Normal Pressure Hydrocephalus: Clinical Approach and Practical Considerations
Maria Alejandra Nieto-Salazar1, Adriana Carolina Toro-Velandia1, Ana Luisa Davie2, Sharima del Milagro Kanahan Osman3, Daisy Marielos Torres Treminio4, Fredy Reynaldo Pavón Enamorado5, Zulma Dorila Sosa Carcamo6, Ericka Alexandra Saldana7, Catherinne Nathaly Espinal Amaya8, Keyla Minorka Reyes Suarez9, Jeannett Maricela Anaya8, Karla Nicole Aguirre Ordóñez10, Ana Belen Brito Galvez11 and David Adrian De Leon Garza12
1Juan N Corpas University, Colombia. Larkin Community Hospital, Miami, Florida, USA
2Universidad Xochicalco, Mexico. University of Texas Health Science Center, Houston, Texas, USA
3Universidad de Carabobo, Venezuela
4Universidad Dr. Jose Matias Delgado, El Salvador
5Universidad Católica de Honduras, Honduras
6Universidad Evangélica de El Salvador, El Salvador
7Universidad Salvadoreña Alberto Masferrer, El Salvador
8Universidad de El Salvador, El Salvador
9Universidad Espíritu Santo, Ecuador
10Pontificia Universidad Católica del Ecuador, Ecuador
11Universidad de Especialidades Espíritu Santo, Ecuador
12Universidad de Monterrey, Mexico
Submission: December 20, 2022; Published: January 03, 2023
*Corresponding author: Maria Alejandra Nieto-Salazar, Juan N Corpas University, Colombia, Larkin Community Hospital, 6100 City Ave. Philadelphia, PA 19131, Miami, Florida, USA
How to cite this article: Maria A N-S, Adriana T, Ana Luisa D, Sharima K, Daisy M T T, al. Normal Pressure Hydrocephalus: Clinical Approach and Practical Considerations. Open Access J Neurol Neurosurg 2023; 17(5): 555972.DOI: 10.19080/OAJNN.2023.17.555972.
Abstract
Normal pressure hydrocephalus is defined as an abnormal cerebrospinal fluid accumulation in the ventricles. The condition is more commonly seen in the elderly population. It is present in more than 700,000 Americans between the ages of 60 - 70, but less than 20% receive an accurate diagnosis. It may be idiopathic without a known cause or the result of any circumstance that interferes with the normal cerebral spinal fluid flow (i.e., subarachnoid hemorrhage, head trauma, infection, tumor, or complications from surgery). Clinical manifestations include the presence of cognitive impairment, gait disturbance, and urinary incontinence. The diagnosis of normal pressure hydrocephalus is complex since it may present similar symptoms to those associated with other neurological conditions, particularly dementia syndromes. Therefore, a combination of classic clinical presentation, brain imaging findings, and dynamic evaluation of cerebrospinal fluid is necessary to identify this disorder. Depending on the patient’s characteristics, medical/conservative treatment or ventriculoperitoneal surgical shunting can be effective management methods. On an individual basis, the prognosis of the disease and the outcome of treatment may vary.
Keywords: Normal pressure hydrocephalus; NPH; Idiopathic hydrocephalus; Reversible dementia
Abbreviations: NPH: Normal Pressure Hydrocephalus; NINDS: National Institute of Neurological Disorders and Stroke; CSF: Cerebrospinal Fluid; ICP: Intracranial Pressure; PD: Parkinson’s Disease; AD: Alzheimer’s Disease; CT: Computed Tomography; MRI: Magnetic Resonance Imaging; iNPH: Idiopathic Normal Pressure Hydrocephalus; CNS: Central Nervous System; CVD: Cerebrovascular Disease
Introduction
The National Institute of Neurological Disorders and Stroke (NINDS) defines Normal pressure hydrocephalus (NPH) as an abnormal cerebrospinal fluid (CSF) accumulation in the ventricles. NPH can occur at any age but is more common in older people. The condition occurs if the normal flow of CSF through the brain and spinal cord is blocked in some way [1]. This causes the ventricles to enlarge, putting pressure on the brain. The term “normal pressure” could be misleading, as many patients experience fluctuations in CSF pressure that range from high to low and are variable within those parameters [1]. Many causes can lead to NPH, such as subarachnoid hemorrhage, head trauma, infection, tumor, or complications from surgery [2]. The Hydrocephalus Association estimates that more than 700,000 Americans between the ages of 60 and 70 have NPH, but less than 20% receive a proper diagnosis [2]. Since the symptoms of NPH include progressive mental decline, difficulty walking, and impaired bladder control, it is mistakenly attributed to “normal aging” or misdiagnosed with another type of dementia, such as Parkinson’s disease (PD) or Alzheimer’s disease (AD) [3]. This symptoms triad (also known as Hakim’s triad) does not need to be present to make the diagnosis. Although all the triad elements are present, ancillary tests such as cross-sectional brain imaging examinations (i.e., CT, MRI) are required to identify the presence of ventricle enlargement. Lumbar CSF extraction predicts response to shunting. When a large volume of CSF (usually 30 to 40 cc) is removed, one or more symptoms may be lessened or completely reversed. Another test that can be performed to confirm NPH is a neuropsychological test [3]. After the diagnosis is confirmed, the best treatment available for NPH is the surgical implantation of a shunt. The latter consists of a flexible tube placed in the brain’s ventricular system that diverts the CSF’s flow to another region (most often the abdominal cavity), where it can be reabsorbed [2,3]. This article aims to provide an exhaustive review of normal pressure hydrocephalus to provide a better understanding of the diagnosis and management of this complex neurological condition.
Etiology & Pathogenesis
Over the years, the term Idiopathic Normal Pressure Hydrocephalus (iNPH) has been used to refer to all individuals who present with “unexplained” ventriculomegaly detected by brain imaging, associated with a classic triad comprising cognitive impairment, gait disturbance, and urinary incontinence. Many causes can be attributed to iNPH. The most important are related to abnormal cerebrospinal fluid dynamics. It was believed to be the initiating factor contributing to the subsequent ventriculomegaly and neurological deficits in iNPH [4]. In normal conditions, CSF flow has both bulk and pulsatile components. Driven by the continuous production of CSF, the bulk flow moves from the lateral ventricles to the third ventricle through the interventricular foramen. It continues to flow across the aqueduct of Sylvius down to the fourth ventricle. Further, through the foramen of Magendie and foramen of Luschka, CSF flows to the subarachnoid space, where it is reabsorbed into blood circulation. On the contrary, CSF pulsatile flow is driven by arterial pulsatility and intracranial blood inflow. It is most prominent in the aqueduct of Sylvius, representing a rapid CSF oscillation. Two mechanisms concerning the disturbance of CSF pulsatility and normal CSF drainage have been proposed [5].
i. Increased CSF pulsatility: studies about the CSF flow in the systole and diastole phases found that the increased pulsatile flow through the aqueduct was not equally matched. The rise of CSF flow in the diastole phase exceeds that of the systole phase, causing a reversed aqueductal CSF net flow in the direction of caudal‐cranial. In addition, the retrograde aqueductal flow could generate a sustained pressure gradient that contributes to the dilation of ventricles, which is a core anatomical feature of iNPH [5].
ii. Reduced CSF drainage: the elevated resistance to CSF outflow is widely used for diagnosing iNPH and selecting candidates for shunting surgery. The retrograde jugular venous flow found in iNPH could induce transmission of high venous pressure, possibly leading to lower flow velocity at the superior sagittal sinus, which causes abnormal CSF absorption. In addition, insufficient CSF absorption caused by outflow resistance could lead to the accumulation of CSF and further facilitate the ventricular dilatation driven by high CSF pulsatility [5].
The force exerted by the CSF on the ventricles is transmitted centrifugally, which compresses the brain and elevates the transmantle pressure, i.e., the difference between ventricular pressure and the pressure over the cerebral convexity. The result is a global decrease in cerebral perfusion. Furthermore, this ventricular enlargement increases mechanical stress on the parenchyma and blood vessels, causing hypoperfusion and consequent hypoxia in iNPH [4].
Epidemiology
The prevalence of NPH is not entirely understood. In various population-based epidemiological studies across the globe, the incidence of NPH is estimated to range from 0.3 to 3% among patients over 61 years of age. There is evidence of a significant increase in NPH incidence with age [6]. According to the Alzheimer association, NPH primarily affects people in their 60s and 70s. The hydrocephalus association estimates that nearly 700,000 adults have NPH, but it is often misdiagnosed as Alzheimer’s or Parkinson’s. Less than 20% of people with the disease are adequately diagnosed [6,7].
Clinical Manifestations
Wide-based and shuffling gait is commonly the first manifestation seen in NPH. It is caused by the increased intracranial pressure producing stretching and compression of the corticospinal tract fibers in the corona radiata (lower limbs innervation), decreased white matter, and prefrontal region hypoperfusion due to the compression of brainstem structures. As the disease progresses, the gait becomes broad-based, slow, and short-stepped. Multi-step turns and gait initiation difficulty are also seen. The occurrence of gait abnormality and disequilibrium before the onset of cognitive decline has been reported to predict a better prognosis after shunting [8]. Dementia manifests with inertia, forgetfulness, and poor executive function when the ventricles enlarge and the cortex pushes against the inner table of the calvarium. Dementia is highly related to incontinence in the later stages of the disease; however, it can manifest early due to the loss of voluntary, supraspinal control of bladder contractions caused by increased intracranial pressure [8,9]. Usually, bradykinesia is the most common motor deficit. Moreover, 40% of patients with idiopathic NPH present tremors in the extremities, which typically do not respond to shunt surgery [8]. Although the evidence is scarce, idiopathic NPH can be asymptomatic, and radiological changes can be observed at least three years before symptoms onset [9].
Diagnosis
The diagnosis of NPH is considered complex because of the association with diseases with similar symptoms, such as Alzheimer’s, Parkinson, Binswanger’s disease, vascular dementia, and degenerative dystrophic spine diseases. NPH should be considered in patients with unexplained symmetric gait disturbance, a frontal subcortical pattern of cognitive impairment, and urinary urge incontinence. Ventriculomegaly is part of the suspected diagnosis, but not when it is the only sign [10,11]. The diagnosis is based on the evaluation of clinical symptoms, including Hakim’s triad, MRI assessment, CSF dynamic parameter evaluation by tap test, lumbar infusion test, and external lumbar drainage [13]. The tap test is one of the main ways to diagnose NPH and consists of a lumbar puncture with a single removal of a sufficiently large amount of CSF (30-60 ml). However, the sensitivity of the tap test is low (60%). One of the current methods for NPH diagnosis is monitoring ICP. This method consists of the implantation of a lumbar or ventricular catheter and registration of ICP for 24-72 hours [6]. The diagnostic criteria for NPH are described in Table 1.
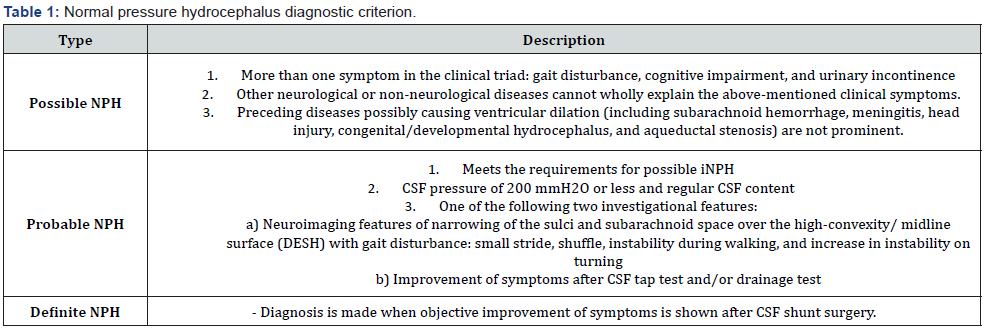
*Adapted from: Nakajima M et al. (2021) Guidelines for management of idiopathic normal pressure hydrocephalus (third edition): Endorsed by the Japanese Society of Normal Pressure Hydrocephalus. Neurologia medico-chirurgica 61(2): 63-97.
Differential diagnosis
NPH can manifest similar characteristics to other types of neurological conditions. As a result, NPH might be challenging to identify because of the overlap and/or the coexistence of different types of dementia like Alzheimer’s disease, Parkinson’s disease, dementia with Lewy Bodie’s corticobasal degeneration, and progressive supranuclear palsy [14]. NPH is commonly characterized by Hakim’s triad in addition to ventricular dilation. However, both conditions are not always present because the progression and severity are variable. The gait impairment must be present to diagnose NPH and is typically the first clinical manifestation. Patients complain of reduced speed, dizziness, and difficulty sitting down or getting up from a chair [15].
As the disease progresses, the patient may also experience challenges in daily life, such as walking, with a broad base and glue-footed gait. This characteristic differs from other types of dementia because of the absence of apraxia. In cognitive deficits, the principal affected areas are the executive function, where psychomotor slowing, short-term memory impairment, attention impairment, fine motor slowing, and imprecision are the most common [16]. Separately from reactive depression, NPH does not present psychiatric abnormalities. Thus personality changes and moods should orientate toward other types of dementia. Incontinence results from detrusor hyperactivity in NPH. Patients initially suffer from increased urinary frequency and then permanent urinary incontinence. Fecal incontinence is rare and leads to consider another type of disease [16,17]. Some clinical findings can be used to rule out NPH and arouse suspicion of a different kind of dementia, including the following:
a. People under the age of 40 years old
b. Cortical deficits
c. Intracranial pressure greater than 25 cm H2O
d. Transient symptoms or asymmetrical symptoms
e. Progressive dementia without gait impairment
Management
Medical treatment
Normal pressure hydrocephalus is one of the few causes of dementia that is potentially reversible. According to pathogenesis, pharmacological interventions such as decreasing CSF production, pulsatility, and outflow resistance could be used to normalize CSF. These measures restore blood perfusion, promote clearance of waste metabolites, alleviate neuroinflammation, and provide neuroprotection [18]. Several clinical trials have suggested that acetazolamide, a carbonic anhydrase inhibitor, reduces CSF production. Therefore, this medication is recommended for patients deemed non-surgical candidates and those who decline surgery [19]. In addition, since shunt complications are common, acetazolamide can be an effective medical alternative [20].
Surgical treatment
The surgical treatment for NPH consists of ventriculoperitoneal shunting. Recent studies have shown success rates of up to 90% after an adequate selection of patients that are surgical candidates. However, it should be noted that the shunting procedure has some complications that could be associated with significant adverse effects: subdural hematomas/hygromas, central nervous system (CNS) infection, over-drainage, prolonged postoperative delirium, and complex partial seizures. There is also a minimal chance of delayed postoperative pneumocephalus and death [19]. Clinical guidelines for surgical management in NPH were created because of the many limitations and the available evidence of the severe complications that might occur [21].
Prognosis
Over the past few years, surgical outcomes have improved. However, since pre and postoperative shunt surgery outcomes are measurable with diverse validated scales and methods (biochemical and imaging), it is not easy to compare studies. The improvement rates are as variable as 39-81% in 3-6 months to 63–84% in 1 year [13]. In addition, the recovery in the first months is lower due to short-term complications such as excessive drainage, subdural hematomas, insufficient drainage, and shunt dysfunction [22]. Cognitive improvement is known to have mixed results. Frontal lobe executive functions do not usually improve after shunt surgery. The ability to walk independently and urinary output significantly enhance the quality of life despite short-term complications. Follow-up with changes in the neuropsychological state is recommended using validated scales, gait, and MRI. The prognosis can also be affected by the duration and severity of the disease, response to tap tests, and the status of imaging findings.
Increasing age and established cerebrovascular disease (CVD) were associated with less favorable outcomes after shunt surgery. Long waiting time for shunt surgery was a negative predictor of outcome, which indicates that iNPH is a progressive neurological disorder with worsening symptoms over time [23].
Conclusion
The National Institute of Neurological Disorders and Stroke defines NPH as an abnormal CSF accumulation in the ventricles, typically occurring when its normal flow through the brain and spinal cord is blocked. Symptoms include progressive mental decline and dementia, difficulty walking, and impaired bladder control. Idiopathic Normal Pressure Hydrocephalus (iNPH) refers to all individuals who present with “unexplained” ventriculomegaly detected by brain imaging. Many causes are attributed to iNPH, being the most important related to abnormal CSF dynamics. NPH develops as increased intracranial pressure produces stretching and compression of the corticospinal tract; thus, the gait becomes broad-based, slow, and short-stepped with disease progression. The occurrence of gait abnormalities before cognitive decline has been reported to predict a better prognosis after shunting. Whereas incontinence results from detrusor hyperactivity, patients with NPH initially suffer from increased urinary frequency and then, often, permanent urinary incontinence.
Idiopathic NPH is initially asymptomatic, but radiological changes can be observed at least three years before symptom onset. NPH should be considered a diagnosis for patients with unexplained symmetric gait disturbance, a frontal subcortical pattern of cognitive impairment, and urinary urge incontinence. NPH often manifests similar aspects to other illnesses, which is why it may sometimes be challenging to detect. Diagnosis consists of implantation of a lumbar or ventricular catheter and registration of ICP for 24-72 hours. A definitive diagnosis of NPH can only be made when objective improvement of symptoms is shown after shunt surgery. Acetazolamide, a carbonic anhydrase inhibitor, has represented a medical treatment option since it has been shown to reduce the production of CSF. However, it does not provide a definitive remission. With a surgical approach, the ability to walk independently and decreased urinary symptoms significantly improve quality of life, even despite short-term complications that may present. Unfortunately, long waiting time for shunt surgery has been a negative predictor of outcome. Given this diagnosis’s significant impact on patients and their families, it is paramount to continue investigating possible measures that might aid in improving their day-to-day functioning until better treatment options are developed and available.
References
- Normal pressure hydrocephalus [Internet]. National Institute of Neurological Disorders and Stroke. U.S. Department of Health and Human Services.
- Golomb JB, Hayden S (2022) What is normal pressure hydrocephalus (NPH) [Internet]. About Normal Pressure Hydrocephalus (NPH). Hydrocephalus association.
- Normal pressure hydrocephalus. Alzheimer's Disease and Dementia.
- Oliveira LM, Nitrini R, Román GC (2019) Normal-pressure hydrocephalus: A critical review. Dementia & Neuropsychologia 13(2): 133-143.
- Wang Z, Zhang Y, Hu F, Ding J, Wang X (2020) Pathogenesis and pathophysiology of idiopathic normal pressure hydrocephalus. CNS Neuroscience & Therapeutics 26(12): 1230-1240.
- Gavrilov GV, Gaydar BV, Svistov DV, Korovin AE, Sanarcev IN, et al. (2019) Idiopathic normal pressure hydrocephalus (Hakim-Adams Syndrome): Clinical symptoms, diagnosis and treatment. Psychiatria Danubina 31(5): 737-744.
- Normal pressure hydrocephalus. Alzheimer's Disease and Dementia.
- MDas JM, BIagioni MC (2022) Home - books - NCBI [Internet]. National Center for Biotechnology Information. U.S. National Library of Medicine.
- Engel DC, Adib SD, Schuhmann MU, Brendle C (2018) Paradigm-shift: Radiological changes in the asymptomatic inph-patient to be: An observational study. Fluids and Barriers of the CNS 15(1): 5.
- Williams MA, Malm J (2016) Diagnosis and treatment of idiopathic normal pressure hydrocephalus. CONTINUUM: Lifelong Learning in Neurology 22(2, Dementia): 579-599.
- Saldarriaga CA, Yepes GV, Rivas JC (2020) Normal pressure hydrocephalus: Diagnostic delay. Biomédica 40(4): 656-663.
- Skalický P, Mládek A, Vlasák A, De Lacy P, Beneš V, et al. (2019) Normal pressure hydrocephalus-an overview of pathophysiological mechanisms and diagnostic procedures. Neurosurgical Review 43(6): 1451-1464.
- Nakajima M, Yamada S, Miyajima M, Ishii K, Kuriyama N, et al. (2021) Guidelines for management of idiopathic normal pressure hydrocephalus (third edition): Endorsed by the Japanese Society of Normal Pressure Hydrocephalus. Neurologia medico-chirurgica 61(2): 63-97.
- Ohmichi T, Tokuda T (2022) [idiopathic normal pressure hydrocephalus and neurodegenerative diseases: A short review of differential diagnosis]. No shinkei geka. Neurological surgery. U.S. National Library of Medicine 50(2): 319-330.
- Graff Radford NR, Jones DT (2019) Normal pressure hydrocephalus. CONTINUUM: Lifelong Learning in Neurology 25(1): 165-186.
- Skalický P, Mládek A, Vlasák A, De Lacy P, Beneš V, et al. (2020) Normal pressure hydrocephalus-an overview of pathophysiological mechanisms and diagnostic procedures. Neurosurg Rev. diciembre de 43(6): 1451-1464.
- Deutscher Ärzteverlag GmbH RDÄ (2012) The differential diagnosis and treatment of normal-pressure hydrocephalus.
- Wang Z, Zhang Y, Hu F, Ding J, Wang X (2020) Pathogenesis and pathophysiology of idiopathic normal pressure hydrocephalus. CNS Neuroscience & Therapeutics 26(12): 1230-1240.
- Oliveira LM, Roman GC, Nitrini R (2019) Normal-pressure hydrocephalus: A critical review. Dement Neuropsychol 13(2): 133-143.
- Del Bigio MR, Di Curzio DL (2015) Nonsurgical therapy for hydrocephalus: A comprehensive and critical review. Fluids and Barriers of the CNS 13: 3.
- Bergsneider M, Black PML, Klinge P, Marmarou A, Relkin N (2005) Surgical management of idiopathic normal-pressure hydrocephalus. Neurosurgery 57(suppl 3): S29-39.
- Gavrilov GV, Gaydar BV, Svistov DV, Korovin AE, Samarcev IN, et al. (2019) Idiopathic Normal Pressure Hydrocephalus (Hakim-Adams Syndrome): Clinical Symptoms, Diagnosis and Treatment. Psychiatr Danub 31(Suppl 5): 737-744.
- Bådagård H, Braun M, Nilsson D, Stridh L, Virhammar J (2019) Negative predictors of shunt surgery outcome in normal pressure hydrocephalus. Acta Neurologica Scandinavica 141(3): 219-225.






























