Mexican Sphenoid Sinus Radiological Anatomy: High Risk Anatomy for Endoscopic Endonasal Skull Base Surgery
Agustín Dorantes-Argandar1,2,4*, Luis Pérez-García1,2, Flavio Rodas-Berrezueta1,2, Juan Pablo Ichazo-Castellanos1,2, Antonio Tovar-Díaz3, Christian Janis Sandoval-Ramírez3, Victor Ramzes Chavez-Herrera3 and Berenice García-Guzmán1,2,4
1Center for Cranial Base and Minimally Invasive Neurosurgery, Hospital Angeles Pedregal, Centro de Especialidades Quirúrgicas, Ciudad de México, México
2Surgical Neuroanatomy Laboratory, Facultad Mexicana de Medicina, Universidad La Salle, Ciudad de Mexico, México
3Neurosurgery Department, Hospital de Especialidades, Centro Médico Nacional Siglo XXI, Instituto Mexicano del Seguro Social, Ciudad de México, México
4Pituitary Clinic, Neurospecialties Group, Hospital Angeles Pedregal, Centro de Especialidades Quirúrgicas, Mexico
Submission: January 24, 2023; Published: February 03, 2023
*Corresponding author: Agustín Dorantes-Argandar, Professor of Skull Base and Minimally Invasive Neurosurgery, Center for Cranial Base and Minimally Invasive Neurosurgery, Pituitary Clinic, Neurospecialties Group, Hospital Angeles Pedregal, Centro de Especialidades Quirúrgicas, Surgical Neuroanatomy Laboratory, Facultad Mexicana de Medicina, Universidad La Salle, Ciudad de Mexico, México
How to cite this article: Agustín Dorantes-Argandar, Luis Pérez-García, Flavio Rodas-Berrezueta, Juan Pablo Ichazo-Castellanos, Antonio Tovar-Díaz, et al. Mexican Sphenoid Sinus Radiological Anatomy: High Risk Anatomy for Endoscopic Endonasal Skull Base Surgery. Open Access J Neurol Neurosurg 2023; 17(5): 555973.DOI: 10.19080/OAJNN.2023.17.555973.
Abstract
Background: We present a detailed description of the radiological anatomy of the sphenoid sinus and neurovascular structures that surround it from an endoscopic endonasal skull base surgical perspective and in an exclusively Mexican patient population.
Methods: We performed a cross-sectional study of 500 patients form the Neurosurgery Patient Database at the Specialties Hospital of the 21st Century National Medical Center. Inclusion criteria were minimum age of 18 years old, availability of fine cut CT with skull base reconstruction, absence of skull base pathology, trauma, and radiological artifacts or distortion at the area of study.
Results: These 500 patients have a sphenoid sinus with predominant sagittal post-sellar type and coronal pre-rotundum type pneumatization patterns, single intrasinus septae with predominant posterior insertion over the internal carotid arteries, intrasinus non visible carotid artery prominences, thinned carotid canal bony thickness, intrasinus non visible optic nerve prominences, and thinned optic canal bony thickness.
Conclusion: Our study suggests that Mexican patients have a well pneumatized sphenoid sinus with few visible neurovascular landmarks and thin bone coverings over the internal carotid arteries and optic nerves. This may increase the risk for optic nerve or internal carotid artery injury during endonasal transsphenoidal surgery. We believe this information will be useful for effective preoperative planning and safe surgical execution during endoscopic endonasal skull base surgery in Mexican patients.
Keywords: Endoscopic Endonasal Surgery; Mexican; Skull Base; Sphenoid Sinus; Transsphenoidal Surgery; Anatomy
Abbreviations: CT: Computed Tomography; ICA: Internal Carotid Artery; OC: Optic Canal; cor IPS: coronal Inferior Presellar Diameter; cor ISS: Coronal Inferior Subsellar Diameter; cor SPS: coronal Superior Presellar Diameter; sag IPS: Sagittal Inferior Presellar Diameter; sag ISS: sagittal Inferior Subsellar Diameter; sag SPS: sagittal Superior Presellar Diameter; vid-rot: direct oblique distance between the vidian canal and foramen rotundum
Introduction
From an endoscopic endonasal surgical perspective, the sphenoid sinus is the entry point into the sellar region, cavernous sinus, Meckel´s cave, temporal fossa, infratemporal fossa, suprasellar region, anterior floor of the skull base, posterior fossa and cranio-vertebral junction. Inside the sphenoid sinus there are several normal anatomic variations that can make a surgery simpler or more challenging [1-6]. Not taking them into account may lead to serious complications [7,8]. This sinus is present at birth as a minuscule cavity and most of its development occurs after puberty. In early age it extends posteriorly towards the presellar region and subsequently expands to below and behind the sella turcica reaching its maximum size during adolescence [9,10]. It’s pneumatization pattern, precise location of anatomic references and neurovascular relationships are of the upmost importance during endonasal transsphenoidal surgery. Slight deviations of just a few millimeters may result in unfavorable outcomes [11-16].
Sphenoid sinus pneumatization in the sagittal plane is classified into four different types: conchal, presellar, sellar, and postsellar [9, 17-20]. In the conchal type, sinus pneumatization is minimal. In the presellar type, sinus pneumatization is intermediate with the presence of a presellar recess and absence of a clival recess. In the sellar type, pneumatization is extensive with the presence of presellar and clival recesses. In the postsellar type, pneumatization is the most extensive with the presence of presellar, clival and retrosellar recesses. Sphenoid sinus pneumatization in the coronal plane is classified into three different types: pre-vidian, pre-rotundum, and post-rotundum [21]. In the pre-vidian type, pneumatization extends from the midline to the medial border of the vidian canal. In the pre-rotundum type, pneumatization extends from the midline to the lateral border of the foramen rotundum. In the post-rotundum type, pneumatization extends from the midline to past the lateral border of the foramen rotundum.
It has been documented that sphenoid sinus pneumatization in the sagittal and coronal plane are directly related, meaning that pterygoid process and clival pneumatization are codependent. These different degrees of pneumatization have specific surgical implications [21]. According to the specific pathology we aim to treat, besides the pneumatization pattern, there are several other important anatomical factors that are best to observe and determine preoperatively in order to further our opportunity for a good outcome. These include the existence and insertion of intrasinus septae, the relationship between the internal carotid arteries and the sphenoid sinus, the relationship between the optic nerves and the sphenoid sinus, and the relationship between the vidian and maxillary nerves and the sphenoid sinus [22-28]. In this article we present our radiological findings relevant for a safe and effective execution of endonasal transsphenoidal skull base surgery in Mexican patients. It is of the upmost importance that we consider this information in every case in order to offer the best surgical care for our patients.
Materials and Methods
Study Design and Cohort
We performed a cross-sectional study of 500 patients from the Neurosurgery Department Patient Database of the Specialties Hospital at the 21st Century National Medical Center in Mexico City. Inclusion criteria were patients with minimal age of 18 years, availability of fine cut head CT (1mm separation) and skull base reconstruction, absence of skull base pathology, trauma, radiological artifacts, or distortion at the area of study. This study was done with approval of the corresponding institution.
Measurements
Digital images were analyzed using the Xero Viewer Software 8.1.2 (AGFA, Belgium). Sphenoid sinuses were examined in a dynamic fashion, using axial, coronal, and sagittal projections in every one of the patients. In the sagittal plane the degree of pneumatization was classified as conchal, presellar, sellar, and postsellar. In the coronal plane the degree of pneumatization was classified as pre-vidian, pre-rotundum, and post-rotundum. Measurements included vidian canal and foramen rotundum localization, distance between the midline and the vidian canal, distance between the midline and the foramen rotundum, existence and insertion of intrasinus septae, degree of prominence of the internal carotid arteries into the sphenoid sinus, bony thickness and presence of bone dehiscence over the carotid prominences, degree of prominence of the optic nerves into the sphenoid sinus, bony thickness and presence of bone dehiscence over the optic nerves, and sphenoid sinus diameter, height, and depth. All images were analyzed by two independent observers.
Statistical Analysis
Statistical Analysis was done with IBM SPSS (International Business Machines Corporation, Armonk, New York, USA).
Results
Sphenoid Sinus Pneumatization
Pneumatization was classified on the sagittal plane in conchal, presellar, sellar, and postsellar types. In the coronal plane, pneumatization was classified in pre-vidian, pre-rotundum, and post-rotundum types.
Sphenoid sinus sagittal conchal type (1.8%): the presellar recess was minimal, the clival recess was absent and the optic nerve, pituitary gland, and internal carotid artery paraclinoid and clival prominences were not identifiable from within the sphenoid sinus. The thickness of bone that separated the pituitary gland from the sphenoid sinus was at least 10mm. This type of sphenoid sinus is not a contraindication for endonasal transsphenoidal surgery but due to the absence of clear anatomical landmarks we recommend the use of some type of neuronavigation for the identification of specific critical neurovascular structures.
Sphenoid sinus sagittal presellar type (17.2%): the pneumatization is evident in the presellar recess but it does not extend past a vertical plane parallel to the anterior sellar wall. Optic canal protrusions can be appreciated in the superolateral aspects of the presellar recess, the pituitary gland protrusion or anterior sellar wall can be observed in the central portion of the recess, and internal carotid artery paraclinoid segment protrusions can be identified in the lateral aspects of the recess. There is no clival recess and the internal carotid artery paraclival segment protrusions cannot be identified from within the sinus.
Sphenoid sinus sagittal sellar type (19.2%): the pneumatization extends from the presellar recess, past the body of the sphenoid bone and below the sellae turcica to reach the clivus. Due to the higher degree of pneumatization it is easier to identify the optic nerve protrusions, pituitary gland, paraclinoid and paraclival internal carotid artery segments. As well as the medial and lateral optic-carotid recesses, middle clinoid recess, sphenoid limbus, and tuberculum sellae recess.
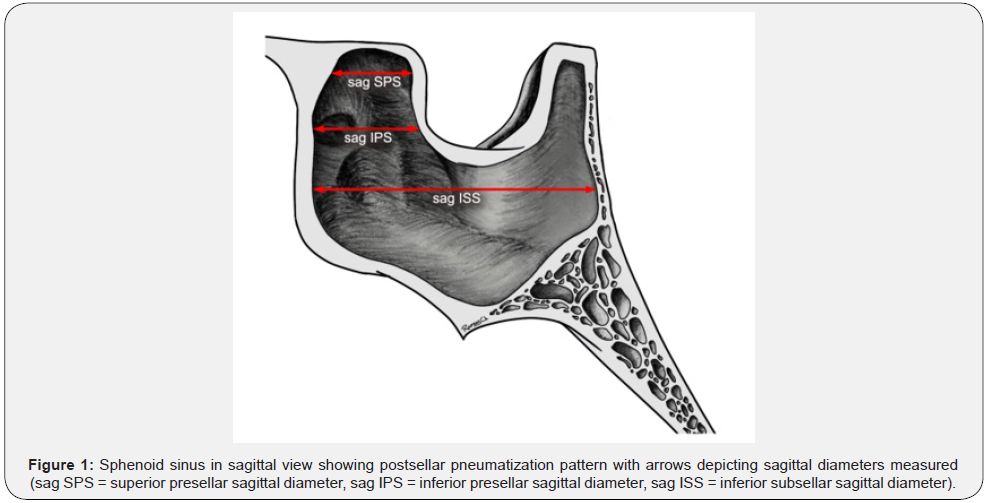
Sphenoid sinus sagittal post-sellar type (60.3%): the degree of pneumatization includes that of the sellar type and extends posteriorly past a vertical plane parallel to the dorsum sellae, creating a retrosellar recess. This recess may extend from the dorsum sellae to the posterior clinoid processes and even the superior portion of the occipital bone. Most protrusions and recess are readily identified (Figure 1).
Sphenoid sinus coronal pre-vidian type (7.8%): the pterygoid recess is absent and the vidian canal and maxillary nerve protrusions cannot be identified from within the sinus. It is necessary to perform a wide opening of the pterygopalatine fissure and transect the sphenopalatine and palatosphenoidal arteries in able to identify the vidian nerve when it emerges from the vidian canal. The foramen rotundum localized at the superolateral margin of the pterygopalatine fissure can only be identified after drilling of this area. As one advances on depth, extensive bone drilling is required to expose the internal carotid artery paraclival segment, foramen lacerum, Meckel´s cave, foramen ovale and anterolateral middle fossa triangle (between the maxillary and mandibular nerves). In these cases, it may be necessary to sacrifice the vidian nerve.
Sphenoid sinus coronal pre-rotundum type (66.1%): the pterygoid recess is partially pneumatized and one may identify the vidian canal in the floor of the pterygoid recess and the prominence of the maxillary nerve in the superolateral aspect of the recess. It is easier to identify the internal carotid artery paraclival segment and less bone removal is required to expose Meckel`s cave, foramen ovale and the anterolateral triangle of the middle fossa.
Sphenoid sinus coronal post-rotundum type (24.6%): the pterygoid recess is extensively pneumatized and it is simple to identify the vidian canal in the medial portion of the floor of the pterygoid recess and the maxillary nerve prominence in the superolateral aspect of the recess. Pneumatization extends to the pterygoid body and greater wing of the sphenoid. After access to the pterygopalatine fissure is achieved, minimal bone removal is required to open the anterior wall of the pterygoid recess. At this point only a thin layer of bone must be removed in order to access Meckel´s cave, foramen ovale, and the anterolateral triangle of the middle fossa. In these cases, the vidian nerve may be preserved.
From a surgical endonasal transsphenoidal perspective, the vidian canal localizes the petrosal segment of the internal carotid artery, with the transition from petrosal to paraclival segments projecting medial to the crossing of the vidian nerve. In a surgical access to the middle cranial fossa, the maxillary nerve (V3) defines the inferior limit of the anteromedial triangle and the super limit of the anterolateral triangle of the middle fossa.
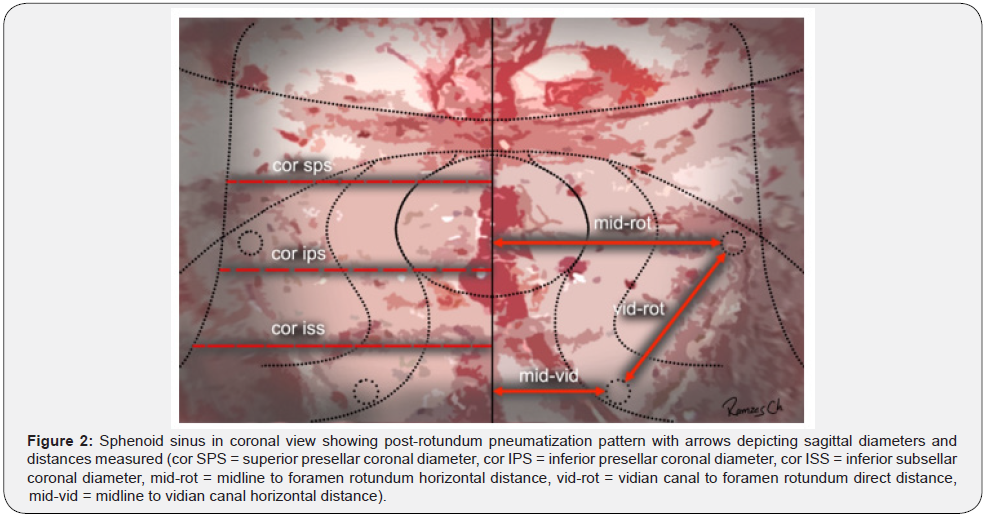
Sphenoid Sinus Diameters
Our patient population sphenoid sinus measurements on the sagittal plane correspond to an anteroposterior superior presellar (sag SPS) mean diameter of 13.09mm, inferior presellar (sag IPS) mean diameter of 17.21mm and inferior subsellar (sag ISS) mean diameter of 22.62mm. On the coronal plane diameters from side to side correspond to a latero-lateral superior presellar (cor SPS) mean diameter of 20.87mm, inferior presellar (cor IPS) mean diameter of 27.78mm, and inferior subsellar (cor ISS) mean diameter of 34.26mm. Sphenoid sinus height or superior-inferior presellar diameter correspond to a median of 24.54mm. Horizontal distance between the midline and the me-dial border of the vidian canal (mid-vid) was a mean of 11.20mm for the right side and 11.96 for the left side. Horizontal distance between the midline to the medial border of the foramen rotundum (mid-rot) was a mean of 16.44mm for the right side and 17mm for the left side. Direct oblique distance between the vidian canal and foramen rotundum (vid-rot) was a mean of 6.35mm on the right side and 6.51mm on the left side. The foramen rotundum was located 3.95mm superior and 3.68mm lateral to the vidian canal on the right side and 4.04mm superior and 4.03mm lateral to the vidian canal on the left side (Figure 2).
Intrasinus Septae
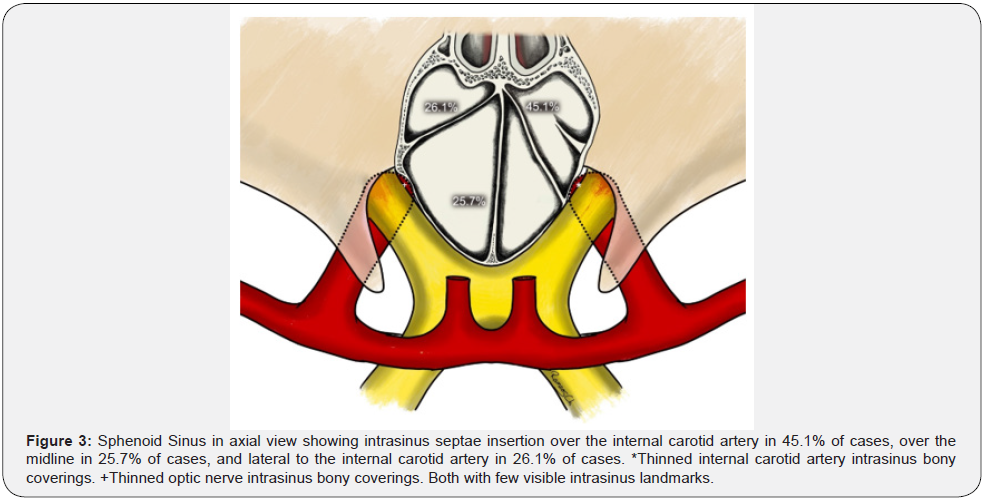
In our series we found that intra sinus septae occur in 94.8% of all sinuses, 41.7% as a single septae, 21.4% as two septations, and 31.7% as multiple septations. In 45.1% of all cases this septae insert themselves at some area of bone over the internal carotid arteries and 25.7% over the sellar prominence. We also found that they may even insert themselves onto the lateral sinus wall in 26.1% of cases.
Relationship between the Internal Carotid Arteries and the Sphenoid Sinus
Due to the importance of preoperative planning during every one of our cases, it is part of our standard preoperative protocol to identify and classify the relationship between the internal carotid artery and the sphenoid sinus. We define the relationship of the internal carotid artery (ICA) as “lateral non visible” when we do not observe a carotid artery prominence, as “visible ICA” when we can observe a carotid artery prominence but it has less than 50% of its diameter inside the sphenoid sinus cavity, and “protruded ICA” when we can observe a carotid artery prominence and it has more than 50% of its diameter inside the sphenoid sinus cavity. We also consider very important to determine and classify the thickness of the bone that covers the internal carotid arteries. With regard to this we define as “normal carotid canal thickness” when the bone covering is 1mm or more, as “thinned carotid canal thickness” when it is from 0.5mm to 1mm, and “dehiscent carotid canal thickness” when it is less than 0.5mm.
In our series we found lateral non visible ICA in 55.9% on the right side and 60.1% on the left side; visible ICA in 30.7% on the right side, and 27.7% on the left side; protruded ICA in 12.6% on the right side, and 12% on the left side of all cases. The thickness of bone covering the internal carotid arteries was normal carotid canal thickness in 29.7% on the right side and 28.9% on the left side, thinned carotid canal thickness in 63.1% on the right side and 64.1% on the left side, and dehiscent carotid canal thickness in 7.2% on the right side and 7% on the left side of all cases. The area over the carotid prominences with less bone wall thickness was the paraclinoid segment just below and lateral to the tuberculum sellae recess.
Relationship between the Optic Nerves and the Sphenoid Sinus
As another key point of our standard preoperative protocol we identify and classify the relationship between the optic nerves and the sphenoid sinus. We define as “lateral non visible” when we do not observe an optic nerve prominence, as “visible optic nerve” when less than 50% of its diameter is inside the sphenoid sinus cavity, and “protruded optic nerve” when more than 50% of its diameter is inside the sphenoid sinus cavity. We also consider very important to determine and classify the thickness of the bone that covers the optic nerves. With regard to this we define as “normal optic canal thickness” when the bone covering is 1mm of more, as “thinned optic canal thickness” when it is from 0.5mm to 1mm, and “dehiscent optic canal thickness” when it is less than 0.5mm.
In our series we found lateral non visible optic nerve in 78.4% on the right side and 77.4% on the left side; visible optic nerve in 18% on the right side, and 17.2% on the left side; protruded optic nerve in 3.6% on the right side, and 5.4% on the left side of all cases. The thickness of bone covering the optic nerves was normal optic canal thickness in 30.5% on the right side and 30.1% on the left side, thinned optic canal thickness in 57.7% on the right side and 60.1% on the left side, and dehiscent optic canal thickness in 11.8% on the right side and 9.8% on the left side of all cases. The area over the optic nerve prominences with less bone wall thickness was the segment just lateral to the tuberculum sellae recess (Figure 3).
Discussion
At birth the sphenoid sinus is present as a minuscule cavity and most of its development occurs after puberty. In early age it extends posteriorly towards the presellar region and sub-sequentially to the area bellow and behind the sellae turcica to reach its full size after adolescence. As the sinus grows and develops through its normal pneumatization it may partially surround nearby neurovascular structures. With considerable sinus development this pneumatization may even extend to the root of the pterygoid processes, greater wing of the sphenoid, posterior clinoid processes and basilar portion of the occipital bone.
Intrasinus septations occur in a natural manner within the sphenoid sinus and these must be effectively reduced in order to fully appreciate the delicate anatomical references during an endonasal transsphenoidal surgical approach. These septae are generally flat, thin and long sheets of bone that divide the sphenoid sinus into several compartments. Around 87% of these insert themselves into some area over the paraclinoid or paraclival segments of the internal carotid arteries. When they are multiple, at least one of them will have its insertion over the arteries and they must not be taken as a reference for the midline [22,29,30,31].
The internal carotid arteries can be localized on the posterolateral aspects of the sphenoid sinus on both sides. As the sinus develops the internal carotid arteries form a prominence inside the sphenoid sinus walls. This may vary in definition and depth according to the degree of sinus pneumatization. The internal carotid arteries may not always be in direct contact with their bony prominences but may be separated from them by an extension of the cavernous sinus. The bone that separates the artery from the mucous of the sphenoid sinus is thinnest over the part of the artery just below and lateral to the tuberculum sellae. The thickness of the bone that separates the artery from the sinus is less than 0.5mm in up to 90% of cases and there are close to 10% of cases that may have a dehiscence of this bony covering, leaving only a layer of periosteum and sphenoid mucous lining separating the internal carotid arteries from the sinus air cavity [32-36].
The optic canals are localized at the superior-lateral aspect of the sphenoid sinus on both sides. As the sinus develops the optic nerves form prominences within the wall of the sphenoid sinus. These also vary in depth and definition according to the degree of sinus pneumatization. In approximately 80% of cases the thickness of the bone that covers the optic nerves and sheaths inside the sphenoid sinus is less than 0.5mm and that there are also areas where there is no bone separating the optic sheaths from the sphenoid sinus mucosa [37-42].
Different ethnicities appear to have different specific anatomic variations. Anusha, et al. [43] performed a cross-sectional study in which they analyzed 300 CT scans of the brain, paranasal sinuses and head and neck area at a tertiary referral center in Malaysia. Their data showed a predominance of a sellar sphenoid sinus pneumatization pattern (93%), single intersphenoid septum (53.7%), low frequency of optic nerve dehiscence (7%) and optic nerve protrusion (2.3%), as also, rare carotid artery dehiscence (3%) and carotid artery protrusion (10%). They refer to their results as an optic nerve protrusion rate lower in southeast Asian population and optic nerve dehiscence, internal carotid artery dehiscence and internal carotid artery protrusion within international averages. Badia, et al. [44] Analyzed 200 CT scans of the paranasal sinuses in 100 Caucasian patients in London and 100 Chinese patients in Hong Kong with results that suggest that Chinese ethnicity may have a higher incidence of concha bullosa, paradoxical bending of the middle turbinate, presence of spheno-ethmoidal cells and ethmoidal roof asymmetry. They found no difference with regard to septations adjoining the internal carotid artery on the lateral sinus wall or in the exposure of the optic nerve within the sphenoid sinus. Hiremath, et al.45 Analyzed the paranasal sinus CT scans of 500 Indian patients and report a predominance of “complete sellar” (post-sellar) sagittal pneumatization pattern (76.6%), with a clival type extension (76.6%), and a “pterygoid” (pre-rotundum) coronal pneumatization pattern (52.4%).
They suggest a proportional increase of internal carotid artery and optic nerve protrusions and degree of bony thinning of the adjacent neurovascular structures bone coverings in relationship to a greater degree of sphenoid sinus pneumatization. Also they report a statistical difference in sphenoid sinus pneumatization patterns with regard to Caucasian and East Asian populations. Lu, et al.46 Retrospectively studied sphenoid sinus high resolution CT images in 200 Chinese individuals and report a predominance of a “sellar” sagittal sphenoid sinus pneumatization pattern (65.5%) and “full lateral” (post-rotundum) coronal sphenoid sinus pneumatization extension pattern (41.6%). They describe a “clival extension” (post-sellar) sagittal sphenoid sinus pneumatization pattern in only 21.4% of cases and a “pterygoid” (pre-rotundum) coronal sphenoid sinus pneumatization extension pattern in 37.2%. Their study suggests that Chinese individuals may have different sphenoid sinus pneumatization patterns compared to Caucasians and also may exhibit a higher anterior gasification rate with easily identifiable anterior neurovascular structures but poor lateral and posterior gasification rates with difficult identification of vidian canals, V2 prominences and petrous internal carotid arteries. Tawfik, et al.47 Performed a cross-sectional study of sinonasal computed tomography of the sphenoid sinus in 500 adult Egyptians. They report a predominance of “sellar” sagittal sphenoid sinus pneumatization pattern (96.8%) and “lateral recess” (post-rotundum) coronal sinus pneumatization pattern (31.8%) with a single intersphenoid septum (85.2%). They also report protrusions of the internal carotid arteries (8.5%), optic nerves (9.1%), vidian nerves (6.6%), and maxillary nerves (3.4%) as well as bony dehiscence over internal carotid arteries (7.2%), optic nerves (15%), vidian nerves (11.9%), and maxillary nerves (4.2%). With regards to intersphenoid septum attachment, only 7.2% had an insertion over the internal carotid arteries and only 2% over the optic nerves. This study highlights significant possible variations of surgically important anatomic structures in Egyptian patients such as a predominant sellar type sphenoid sinus, 14.6% of intrasinus septum multiplicity, 7.2% of septae insertion over the internal carotid artery, 55% of optic nerve dehiscense, and 50% of optic nerve protrusion.
International studies suggest that sphenoid sinus pneumatization patterns may vary among different ethnicities [43-47]. Predominantly, African-Americans have a “sellar” type (53.8%), Spanish people and Caucasians have a “post-sellar” type (48.2%), Asian population are “sellar” (50%) and “post-sellar” (50%), and Egyptians have mostly the “sellar” type (96.3%).48 Our study suggests that Mexican patients have a predominant “post-sellar” sagittal (60.3%) and “pre-rotundum” coronal (66.1%) sphenoid sinus pneumatization patterns. Intersphenoid septum attachments have been reported over the internal carotid arteries in up to 87% of cases22 and in our study this occurred in only 45.1% of cases, with 25% over the sellar prominence, and 26.1% over the lateral sinus wall. Neurovascular structure relationships within the sphenoid sinus are reported as internal carotid artery (ICA) dehiscence in 1.5 to 30%, internal carotid artery protrusion as high as 67%, optic nerve dehiscence in 0.7 to 30.6%, and optic nerve protrusion in 4.1 to 35.6%. Our results show an ICA bony canal dehiscence of 7.1% and a thinned ICA bony canal thickness (0.5 to1 mm of bone) of 63.1% with an ICA protrusion in 12.3% but lateral non-visible ICA (no visible ICA prominence inside the sphenoid sinus) in 58%. Dehiscent optic canal (OC) was observed in 10.8% and a thinned OC thickness (0.5 to1 mm of bone) in 58.9% with an OC protrusion of 4.5% and lateral non-visible OC (no visible OC prominence inside the sphenoid sinus) in 77.9%. In comparison to previous studies performed on different ethnicities, our study suggests that Mexican patients may also have a different sphenoid sinus configuration with specific neurovascular structure relationships. We analyzed thirty-three published reports related to sphenoid sinus radiological anatomy and compared their results with our cohort. We classified the comparison in sagittal plane sphenoid sinus pneumatization, coronal plane sphenoid sinus pneumatization, intrasinus septae characteristics and neurovascular intrasphenoid relationships.
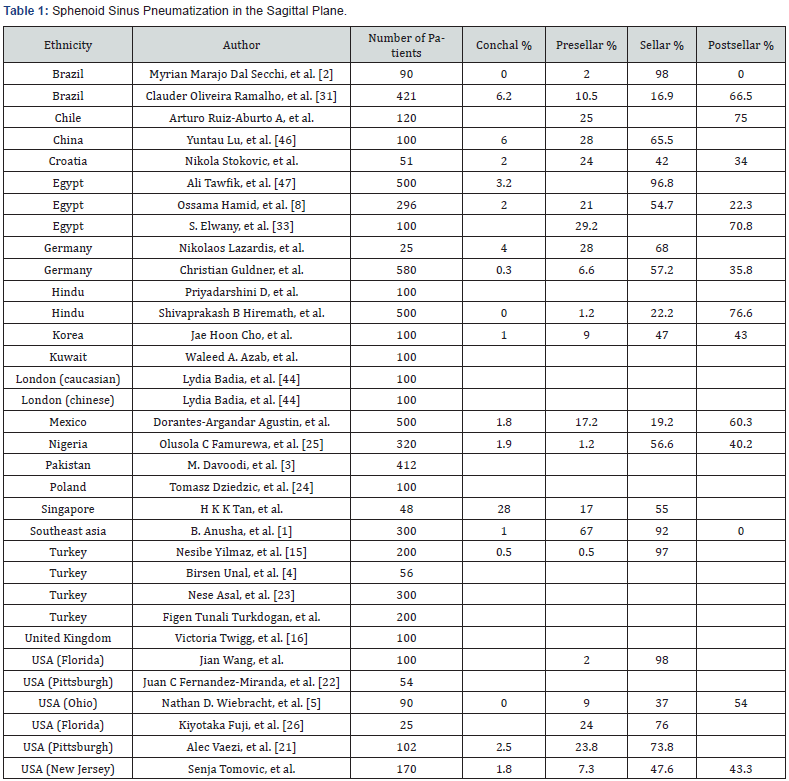
For sagittal plane sphenoid sinus pneumatization in the 33 published reports, conchal sinus type was found in 1.85%, presellar sinus type in 56.9%, and sellar sinus type in 43.15%. In our series, conchal sinus type was found in 1.8%, presellar sinus type in 17.2%, sellar sinus type in 19.2% and postsellar sinus type in 60.3%. This data suggests that Mexican patient sphenoid sinus is more pneumatized than other world populations (Table 1).
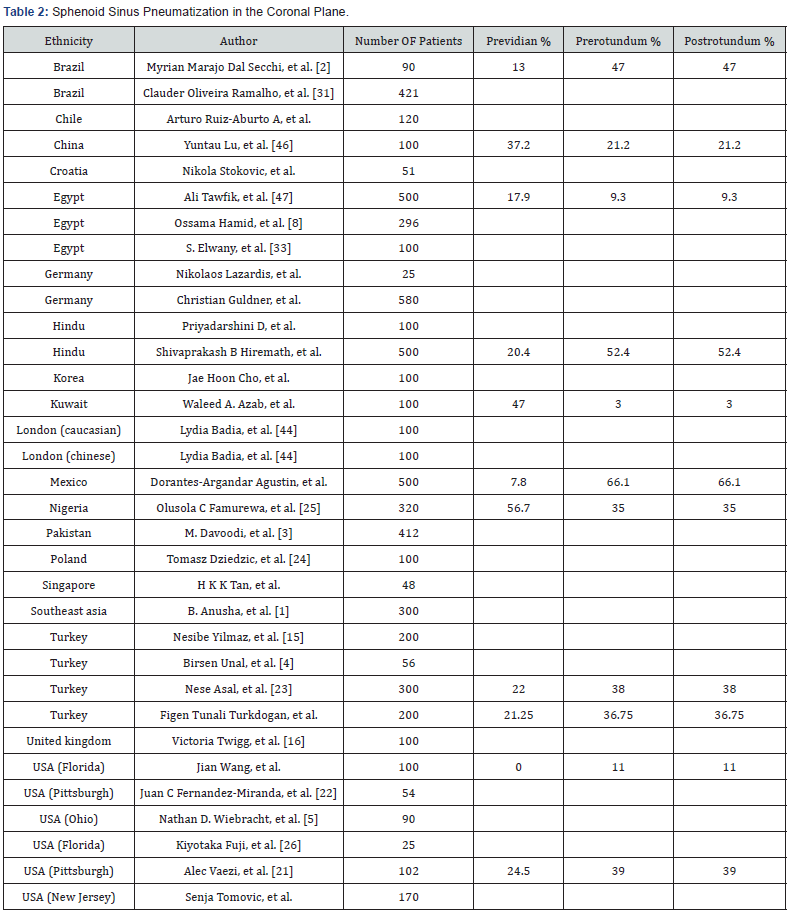
For coronal plane sphenoid sinus pneumatization in the 33 published reports, previdian sinus type was found in 21.25%, prerotundum sinus type in 36.75%, and postrotundum in 30.3%. In our series, previdian sinus type was found in 7.8%, prerotundum sinus type in 26.1%, and postrotundum sinus type in 66.1%. This data correlates with the predominant extensive postsellar pneumatization pattern found in the sagittal plane of our cohort and supports the evidence that Mexican patient sphenoid sinus is a generally more pneumatized sphenoid sinus overall (Table 2).
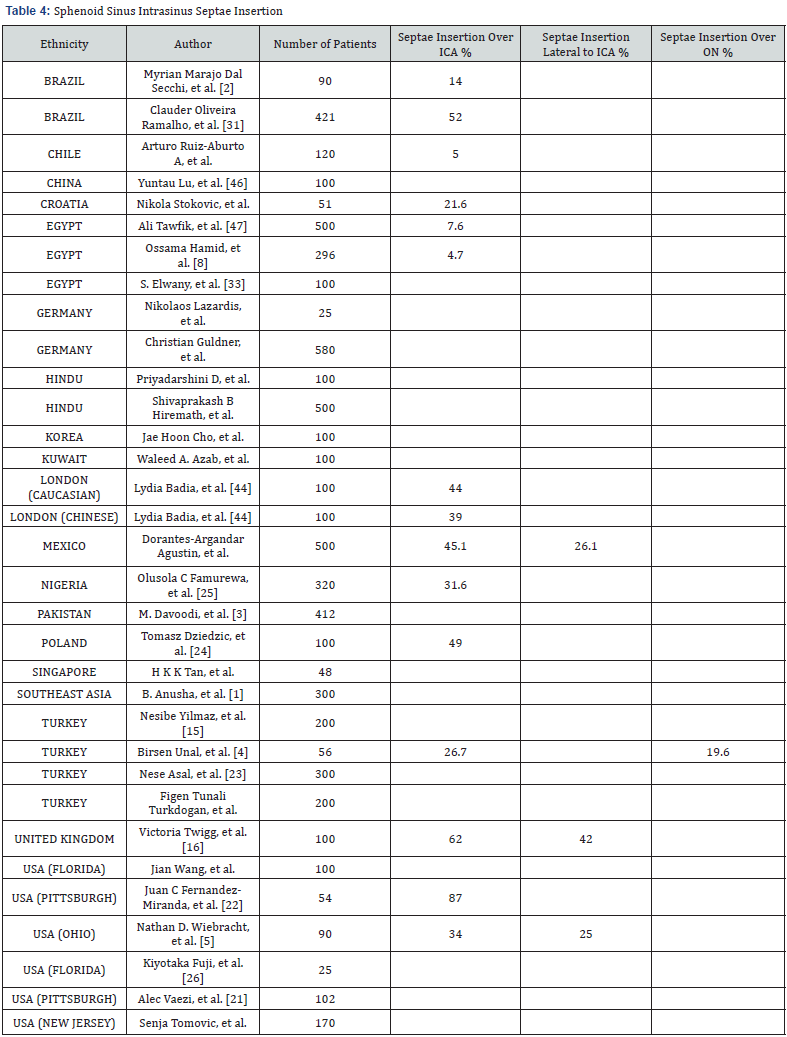
With regard to intrasinus septae, our 33-publication review resulted in a single intrasinus septae in 47.55%, multiple sinus septae in 30.34%, and septae insertion directly over de internal carotid artery in 34.8% of cases. In comparison with our series, we found single intrasinus septae in 41.7%, multiple septae in 31.7%, and direct septae insertion over the internal carotid artery in 45.1% of cases. Our data suggests that Mexican patients tend to have more frequent intrasinus septae insertion over the internal carotid artery (Table 3 & 4).

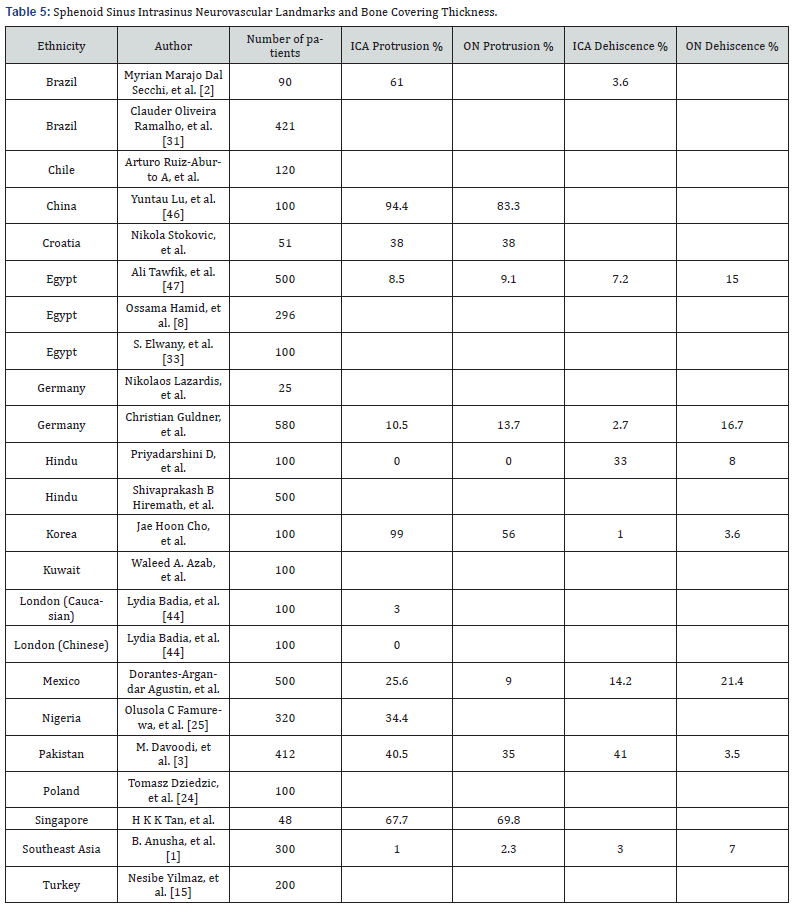
As to neurovascular intra-sphenoid sinus relationships, the 33 publication review resulted in intra-sphenoid sinus ICA protrusion in 36.7%, ON protrusion in 34.68%, ICA bony dehiscence in 11.45%, and ON bony dehiscence in 9.38%. Our series resulted in intra-sphenoid sinus ICA protrusion in 25.6%, ON protrusion in 9%, ICA bony dehiscence in 14.2%, and ON bony dehiscence in 21.4%. This comparison suggests that Mexican patient intra sphenoid sinus neurovascular relationships have a less prominent and less visible intrasinus ICA and ON landmarks, and that the bony covering over the intra sphenoid sinus ICA and ON is less thick and more dehiscent (Table 5).
Overall, with this different and varied worldwide sphenoid sinus radiological anatomy population comparison, we can suggest that Mexican patients have an extensively pneumatized sphenoid sinus, mostly single intrasinus septae, predominant septae insertion directly over the ICA, few neurovascular intrasinus visible landmarks, and greater bony dehiscence over the intrasinus ICA and ON.
Conclusion
Our study details and describes the radiological anatomy of the sphenoid sinus from an endoscopic endonasal skull base surgical perspective in an exclusively Mexican patient population. This 500 patient cross-sectional study suggests that Mexican patients have a sphenoid sinus with a predominant sagittal post-sellar type and coronal pre-rotundum type pneumatization pattern, single intrasinus septae with a predominant posterior insertion over the internal carotid arteries, intrasinus less visible internal carotid artery prominences, thinned internal carotid canal bony thickness, intrasinus less visible optic nerve prominences, and thinned optic canal bony thickness. This translates into a well pneumatized sphenoid sinus but with few visible neurovascular landmarks and thin bone coverings over the internal carotid arteries and optic nerves. These specific anatomical variations may increase the risk for optic nerve or internal carotid artery injury during endonasal transsphenoidal surgery. We believe that this information will be useful for effective preoperative planning and safe surgical execution during endoscopic endonasal skull base surgery in Mexican patients.
References
- Anusha B, Baharudin A, Philip R, Harvinder S, Shaffie BM (2014) Anatomical variations of the sphenoid sinus and its adjacent structures: a review of existing literature. Surg Radiol Anat 36(5): 419-427.
- Dal Secchi MM, Dolci RLL, Teixeira R, Lazarini PR (2018) An Analysis of Anatomic Variations of the Sphenoid Sinus and Its Relationship to the Internal Carotid Artery. Int Arch Otorhinolaryngol 22(2):161-166.
- Davoodi M, Saki N, Saki G, Rahim F (2009) Anatomical variations of neurovascular structures adjacent sphenoid sinus by using CT scan. Pak J Biol Sci 12(6): 522-525.
- Unal B, Bademci G, Bilgili YK, Batay F, Avci E (2006) Risky anatomic variations of sphenoid sinus for surgery. Surg Radiol Anat 28(2): 195-201.
- Wiebracht ND, Zimmer LA (2014) Complex anatomy of the sphenoid sinus: a radiographic study and literature review. J Neurol Surg B Skull Base 75(6): 378-382.
- Zhou D, Patil AA, Rodriguez-Sierra J (2005) Endoscopic neuroanatomy through the sphenoid sinus. Minim Invasive Neurosurg 48(1): 19-24.
- Cellina M, Gibelli D, Floridi C, Toluian T, Valenti Pittinoet C, et al. (2020) Sphenoid sinuses: pneumatisation and anatomical variants-what the radiologist needs to know and report to avoid intraoperative complications. Surg Radiol Anat 42(9):1013-1024.
- Hamid O, El Fiky L, Hassan O, Kotb A, El Fiky S (2008) Anatomic Variations of the Sphenoid Sinus and Their Impact on Trans-sphenoid Pituitary Surgery. Skull Base 18(1): 9-15.
- Rhoton AL Jr (2002) The sellar region. Neurosurgery 51(4 Suppl): S335-S374.
- Cho JH, Kim JK, Lee JG, Yoon JH (2010) Sphenoid sinus pneumatization and its relation to bulging of surrounding neurovascular structures. Ann Otol Rhinol Laryngol 119(9): 646-650.
- Lazaridis N, Natsis K, Koebke J, Themelis C, (2010) Nasal, sellar, and sphenoid sinus measurements in relation to pituitary surgery. Clin Anat 23(6): 629-636.
- Mohebbi A, Rajaeih S, Safdarian M, Omidian P (2017) The sphenoid sinus, foramen rotundum and vidian canal: a radiological study of anatomical relationships. Braz J Otorhinolaryngol 83(4): 381-387.
- Oliveira JM, Alonso MB, de Sousa E Tucunduva MJ, Fuziy A, Scocate AC, et al. (2017) Volumetric study of sphenoid sinuses: anatomical analysis in helical computed tomography. Surg Radiol Anat 39(4): 367-374.
- Peris-Celda M, Kucukyuruk B, Monroy-Sosa A, Funaki T, Valentine R, et al. (2013) The recesses of the sellar wall of the sphenoid sinus and their intracranial relationships. Neurosurgery. 73(2 Suppl Operative): 117- 131.
- Yilmaz N, Kose E, Dedeoglu N, Colak C, Ozbag D,et al. (2016) Detailed Anatomical Analysis of the Sphenoid Sinus and Sphenoid Sinus Ostium by Cone-Beam Computed Tomography. J Craniofac Surg 27(6): e549-e552.
- Twigg V, Carr SD, Balakumar R, Sinha S, Mirza S, et al. (2017) Radiological features for the approach in trans-sphenoidal pituitary surgery. Pituitary 20(4): 395-402.
- Banna M, Olutola PS (1983) Patterns of pneumatization and septation of the sphenoidal sinus. J Can Assoc Radiol. 34(4): 291-293.
- Pirinc B, Fazliogullari Z, Guler I, Unver Dogan N, Uysal II, et al. (2019) Classification and volumetric study of the sphenoid sinus on MDCT images. Eur Arch Otorhinolaryngol 276(10): 2887-2894.
- Štoković N, Trkulja V, Dumić-Čule I, Čuković-Bagić I, Tomislav Lauc T, et al. (2016) Sphenoid sinus types, dimensions and relationship with surrounding structures. Ann Anat 203: 69-76.
- Idowu OE, Balogun BO, Okoli CA (2009) Dimensions, septation, and pattern of pneumatization of the sphenoidal sinus. Folia Morphol (Warsz) 68(4): 228-232.
- Vaezi A, Cardenas E, Pinheiro-Neto C, Alessandro Paluzzi, Barton F Branstetter 4th, et al. (2015) Classification of sphenoid sinus pneumatization: relevance for endoscopic skull base surgery. Laryngoscope 125(3): 577-581.
- Fernandez-Miranda JC, Prevedello DM, Madhok R, Morera V, Barges-Coll J, et al. (2009) Sphenoid septations and their relationship with internal carotid arteries: anatomical and radiological study. Laryngoscope 119(10):1893-1896.
- Asal N, Bayar Muluk N, Inal M, Şahan MH, Doğan A, et al. (2019) Carotid canal and optic canal at sphenoid sinus. Neurosurg Rev 42(2): 519-529.
- Dziedzic T, Koczyk K, Gotlib T, Kunert P, Maj E, et al. (2020) Sphenoid sinus septations and their interconnections with parasphenoidal internal carotid artery protuberance: radioanatomical study with literature review. Wideochir Inne Tech Maloinwazyjne 15(1): 227-233.
- Famurewa OC, Ibitoye BO, Ameye SA, Asaleye CM, Ayoola OO, et al. (2018) Sphenoid Sinus Pneumatization, Septation, and the Internal Carotid Artery: A Computed Tomography Study. Niger Med J 59(1): 7-13.
- Fujii K, Chambers SM, Rhoton AL Jr (1979) Neurovascular relationships of the sphenoid sinus. A microsurgical study. J Neurosurg 50(1): 31-39.
- García-Pastor C, Moreno-Jimenez S, Gómez-Llata S (2005) Microanatomía de la región selar y paraclinoidea en especímenes mexicanos. Arch Neurocien 10(4): 212-220.
- Güldner C, Pistorius SM, Diogo I, Bien S, Sesterhenn A, et al. (2012) Analysis of pneumatization and neurovascular structures of the sphenoid sinus using cone-beam tomography (CBT). Acta Radiol 53(2): 214-219.
- Hwang SH, Joo YH, Seo JH, Cho JH, Kang JM (2014) Analysis of sphenoid sinus in the operative plane of endoscopic transsphenoidal surgery using computed tomography. Eur Arch Otorhinolaryngol 271(8): 2219-2225.
- Poirier J, Duggal N, Lee D, Rotenberg B (2011) Sphenoid sinus septations: unpredictable anatomic landmarks in endoscopic pituitary surgery. J Otolaryngol Head Neck Surg 40(6): 489-492.
- Ramalho CO, Marenco HA, de Assis Vaz Guimarães Filho F, Silva da Costa MD, Fernandes de Oliveira Santos B et al. (2017) Intrasphenoid septations inserted into the internal carotid arteries: a frequent and risky relationship in transsphenoidal surgeries. Braz J Otorhinolaryngol 83(2):162-167.
- D Priyadarshini, Prabhu LV, Kumar A, Pai MM, Kvn D (2015) The anatomical variations in the neurovascular relations of the sphenoid sinus: an evaluation by coronal computed tomography. Turk Neurosurg 25(2): 289-293.
- Elwany S, Elsaeid I, Thabet H (1999) Endoscopic anatomy of the sphenoid sinus. J Laryngol Otol 113(2): 122-126.
- Elwany S, Yacout YM, Talaat M, El-Nahass M, Gunied A, et al. (1983) Surgical anatomy of the sphenoid sinus. J Laryngol Otol. 97(3): 227-241.
- Yang Y, Zhan G, Liao J, Dang R, Wang H, et al. (2015) Morphological Characteristics of the Sphenoid Sinus and Endoscopic Localization of the Cavernous Sinus. J Craniofac Surg 26(6): 1983-1987.
- C Mutlu, HH Unlu, C Goktan, S Tarhan, M Egrilmez (2015)Radiologic anatomy of Sphenoid Sinus, analysis of 120 surgically intervened patients. Rev Chil Neurocirugía 41(1): 54-58.
- Azab WA, Abdelnabi EA, Mostafa KH, Burhamah TA, Alhaj AKH, et al. (2020) Effect of Sphenoid Sinus Pneumatization on the Surgical Windows for Extended Endoscopic Endonasal Transsphenoidal Surgery. World Neurosurg 133: 695-701.
- Enatsu K, Takasaki K, Kase K, Jinnouchi S, Kumagami H, et al. (2008) Surgical anatomy of the sphenoid sinus on the CT using multiplanar reconstruction technique. Otolaryngol Head Neck Surg 138(2): 182-186.
- García-Garrigós E, Arenas-Jiménez JJ, Monjas-Cánovas I, Abarca-Olivas J, Julián Cortés-Vela J, et al. (2015) Transsphenoidal Approach in Endoscopic Endonasal Surgery for Skull Base Lesions: What Radiologists and Surgeons Need to Know. Radiographics. 35(4): 1170-1185.
- Lee SJ (2017) The relationship of the medial roof and the posterior wall of the maxillary sinus to the sphenoid sinus: a radiologic study. Braz J Otorhinolaryngol 83(4): 375-380.
- Ucerler H, Aktan Ikiz ZA, Yoruk MD, Boduc E, Ozturk L (2020) Morphometric assessment of important landmarks on skull intended for Vidian nerve surgery. Surg Radiol Anat 42(9): 987-993.
- Wada K, Moriyama H, Edamatsu H, Hama T, Arai C, et al. (2015) Identification of Onodi cell and new classification of sphenoid sinus for endoscopic sinus surgery. Int Forum Allergy Rhinol 5(11): 1068-1076.
- Anusha B, Baharudin A, Philip R, Harvinder S, Shaffie BM, et al. (2015) Anatomical variants of surgically important landmarks in the sphenoid sinus: a radiologic study in Southeast Asian patients. Surg Radiol Anat 37(10): 1183-1190.
- Badia L, Lund VJ, Wei W, Ho WK (2005) Ethnic variation in sinonasal anatomy on CT-scanning. Rhinology 43(3): 210-214.
- Hiremath SB, Gautam AA, Sheeja K, Benjamin G (2018) Assessment of variations in sphenoid sinus pneumatization in Indian population: A multidetector computed tomography study. Indian J Radiol Imaging 28(3): 273-279.
- Lu Y, Pan J, Qi S, Shi J, Zhang X, et al. (2011) Pneumatization of the sphenoid sinus in Chinese: the differences from Caucasian and its application in the extended transsphenoidal approach. J Anat 219(2): 132-142.
- Tawfik A, El-Fattah AMA, Nour AI, Tawfik AM (2018) Neurovascular Surgical Keys Related to Sphenoid Window: Radiologic Study of Egyptian's Sphenoid. World Neurosurg 116: e840-e849.






























