Endoscopic Transsellar Transdiaphragmatic Surgery; A Minimally İnvasive Approach for İnfundibular Lesions: A Case Series of Seven Patients
Atakan Emengen1, Eren Yilmaz2, Burak Cabuk2, Ihsan Anik2 and Savas Ceylan2*
1Department of Neurosurgery, Kocaeli State Hospital, Kocaeli, Turkey
2Department of Neurosurgery, Kocaeli University, Pituitary Research Center, Kocaeli, Turkey
Submission: May 26, 2022; Published: June 14, 2022
*Corresponding author: Savas Ceylan, Department of Neurosurgery, Kocaeli University, Pituitary Research Center, Kocaeli, Turkey
How to cite this article: Atakan Emengen, Eren Yilmaz, Burak Cabuk, Ihsan Anik, Savas Ceylan. Endoscopic Transsellar Transdiaphragmatic Surgery; A Minimally İnvasive Approach for İnfundibular Lesions: A Case Series of Seven Patients. Open Access J Neurol Neurosurg 2022; 17(2): 555958.DOI: 10.19080/OAJNN.2022.17.555958.
Abstract
The endoscopic endonasal approach provides the possibility of obtaining early devascularization in sellar, infra and supradiafragmatic and intraventricular midline lesions without neurovascular retraction or manipulation. In the last two decades, extended endoscopic transsphenoidal approaches have become increasingly common for sellar zone lesions with suprasellar extension and infundibular lesions. Besides the possibility of damage to important anatomical structures, the risk of post-operative CSF leakage is higher than in the standard approach. The diaphragma sellae is an important barrier for CSF leakage. CSF leakage is less likely to occur in surgery in which the diaphragma sellae is preserved. In small-sized suprasellar extension tumors, a window is opened in the diaphragm following the excision of the intrasellar component and the tumor component that has spread to the suprasellar area is excised from this small diaphragmatic foromen. Instead of the extended approach, we applied this intrasellar transdiaphragmatic approach to 7 patients (craniopharyngioma, metastasis, 2 acromegaly, 2 cushing disease and rathke cleft cyst) with suprasellar or infundibular lesions. We presented 4 of these patients. With this method, which is less invasive compared to the extended transsphenoidal approach, CSF leak repair can be controlled more easily and this technique is predicted to be less likely to damage the infindibulum and other important neurovascular structures.
Keywords: Infundibulum; Endoscopic surgery; Pituitary; Transdiaphragmatic
Abbreviations: CSF: Cerebrospinal Fluid; MRI: Magnetic Resonance Imaging
Introduction
The endoscopic endonasal approach provides the possibility of obtaining early devascularization in sellar, infra and supradiafragmatic and intraventricular midline lesions without neurovascular retraction, or manipulation [1,2]. This approach has facilitated the removal of skull base tumors with fewer complications than in other approaches. However, CSF leakage due to the removal of the skull base bone and duramater are important concerns [3]. In particular, giant pituitary adenomas can be successfully treated using the endoscopic approach, with higher gross total resection rates and lower mortality and recurrence rates [4-6].
In the last two decades in particular, as the popularity of endoscopic surgery has increased, extended endoscopic transsphenoidal approaches have become increasingly common for sellar zone lesions with suprasellar extension and infundibular lesions [7-10]. This technique has several difficulties. Besides the possibility of damage to important anatomical structures, the risk of post-operative CSF leakage is higher than in the standard approach [11]. It is difficult to choose a surgical approach in only infundibular lesions and tumors extending through the sella to the suprasellar area. The minimally invasive endoscopic transsellar transdiaphragmatic approach can be used in these tumors because of the widening of the diaphragmatic opening.
The aim of this article is to present our experience with the intrasellar transdiaphragmatic technique, which we use instead of the extended approach in lesions spreading from the very small infundibular opening to the suprasellar area. We also discussed the technical features, advantages and disadvantages of this approach.
As a tertiary centre, we were able to perform this transdiaphragmatic approach in a small number of cases as a result of high experience [4,8,12]. The transdiaphragmatic approach should be considered as a technique and an alternative approach that can be applied after experience in such lesions.
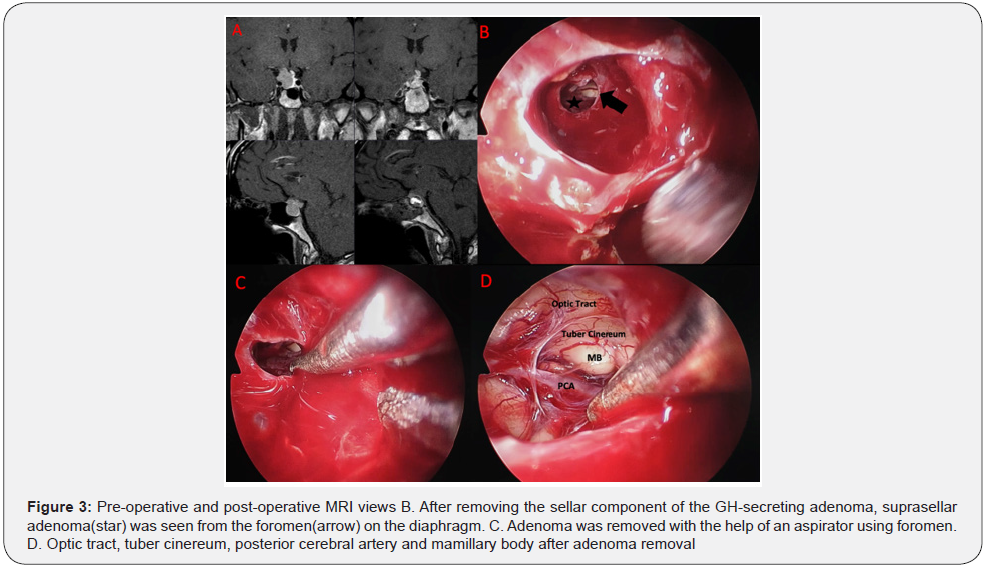
Instead of the extended approach, we applied the intrasellar transdiaphragmatic approach to 7 patients (craniopharyngioma, metastasis, 2 acromegaly, 2 cushing disease and rathke cleft cyst) (Table 1) with suprasellar or infundibular lesions. CSF leakage wasn’t observed in the follow-up of 7 patients. We presented 4 of these patients.
Illustratıve Case I
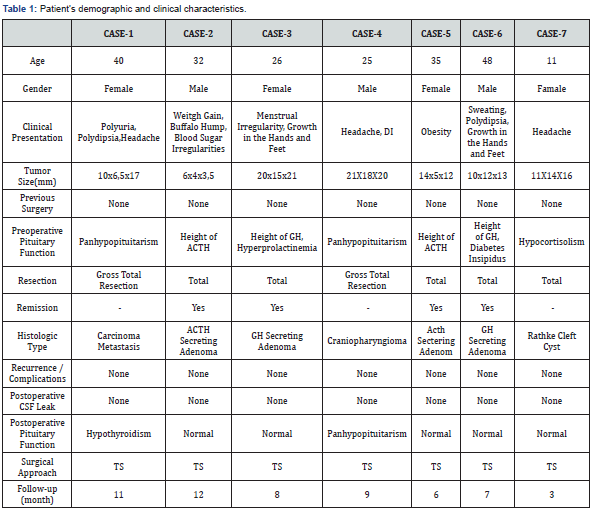
A 40-year-old female presented with headache, polyuria and polydipsia. She had a history of bilateral invasive lobular breast cancer, with surgery in 2017. After this operation and radiotherapy treatment, she was prescribed tamoxifen and luteinizing hormone-releasing hormone (LH-RH) agonists for her chemotherapy treatment (ER95%+, PR90%+, cERB2(- ), ki6510%+). During a routine PET-CT checkup, she was diagnosed with metastasis in the form of a sellar tumor. She gradually developed panhypopituitarism. She was evaluated by endocrinologists and neurosurgeons. A physical examination revealed no abnormalities. On admission, she was using rugs for panhypopituitarism and also a selective estrogen receptor modulator. A 10x6.5x17 mm homogeneously enhancing lesion was observed in the suprasellar cistern, involving the infundibulum, on magnetic resonance imaging (MRI) of the pituitary.
We performed a standard endoscopic transsphenoidal approach. After opening the duramater, we observed a metastatic lesion. A sellar component of the tumor was removed with the help of a micro-punch and curette. After this stage, a foramen of the diaphragmatic sella was seen; it was expanded with sharp dissection. The tumor extending into the suprasellar area was reached through this foramen. The tumor, which was attached to the wall of the third ventricle, was totally excised gross with the help of an ultrasonic aspirator. Then, the third ventricle walls and the basillar area were observed. The sella was closed with a multi-layer closure technique (Figure 1).
Immunohistochemical staining showed strong diffuse GATA- 3, ER, PR, and cytokeratin 7 staining, confirming the diagnosis of breast cancer metastasis. In a post-operative followup, signs of diabetes insipidus and CSF leakage were not observed. The patient was discharged to her home on postoperative day 7.
Illustratıve Case Iı
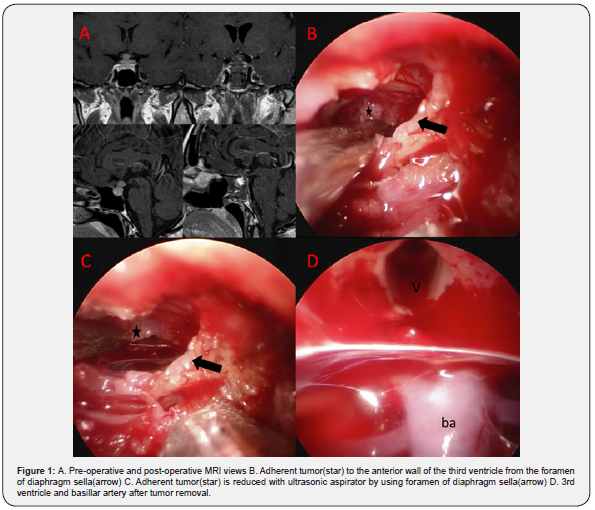
A 32-year-old male presented with weight gain, purple stretch marks on the skin of the abdomen, buffalo hump and blood sugar irregularities. Because of these symptoms, he was investigated by endocrinologists. His basal cortisol level was 25,60 μg/dl, and his ACTH level was 67.4 pg/ml. After a highdose (8 mg) dexamethasone suppression test, his morning serum cortisol level was not suppressed, and MRI prompted a diagnosis of pituitary Cushing disease. Cushing disease signs were observed on physical examination.
MRI of the pituitary showed a microadenoma in the left central part of the pituitary gland, approximately 6x4x3.5 mm in size, possibly at the level of the intermadiate lobe. These are more hypotensive in the late period dynamic contrast series compared to the parenchyma.
He underwent standard endoscopic endonasal transsphenoidal resection. Following the opening of the dura, an incision was made first into the left pituitary tissue, and the tumor tissue was excised with the help of a curette. Then an incision was made on the right side. The second tumor tissue was excised with the help of a curette and a micro-punch. During exploration of the pituitary tissue from the foramen of the diaphragm, the pituitary gland was dissected to the right, and a lobulated pathology was encountered that pushed the infundibulum to the right. Vascular malformations were ruled out with the help of Doppler ultrasound. Then, with the help of a micro-punch, the tumor tissue was excised, together with its pseudo-capsule. Exploratory surgery was employed in the operation (Figure 2).
Immunohistochemical staining showed strong diffuse ACTH and cytokeratin 8/18 staining, confirming the diagnosis of ACTHsecreting adenoma. He had post-surgical remission on the first day (cortisol: 3.44 μg/dl, ACTH <5 pg/ml). He was discharged to his home on postoperative day 6, and any complications were observed during the follow-up period.
Illustratıve Case Iıı
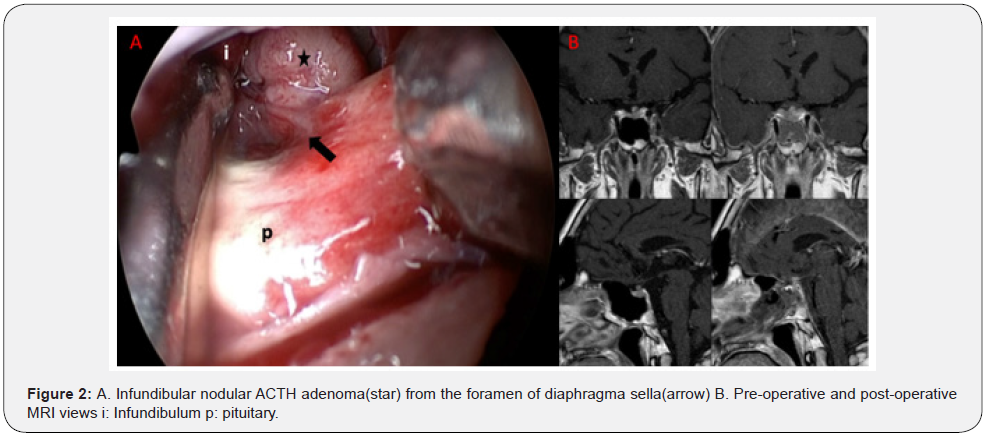
A 26-year-old female patient presented with complaints of menstrual irregularity and growth in the hands and feet. It was investigated by endocrinologists because of these symptoms. There was no abnormality in anterior pituitary hormones except growth hormone and prolactin at the time of admission. Basal Growth Hormone level was 13.9 ug/l, IGF-1 level was 599 ug/l, Prolactin level was 60 ug/l.
The patient was diagnosed with acromegaly, as 20x15x21 mm adenoma tissue was observed in the contrast enhanced sellar magnetic resonance imaging without suppression of growth hormone value by OGTT. On physical examination, the patient’s phenotype was compatible with acromegaly and there was no additional abnormality. The patient had no comorbid disease.
A craniotomy was performed from the sellar region within the sphenoid sinus with a standard endoscopic endonasal transsphenoidal approach. After the dura was opened, the sellar component was excised with a curette, punch and aspirator. Then the foromen on the diaphragmatic sella was seen. Adenoma tissue was excised from the foramen with the aid of a curette and aspirator. The sella was closed with the multilayer closure technique (Figure 3).
Immunohistochemical staining showed diffuse strong cytoplasmic GH staining confirming the diagnosis of GH secreting adenoma. A negative reaction was detected with ACTH and prolactin.
In the examinations performed on the first postoperative day of the patient, GH was 0,9 ug/l, IGF-1 was 220 ug/l, and Prolactin was 3.02 ug/l. There weren’t abnormalities in other anterior pituitary hormones. No problems were encountered in their follow-up. The patient was discharged home on the 5th postoperative day.
Illustratıve Case Iv
A 25-year-old male patient presented with headache, drinking a lot of water and urinating a lot. It was investigated by endocrinologists because of these symptoms. He had hypocortisolemia, thyroid axis disorder, hypogonadism and diabetes insipidus at the time of admission. Hormone replacement therapies were arranged by endocrinologists. Contrast-enhanced sellar magnetic resonance imaging revealed a 21x18x20 mm lesion extending to the suprasellar region. There was no additional abnormality in his physical examination and the patient did not have any comorbidities.
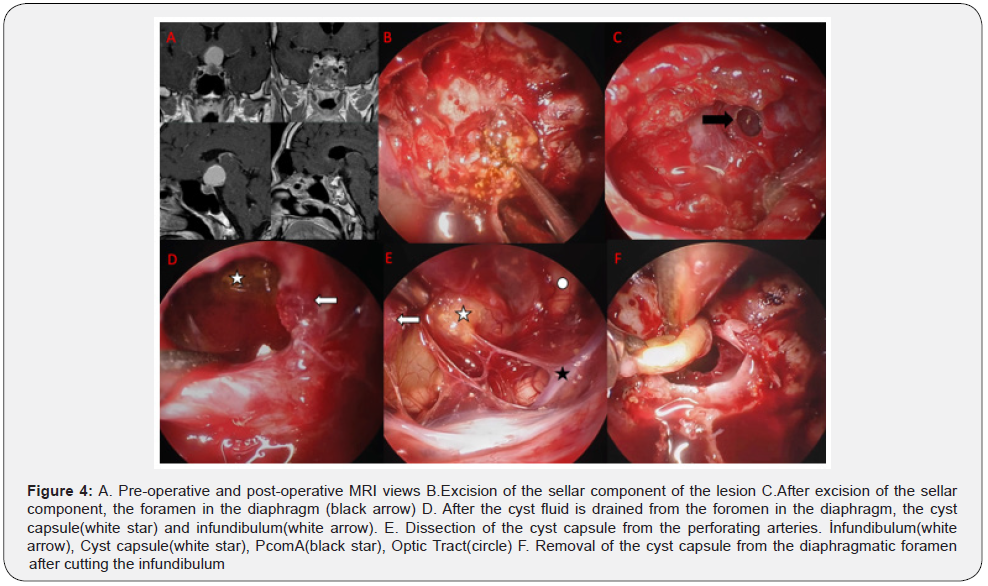
After entering the sphenoid sinus with the standard endoscopic endonasal transsphenoidal approach, the sella was reached. After the dura was opened, the dirty yellow lesion with solid components containing calcifications was evacuated with the help of a curette, punch and aspirator. After the sellar component of the lesion was excised, the foromen on the diaphragm was seen. It was observed that the infundibulum was flat. The infindibulum was cut with scissors, as total excision of the lesion that had spread to the suprasellar region of the patient with panhypopituitarism was aimed. With the aid of a curette and punch, the cyst capsule was completely excised through the opening in the diaphragm. The sella was closed with the multilayer closure technique (Figure 4).
The pathology of the lesion resulted as adamantinomatous type craniopharyngioma. The patient was discharged home on the 7th postoperative day and continued to receive hormone replacement therapy in the postoperative period (desmopressin 3x120mcg, levothyroxine 1x100mcg, hydrocortisone 2x60 mg, testosterone 3 weeks x 250 mg).
Discussion
Lesions with sellar and infundibular extension or suprasellar extension through the diaphragmatic small opening are difficult to approach. The endoscopic transnasal extended approach or the transcranial approach is usually applied to lesions that spread in this way. The transdiaphragmatic approach is an alternative to the extended and transcranial approach. This technique provides resection of an infundibular or suprasellar lesion through a small diaphragmatic foromen via the sellar route. It is a more effective method in preventing CSF leakage than the extended approach, since it is entered through a small foromen in the diaphragm.
The diaphragm sella, which acts as a barrier between the sellar content and the suprasellar area, maintains its position in small tumors [13]. However, in large, giant and suprasellar extending tumors, the diaphragma sellae is displaced and opens laterally, and the suprasellar cystern, which is thinner than the diaphragma sellae, is observed in the midline [4,14]. However, in cases where the diaphragmatic sella maintains its position, tumor resection may be possible with a standard endoscopic approach from a small defect of the diaphragmatic sella.
In the endoscopic transsphenoidal approach, for macro and giant adenomas with suprasellar extension, extracapsular excision with maneuvers applied by cleavage of the tumor after intracapsular resection is a common approach [4,15-17]. However, in these cases, a true dura mater structure is not encountered, as the diaphragm sella is displaced superiorly and laterally due to the effect of the tumor. The structure seen after tumor excision is suprasellar cistern, and because of its weak structure, high-flow CSF leakage can be seen. Although the multilayer closure technique of the skull base, the incidence of CSF leakage is high even in experienced centers [18,19].

In this approach, it is possible to excise the part extending from the very small infundibular opening to the suprasellar area from the small foromen above the diaphragm following the removal of the sellar component in small tumors with suprasellar extension. Rarely, the small foromen can be enlarged with this approach. In these lesions, after the sellar component is removed, the infundibular lesion is removed from the foromen in the diaphragm with intraoperative neuronavigation (Figure 5).
CSF leak repair can be controlled more easily with this method, which is less invasive than the extended transsphenoidal approach. And it can be seen as an alternative method for extended approaches in small-sized suprasellar extension tumors. In addition, this technique, which is more minimally invasive than the extended transsphenoidal approach, is predicted to be less likely to damage the infindibulum and other important neurovascular structures.
Conclusion
In midline lesions with intrasellar location to suprasellar extension and infundibular lesions, it is possible to make extractions through the foramen of the diaphragm sellae without the need for an extended opening with the standard endoscopic transsphenoidal approach. Thus, because of the minimally invasive surgery, complications such as CSF leaks will be less frequent and CSF leakage will be controlled more easily.
Conflict of interest
None.
Informed Consent
Informed consent was obtained from all individual participants included in this study.
References
- Koutourousiou M, Fernandez-Miranda JC, Stefko ST, Wang EW, Snyderman CH, et al. (2014) Endoscopic endonasal surgery for suprasellar meningiomas: experience with 75 patients. J Neurosurg 120(6): 1326-1339.
- de Divitiis E, Esposito F, Cappabianca P, Cavallo LM, de Divitiis O (2008) Tuberculum Sellae Meningiomas. Neurosurgery 62(3): 556-563.
- Ishikawa T, Takeuchi K, Nagata Y, Choo J, Kawabata T, et al. (2019) Three types of dural suturing for closure of CSF leak after endoscopic transsphenoidal surgery. J Neurosurg 131(5): 1625-1631.
- Ceylan S, Sen HE, Ozsoy B, Cemre Ceylan E, Ergen A, et al. (2021) Endoscopic approach for giant pituitary adenoma: clinical outcomes of 205 patients and comparison of two proposed classification systems for preoperative prediction of extent of resection. J Neurosurg 136(3): 786-800.
- Juraschka K, Khan OH, Godoy BL, Monsalves E, Kilian A, et al. (2014) Endoscopic endonasal transsphenoidal approach to large and giant pituitary adenomas: institutional experience and predictors of extent of resection. J Neurosurg 121(1): 75-83.
- McLaughlin N, Eisenberg AA, Cohan P, Chaloner CB, Kelly DF (2013) Value of endoscopy for maximizing tumor removal in endonasal transsphenoidal pituitary adenoma surgery. J Neurosurg 118(3): 613-620.
- Cavallo LM, Frank G, Cappabianca P, Solari D, Mazzatenta D, et al. (2014) The role of the endoscopic endonasal route in the management of craniopharyngiomas. World Neurosurg 121(1): 100-113.
- Ceylan S, Caklili M, Emengen A, Yilmaz E, Anik Y, et al. (2021) An endoscopic endonasal approach to craniopharyngioma via the infrachiasmatic corridor: a single center experience of 84 patients. Acta Neurochir (Wien) 163(8): 2253-2268.
- Ceylan S, Koc K, AnIk I (2011) Extended endoscopic transphenoidal approach for tuberculum sellae meningiomas. Acta Neurochir (Wien) 153(1): 1-9.
- Ceylan S, Anik I, Koc K, Cabuk B (2015) Extended endoscopic transsphenoidal approach infrachiasmatic corridor. Neurosurg Rev 38(1): 137-147.
- De Divitiis E, Cavallo LM, Esposito F, Stella L, Messina A (2008) Extended endoscopic transsphenoidal approach for tuberculum sellae meningiomas. Neurosurgery 62(6 SUPPL.): 23-26.
- Ceylan S, Anik I, Cabuk B, Caklili M, Anik Y (2019) Extension Pathways of Pituitary Adenomas with Cavernous Sinus Involvement and Its Surgical Approaches. World Neurosurg 127: e986-e995.
- Rhoton A (2002) The sellar region. Neurosurgery 51(4 Suppl): S335-S374.
- Cabuk B, Anik I, Kokturk S, Ceylan S, Ceylan S (2020) Anatomic and histologic features of diaphragma sellae that effects the suprasellar extension. J Clin Neurosci 71: 234-244.
- Ismail M, Zidan W, Hamead K, Abdelhak B, Darwish M (2021) Endoscopic transsellar transdiaphragmatic approach for extensive suprasellar pituitary macroadenomas. Am J Otolaryngol 42(1): 102808.
- Fallah N, Taghvaei M, Sadaghiani S, Sadrhosseini SM, Esfahanian F, et al. (2019) Surgical Outcome of Endoscopic Endonasal Surgery of Large and Giant Pituitary Adenomas: An Institutional Experience from the Middle East. World Neurosurg 132: e802-e811.
- Elshazly K, Kshettry VR, Farrell CJ, Nyquist G, Rosen M, et al. (2018) Clinical Outcomes After Endoscopic Endonasal Resection of Giant Pituitary Adenomas. World Neurosurg 114: e447-e456.
- Snyderman C, Kassam A, Carrau R, Mintz A (2007) Endoscopic Reconstruction of Cranial Base Defects following Endonasal Skull Base Surgery. Skull Base 17(1): 73-78.
- Cavallo LM, Messina A, Cappabianca P, Esposito F, de Divitiis E, et al. (2005) Endoscopic endonasal surgery of the midline skull base: anatomical study and clinical considerations. Neurosurg Focus 19(1): E2.






























