Normobaric Oxygen Therapy for Pneumocephalus; Simple, Cheap, Available and Effective
Sigurd Fosmark1, Helene Engstrand Lier1,2, Karoline Skogen3, Eirik Helseth1,4, Mads Aarhus1 and Jon Ramm-Pettersen1
1Department of Neurosurgery, Oslo University Hospital, Norway
2Department of Neurology, Oslo University Hospital, Norway
3Department of Neuroradiology, Oslo University Hospital, Norway
4Institute of Clinical Medicine, Faculty of Medicine, University of Oslo, Norway
Submission: October 13, 2020; Published: May 03, 2021
*Corresponding author: Sigurd Fosmark, Department of Neurosurgery, Oslo University Hospital, Kirkeveien 166, 0450 Oslo, Norway
How to cite this article: Fosmark S, Lier H, Skogen K, Helseth E, Aarhus M, et al. Normobaric Oxygen Therapy for Pneumocephalus; Simple, Cheap, Available and Effective. Open Access J Neurol Neurosurg 2021; 15(2): 555908. DOI: 10.19080/OAJNN.2021.15.555908.
Abstract
Background: Pneumocephalus is quite often seen after traumatic brain injury and neurosurgical procedures. Though the majority of patients are asymptomatic, lethargy, headache, dizziness, decreased level of consciousness and neurological symptoms may all be signs of the condition. A suggested treatment is supplemental normobaric oxygen, a simple, cheap, available and effective treatment. As a reminder of this often forgotten treatment, we here present four cases with pneumocephalus treated with normobaric oxygen supplement. A short review of the theoretical basis for this treatment modality is also presented.
Methods: In this retrospective case series, we present four cases of pneumocephalus, all treated with normobaric oxygen supplement. Serial imaging using CT was applied for evaluation, and air volumes pre- and post-treatment were calculated.
Results: All cases showed decreased volumes of intracranial air after receiving supplemental 100% O2 for 18-71 hours with a volume reduction of the intracranial air ranging from 51.5%-98.2%. In the three awake patients, radiographical volume reduction of the pneumocephalus was paralleled by clinical improvement. In one case the patient was on a ventilator during the normobaric oxygen treatment and clinical evaluation was not possible.
Conclusions: Our findings support the treatment of pneumocephalus with supplemental oxygen therapy
Keywords: Pneumocephalus; Normobaric; Oxygen; Intracranial
Introduction
Pneumocephalus is commonly seen after intracranial procedures and traumatic brain injury. The vast majority of patients are asymptomatic; however, some experience headaches, lethargy, and focal neurological symptoms. In severe cases this condition can be life threatening. In the latter gas tends to accumulate bifrontally appearing as the classical Mount Fuji sign on head CT (computed tomography). This is indicative of a tension pneumocephalus, which may warrant immediate management [1]. Management options include surgical evacuation of air, hyperbaric oxygen treatment and normobaric oxygen therapy. Due to the urgency, the trend is often invasive and resource demanding procedures; while the simple, cheap, and readily available normobaric oxygen treatment is often forgotten. The evidence of its efficacy is scarce rendering it controversial. This treatment is examined through four patients from our institution with different underlying conditions for their substantial pneumocephalus. They all received supplemental normobaric oxygen treatment. In this case series, together with a review of the literature, we want to remind the clinicians of this simple, cheap, available and effective treatment.
Methods
Four cases of pneumocephalus treated at the Neurosurgical department at Oslo University Hospitals were included. They had different underlying conditions and three of them were secondary to neurosurgery. The initial volume (Vpre) of the pneumocephalus was measured on the head CT using Brainlab Elements/iPlan v. 3.0 (Brainlab AG, Olof-Palme-Str. 9, 81829 Munich, Germany) prior to normobaric oxygen treatment. The duration of the normobaric supplemental O2 differed between the patients. A pneumocephalus volume (Vpost) was measured on the control CT performed after normobaric oxygen treatment. From these values the difference in volumes for each patient (ΔV), and the rate of absorption (ΔV/T) defined as change in volume per hour, as well as the rate in per cent per hour (%r/T) was calculated.
Case reports
Case 1
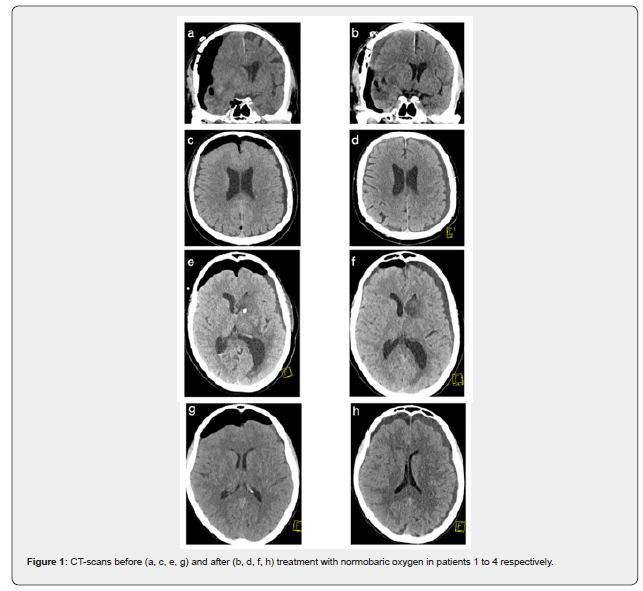
A 69-year-old man with hypertension, previous NSTEMI and atypical Parkinsonism was admitted with a Glasgow Coma Score (GCS) of 13 and left-sided hemiplegia to his local hospital. Head CT and MRI showed a primary brain tumour with haemorrhage. He was transferred to the neurosurgical department and a craniotomy was performed with complete resection of the tumour. The postoperative head CT showed a right-sided pneumocephalus with mass effect and midline shift with a volume of 120.6 mL (Figure 1a). Post operatively he also developed a pneumonia and his level of consciousness varied from a GCS 7-11. The pneumocephalus was managed with 25L/min 100% O2 supplement on a mask with reservoir for 18 h. His pO2 reached a peak level of 19kPa. A control CT (Figure 1b) showed a reduction of the pneumocephalus volume to 58.4 mL and a decrease in the mass effect. This gives an absorption rate of 3.46 mL/h, or 2.86%/h. He was transferred back to the local hospital where he made a gradual partial recovery.
Case 2
A 75-year-old man with angina pectoris on acetylsalisylic acid fell and hit the back of his head on the ice 3 days prior to admission. He remained fully conscious after the fall, and he drove home himself after the incident. In the following days, he experienced an increasing headache and a dot feeling in his left ear together with reduced hearing. Repetitive Valsalva’s maneuvers were performed to equalize the presumed increased pressure in the left ear. This resulted in a bubbling sensation in his head. The preceding day he went to his General Practitioner (GP) as the symptoms persisted in his left ear. The GP admitted him to the local hospital for further evaluation. A head CT revealed a fracture in the left temporal bone affecting the mastoid bone and consequently blood in the left middle ear. There was a 4 mm chronic subdural hematoma, frontal pneumocephalus of 61.4 mL (Table 1) with a tendency of a Mount Fuji sign, but no signs of herniation (Figure 1c). His acetylsalisylic acid was paused and he was transferred to the neurosurgical department. On arrival he was nauseous and on examination had a small cut in the back of his head, decreased hearing on his left ear and moderate leftsided hemotympanum. Further neurological examination was normal. The pneumocephalus was treated with 10L/min 100% O2 on a mask with reservoir. A control head CT after 12 hours of treatment showed some regression of the pneumocephalus, and he had improved clinically. He was treated for a total of 71 hours with O2. The pO2 was not measured during his treatment. On the final control CT there was a significant decrease in the pneumocephalus (Figure 1d) with a remaining pneumocephalus of 1.1 mL, thus the absorption rate was 0.85 mL/h, or 1.38%/h (Table 1). The presenting symptoms, exempting his left-sided hearing loss, regressed and he was discharged

Case 3
This 63-year-old female patient with a history of fibromyalgia, depression and hypertension, treated with antihypertensive medicine was admitted to her local hospital after she collapsed in her own home. On site her GCS was 5 and she had a blown right pupil, hence she was intubated prehospitally. A head CT showed a left sided intracerebral haemorrhage with perforation into both lateral ventricles, third and fourth ventricles as well as the basal cisterns. An intracerebral CT angiogram did not reveal any vascular malformations. She was immediately transferred to the neurosurgical department for an evacuation of the haemorrhage with a left sided craniotomy and placement of an External Ventricular Drain (EVD). Postoperatively she remained intubated and the post operative head CT the next day showed a pneumocephalus of 62 mL with the Mount Fuji-sign (Figure 1e). The pneumocephalus was managed with 100% O2 on a ventilator for approximately 22 hours. Her pO2 was raised to 52kPa during this time. The control head CT (Figure 1f) at this time revealed a considerable reduction of the pneumocephalus to 9.3 mL giving an absorption rate of 2.40 mL/h, or 3.86%/h in relative terms. A new head CT four days later showed almost complete regression of the pneumocephalus. She was discharged to rehabilitation with neurological deficits consisting of a right-sided hemiparesis and dysphasia.
Case 4
An 82-year-old woman with hypertension, osteoporosis and psoriasis on acetylsalisylic acid suffered from headaches and unsteadiness for 3 months. A head CT revealed bilateral Chronic Subdural Hematomas (CSDH) with compression of the lateral ventricles and decreased surface relief. Acetylsalisylic acid was paused for one week and the CSDH were evacuated with bilateral single burr holes. There were no perioperative complications. Postoperatively her GCS score fell to 11. The head CT showed a bifrontal pneumocephalus of 128.0 mL with mass effect (Figure 1g). No action was taken at this time. The consecutive day she developed an intermittent total AV-block with a 10 second pause which was treated with a pacemaker. Her GCS then fell to 5 after this and the pneumocephalus was aspirated through the subdural drains with an immediate effect, and her GCS increased to 13, however her level of consciousness varied. There was still a large pneumocephalus on a control head CT. She was further managed with intermittent Opti flow and then 10 L/min 100% O2 on a mask for 28h giving her a max pO2 of 58kPa. The final control head CT (Figure 1h) showed a considerable reduction of the pneumocephalus to 34.5 mL along with good clinical progress. This gives an absorption rate of 3.34 mL/h or 2.61%/h. On return to her local hospital she had a GCS of 15 and a slight headache.
Discussion
In this case series we present four patients with differing aetiologies for pneumocephalus, all treated with normobaric oxygen therapy. All four cases had imaging improvement with decreased amount of intracranial air, ranging from 51.5-98% volume reduction (Table 1). The absorption rate varied from 1.38- 3.86%/h. These results are similar to ones obtained by Gore et al who reported a mean absorption rate of 2.7%/h (1.7-3.7%/h) in a small prospective case-control study with normobaric oxygen for non-tension pneumocephalus [2]. Pneumocephalus may be caused by trauma, infection or intracranial surgery. In most cases no action is needed, however in rare cases patients may experience a variety of neurological symptoms, commonly lethargy, headache, nausea and altered mental status and if severe it can be a life threatening condition. Intracranial air can accumulate in any space within the cranial vault, but most commonly it occupies the subdural space [3] and generally accumulates bi-frontally, causing the classic and characteristic Mount Fuji sign on a head CT [1, 4]. This may be caused by either tension or non-tension pneumocephalus. Tension pneumocephalus may arise when a valve like fistula between the extracranial and intracranial space allows air to move in but not out of intracranial space. Air will then be trapped within the cranial vault. It may also appear after cranial surgery in the rare cases of N2O anaesthesia which increases the intravascular partial pressure of nitrogen [5, 6]. As this is a neurosurgical emergency, immediate surgical intervention is often warranted. However, in the case of non-tension pneumocephalus it is easy to forget the simple, cheap, available and effective supplemental normobaric O2 which was given to all patients in our series.
The pneumocephalus is made up of atmospheric air which constitutes mainly of oxygen and nitrogen, with the latter posing the largest part of the two gases, 21% vs 79% respectively. Removing nitrogen would decrease the volume to a larger extent than removing any other gas component. Increasing the partial pressure of oxygen within the cerebral arterial blood creates a concentration gradient of nitrogen to cross over the endothelium of cerebral vessels, as oxygen suppresses nitrogen within the blood. Hence the nitrogen diffuses into the blood and is transported to the lungs where it is exhaled [7]. This was described by Dexter and Reasoner who found that an increase in the fraction of inspired oxygen (FiO2) from 0.21 (atmospheric oxygen pressure at sea level) to 0.4 increased the absorption velocity of nitrogen with 67%. Further increase in FiO2 gave only minor increase in nitrogen absorption. Based on mathematical models they found the optimal (FiO2) to be 0.4, reaching close to plateau absorption velocity with minimal risk [7]. Our patients all received 100% O2, hence we did not look further into this matter. The pO2 was measured in three patients, but not in case 3. The maximum values differed from 19kPa to 58kPa. This direct measure of the arterial partial pressure of oxygen is, unlike FiO2, independent of lung function. Finding an optimal value of pO2 for patients with pneumocephalus may be helpful to guide treatment. It was further described that the absorption rate decreased with decreasing size of the pneumocephalus, making the time-absorption relationship non-linear [7]. This can explain the common practice of an initial 24h management and then re-evaluation after a control head CT. The patients presented here had a varying absorption rate which may be explained by different delivery methods. In case 3 the patient received oxygen while on a ventilator, which may have played a role in the high absorption rate of 3.86%/h. In case 2 the patient was treated for 71 hours, and there was no radiographic control between 12 and 71 hours of treatment since the patient was improving. Thus, there is not any assessment of the pneumocephalus between these times. Considering the nonlinear absorption rate described earlier [7], there is a chance the pneumocephalus may have been close to reabsorbed in the time between the two control head CTs. We present four cases of pneumocephalus of which three are after cranial surgery and one has a rather special traumatic mechanism. Based on our experience large pneumocephalus is rarely seen after trauma, but in this case the patient forced air through a dural defect by repeatedly performing Valsalva’s maneuver.
The modes of increasing the partial pressure of oxygen within the cerebral arteries are typically normobaric as in this case series, either by nasal catheter or a mask. Some argue that in severe cases hyperbaric oxygenation should be considered [8,9], as this increases the absorption velocity, while others have suggested efficient treatment with high-flow O2 through a nasal cannula [6]. Exempting case 3 in our series, where the patient was treated while unconscious and intubated, the remaining cases all had symptoms that could be prescribed to the pneumocephalus, and all seemingly had good clinical effect of the treatment. This supports the somewhat controversial current therapy with oxygen for pneumocephalus. The treatment is cheap, simple, readily available and may even be applied in hospitals without a neurosurgeon. The duration of treatment remains controversial, reflected in our cases where the treatment duration varied from 18-71 hours. Pneumocephalus is a well-known condition in the neurosurgical department, it seems reasonable that its treatment should be thoroughly investigated and well-founded. As mentioned, the delivery method and aggressiveness of oxygen therapy also varies, ranging from normobaric oxygen through nasal catheter to the more extreme hyperbaric oxygenation, and herein lies another potential for further investigation.
Limitations
The cases presented here were treated with normobaric oxygen therapy, but with different delivery methods, a mask, with or without reservoir, or a ventilator. This might have influenced the absorption velocities. The treatment duration differed between cases, and the optimal duration was not further investigated. Age, background and medical history, such as lung function, varied between patients. There were no controls in our series and thus resolution of pneumocephalus without supplemental O2 may not be excluded, and the absorption rate in such cases were not assessed. Hence a randomized controlled trial should be performed to assess these points.
Conclusion
The four cases presented in this article support the use of supplemental normobaric O2 for the treatment of pneumocephalus, a simple and effective treatment that should be part of the neurosurgical armamentarium.
Consent
The patients or their closest relatives have given their informed consent for the publishing of case reports.
References
- Heros RC (1986) Lateral suboccipital approach for vertebral and vertebrobasilar artery lesions. J Neurosurg 64(4): 559-562.
- George B, Dematons C, Cophignon J (1988) Lateral approach to the anterior portion of the foramen magnum. Application to surgical removal of 14 benign tumors: technical note. Surg Neurol 29(6): 484-490.
- Kassam A, Carrau RL, Snyderman CH, Gardner P, Mintz A (2005) Evolution of reconstructive techniques following endoscopic expanded endonasal approaches. Neurosurg Focus 19(1): E8.
- Nanda A, Vincent DA, Vannemreddy PS, Baskaya MK, Chanda A (2002) Far-lateral approach to intradural lesions of the foramen magnum without resection of the occipital condyle. J Neurosurg 96(2) :302–309.






























