Symptomatic Craniovertebral Junction Meningioma
Jonathan Wong Kee Chi*and Arshad Ali
Department of Neurosurgery, Sibu Hospital, Malaysia
Submission: April 27, 2021; Published: May 11, 2021
*Corresponding author: Jonathan Wong Kee Chi, Sibu Hospital, Sarawak,, No.2, Blok B, Floor 10, Skyvilla Condominium, Batu Kawah New Township, Malaysia
How to cite this article: Jonathan W K C, Arshad A. Symptomatic Craniovertebral Junction Meningioma. Open Access J Neurol Neurosurg 2021; 15(2): 555909. DOI: 10.19080/OAJNN.2021.15.555909.
Abstract
Meningiomas are tumors originating from the meninges of the brain and spine that are typically benign. Craniocervical Junction (CCJ) meningiomas account for 1.8–3.2% of all the meningiomas [1]. They may cause specific symptoms depending on the neoplasm size and location. Due to its complexity of the anatomy of this area, which includes the brain stem, vertebral artery, and lower cranial nerves, complete resection of CVJ meningioma often makes them a surgical challenge. Preservation and recovery of neurological function is the primary goal of treating CVJ meningiomas through surgical resection.
Method
We present a case of CVJ meningioma diagnosed with magnetic resonance imaging. A 44 years age lady with CVJ meningioma was operated at the Department of Neurosurgery, Sibu hospital, Sarawak, Malaysia.
Case Report
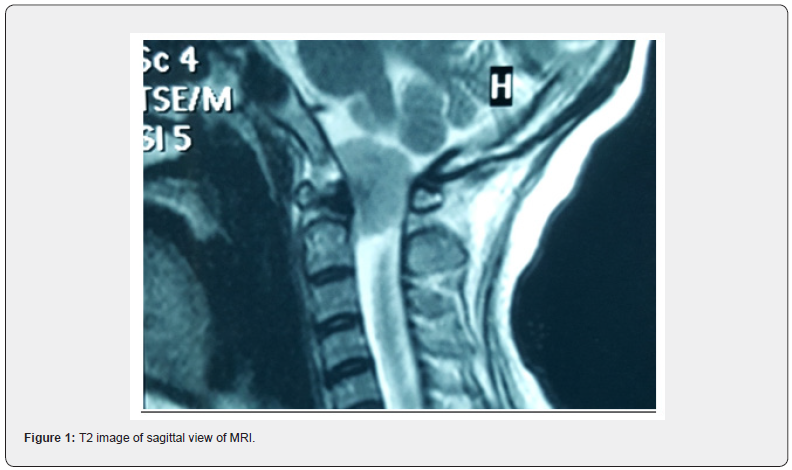
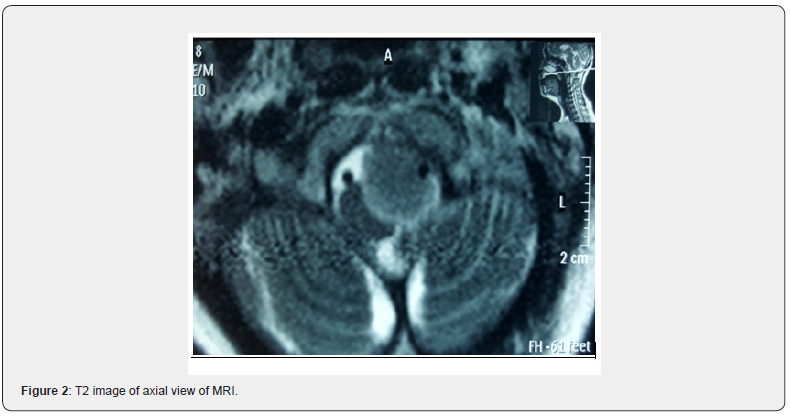
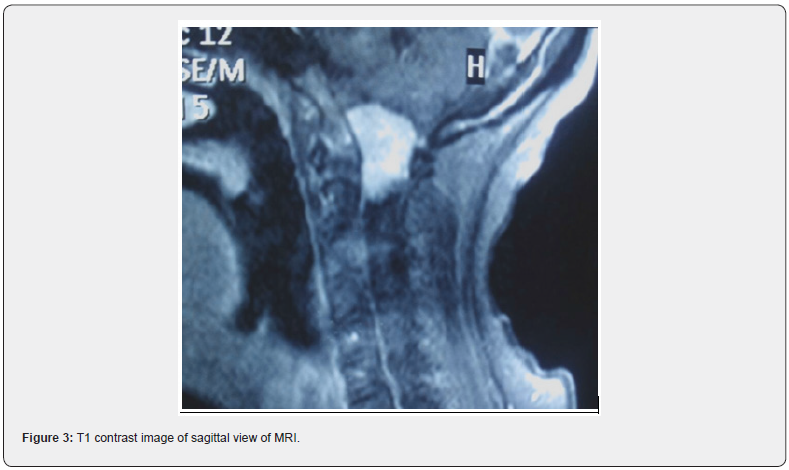
A 44 years old, female, Iban with underlying hypertension and dyslipidemia was referred our setting with initial presentation of neck pain for 3 months, not relieved by analgesia with progressive weakness of upper and lower limbs associated with acute urinary retention for 1 day. The sequelae of the limb weakness started over the left upper limb, followed by right upper limb with numbness, preceded with inability to shrug her bilateral shoulder with the involvement of right lower limb, followed by left lower limb after 3 months. CT Brain showed no obvious pathology. Subsequently, MRI whole spine was done showing intradural, extramedullary mass at cervicomedullary junction, which is isotense on T1, iso to hypotense on T2/FLAIR, measuring 1.6cm x 1.8cm x 2.4cm with the impression of cervico-medullary junction meningioma with medulla and spinal cord compression. On examination, head held in slight flexion with muscle wasting noted more over upper limb than lower limb. There was increased in muscle tone with babinski reflex up going and anal tone was lax. Sensation otherwise, was intact. Power of bilateral upper limb 3/5 with bilateral lower limb 4/5. Cranial nerve IX and XI were affected. Deep tendon reflexes are 3+ in all four limbs. She was started on IV Dexamethasone 6mg QID. She underwent left far lateral approach craniotomy and left C1 partial laminectomy with lumbar drain insertion. Histopathology showed Angiomatous Meningioma, WHO Grade I (Figures 1-4).
Discussion
Case 1
Around 66-73% of craniovertebral junction meningiomas are represented by females [1]. Different surgical approaches have been suggested for craniovertebral junction meningiomas, depending on the anatomical location of the tumor relative to the brainstem. Tumors situated anteriorly may be accessed with the far-lateral approach according to Heros [2], which was done on our patient, or the extreme lateral modification as described by George et al. [3]. Far lateral approach is a modification of the traditional lateral suboccipital approach that provides adequate exposure of the ventral craniocervical junction. In order to accomplish a complete, but safe resection of meningiomas situated in the ventral foramen magnum, techniques involving partial removal of the occipital condyle in combination with transposition of the vertebral artery, have been established which theoretically provides a more direct approach to the anterior clivus and anterolateral lesions by increasing the visibility from a standard posterolateral retrocondylar craniectomy by 15.9°. According to Nanda et al, it is necessary to drill occipital condyle to treat anteriorly located lesions without sufficient lateral extension, as well as large meningiomas associated with bone invasion or VA encasement [4]. Nevertheless, resection of occipital condyle was not performed on our patient. Post operatively, there was no complication encountered throughout the recovery period of our patient. One of the most frequent complications of surgery on foramen magnum meningiomas are lower cranial nerve palsies and other post-operative complications include meningitis, hydrocephalus, occipital-cervical instability and CSF leak. Thus, resection of the occipital condyle should be tailored to individual cases and should not be considered a mandatory technical step.

Conclusion
Although craniovertebral junction meningioma are typically pathologically benign, their locations, and the approaches used to access them, pose significant risks to the patient. So, meticulous pre-operative planning and suitable surgical technique must be employed to achieve the best surgical outcome for the patient
References
- Heros RC (1986) Lateral suboccipital approach for vertebral and vertebrobasilar artery lesions. J Neurosurg 64(4): 559-562.
- George B, Dematons C, Cophignon J (1988) Lateral approach to the anterior portion of the foramen magnum. Application to surgical removal of 14 benign tumors: technical note. Surg Neurol 29(6): 484-490.
- Kassam A, Carrau RL, Snyderman CH, Gardner P, Mintz A (2005) Evolution of reconstructive techniques following endoscopic expanded endonasal approaches. Neurosurg Focus 19(1): E8.
- Nanda A, Vincent DA, Vannemreddy PS, Baskaya MK, Chanda A (2002) Far-lateral approach to intradural lesions of the foramen magnum without resection of the occipital condyle. J Neurosurg 96(2) :302–309.






























