia, delirium and depression. Implications for drug therapy. Drugs Aging 5(6): 431-445.






























