Duplication of the superior sagittal sinus: Potential for misinterpretation as venous sinus thrombosis
Beesan Warasna*
Faculty of Medicine, AlQuds University, Palestine
Submission: March 13, 2021; Published: April 14, 2021
*Corresponding author: Beesan Warasna, Faculty of Medicine, AlQuds University, Jerusalem, Palestine
How to cite this article: Beesan W, Zanna V, Shahram D. Duplication of the superior sagittal sinus: Potential for misinterpretation as venous sinus thrombosis. Open Access J Neurol Neurosurg 2021; 15(1): 555903. DOI: 10.19080/OAJNN.2021.15.555903.
Keywords: Cerebral Venous Sinuses, Stroke, Cerebral Circulatory Variations
Mini Review
An 83-year-old man presented with a gradual onset generalised headache and left facial focal motor seizure, progressing to a generalised tonic clonic seizure. This occurred in the context of previous left hemispheric infarct, hypertension, chronic obstructive pulmonary disease, and a recent calf deep vein thrombosis for which he had completed a course of anticoagulation. Brain CT showed no evidence of acute infarct or other major focal structural deficit. Due to this absence of apparent focal trigger, together with the presence of headache and recent thrombosis, he underwent a brain MRI with MR venogram as part of investigation for his new onset seizure syndrome. This was initially suspected to show a sagittal venous sinus thrombosis, but on re-review this defect was felt to represent a congenital duplicated sagittal sinus.
Anatomical variation of the dural sinuses is common. This is particularly evident at the torcula: the number of variations seen in connections between the superior sagittal sinus, straight sinus and two transverse sinuses is so numerous, in fact, as to preclude classification [1]. This variability owes to the torcula’s late embryologic formation from the primordial venous plexus, which occurs substantially later than that of anterior and middle sinuses.
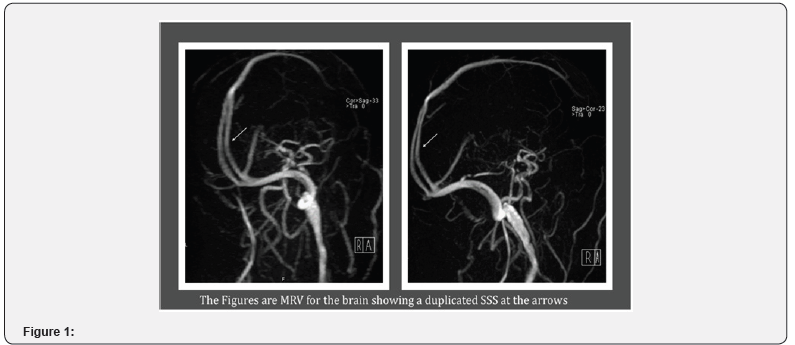
Among this heterogeneity, bifurcation of the superior sagittal sinus is a recognised variant. Previous attempts to estimate its prevalence have varied between 4% [2,3], 14% and 23.5% of individuals studied, and bifurcation has been observed to occur as early as 53mm proximal to the torcula [4]. This has previously been noted to bear potential for misinterpretation as venous sinus thrombosis, for example through artefactual creation of the ‘delta sign’ considered pathognomonic of sinus thrombosis [1]. To our knowledge, however, this is the first reported case in which each fork of the bifurcated superior sagittal sinus drains into one transverse sinus; a variant rendering the imaging particularly liable to misinterpretation as sagittal venous sinus thrombosis by creating the illusion of a flow void. This case therefore emphasises the importance of an appreciation of dural venous sinus anatomical variability, to prevent misdiagnosis of cerebral venous sinus thrombosis.
References
- Zouaoui A, Hidden G (1988) Cerebral Venous Sinuses: Anatomical Variants or Thrombosis? Acta Anat (Basel) 133(4): 318-324.
- Widjaja E, Griffiths PD (2004) Intracranial MR venography in children: normal anatomy and variations. AJNR Am J Neuroradiol 25(9): 1557-1562.
- Bisaria K (1985) Anatomic variations of venous sinuses in the region of the torcular Herophili. J Neurosurg 62(1): 90-95.
- Surendrababu NR, Subathira, Livingstone RS (2006) Variations in the cerebral venous anatomy and pitfalls in the diagnosis of cerebral venous sinus thrombosis: low field MR experience. Indian J Med Sci 60(4):135-142.






























