Diagnostic Value of Long-Term Video-EEG Monitoring in Children with Refractory Absence Epilepsy
Mahmoud Mohammadi1, Alireza Rezayi2,3*, Mahmoudreza Ashrafi1, Gholmamreza Zamani1, Reza Shervin Badv1, Bahram Yarali1, Alireza Tavasoli1, Morteza Heydari1 and Fatemeh Khodaei4
1Department of Pediatric Neurology, Epilepsy Monitoring Unit (EMU), Pediatrics Center of Excellence, Children’s Medical Center, Tehran University of Medical Sciences, Iran
2Skull Base Research Center, Loghman Hakim Hospital, Shahid Beheshti University of Medical Sciences, Iran
3Pediatric Neurology Research Center, Mofid Children Hospital, Shahid Beheshti University of Medical Sciences, Iran
4Master of Midwifery, Skull Base Research Center, Loghman Hakim Hospital, Shahid Beheshti University of Medical Sciences, Iran
Submission: February 08, 2021;Published: March 10, 2021
*Corresponding author: Alireza Rezayi, Department of Pediatric Neurology, Epilepsy Monitoring Unit (EMU), Pediatrics Center of Excellence, Children’s Medical Center, Tehran University of Medical Sciences, Iran Loghman hakim hospital, kamali St, South Karghar, Tehran, Iran
How to cite this article: Mahmoud M, Alireza R, Mahmoudreza A, Gholmamreza Z, Reza Shervin B, et al. Diagnostic Value of Long-Term Video-EEG 0096 Monitoring in Children with Refractory Absence Epilepsy. Open Access J Neurol Neurosurg 2021; 14(5): 555900 DOI: 10.19080/OAJNN.2021.14.555900.
Abstract
Objective: Absence seizures are commonly seen in a few pediatric genetic generalized epilepsy syndromes including childhood and juvenile absence epilepsies (CAE, JAE), absence with eyelid myoclonias (EMA–EM or Jeavons syndrome), atypical absence seizures as a component of Lenox-Gastaut Syndrome (LGS). Here, we report the clinical and electroencephalographic features of patients with refractory absence epilepsy.
Methods: Twenty-five children referred with refractory absence epilepsy were retrospectively enrolled from more than 1100. We have used tow digital VEEG instruments with the international 10-20 system and standard montages. Patients and their Clinical history and VEEG recordings were studied to find data including age, sex, seizure types, electrographic features, and family history of epilepsy.
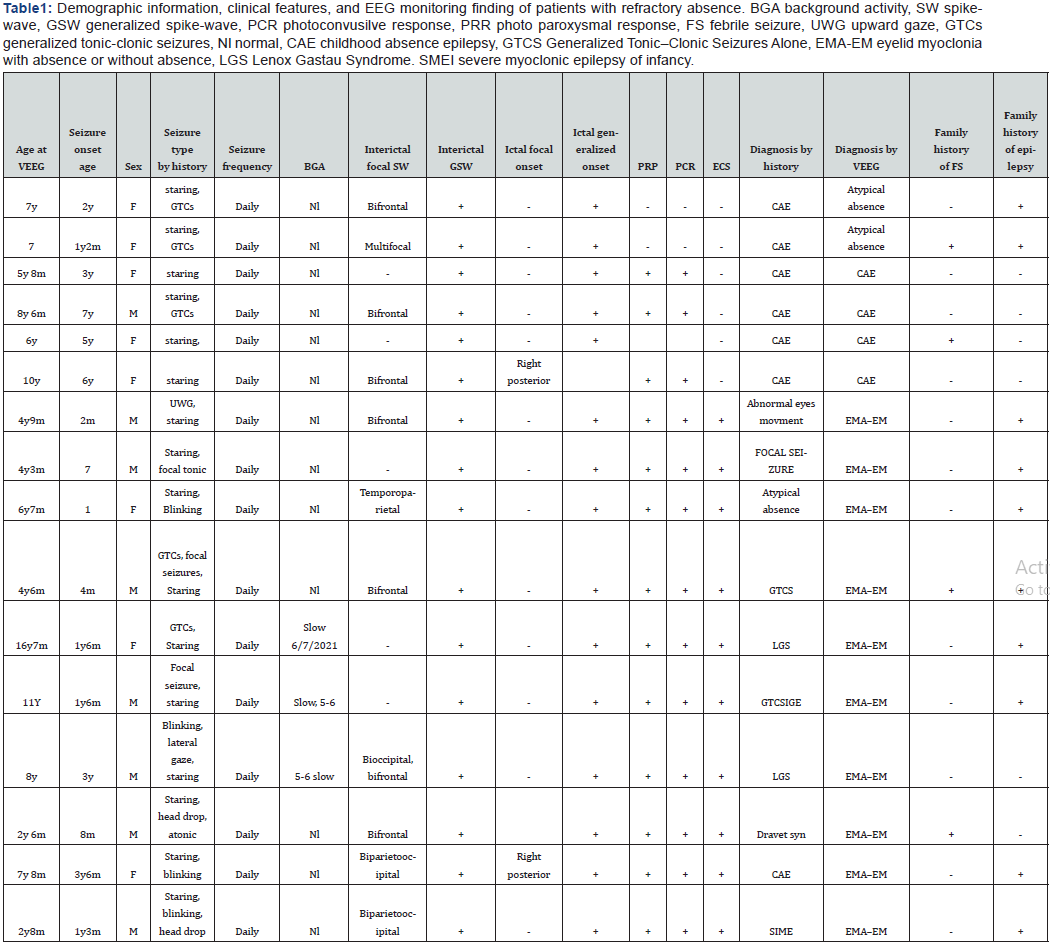
Results: According to exclusion criteria we had 16 patients that 4 of them had CAE and 2 of them had atypical absence epilepsy (AAE) and 10 had EMA–EM. Focal interictal SWD (spike-wave discharges) was seen in both atypical absence patients (100%), 2 from 4(50%) patients of CAE, and 7 of 10(70%) patients EMA–EM. Focal ictal onset was seen in 1 of 4 (25%) of CAE patients and one of 10(10%) of EMA-EM patients. All EMA–EM and atypical absence patients were diagnosed after long-term EEG-monitoring (LTM)and they had other diagnoses before LTM.
Significance: EMA–EM should be considered in refractory childhood absence epilepsy and video-EEG recording is a useful method if EMA-EM is suspected. Focal interictal and ictal onset might be recorded in generalized epilepsy especially in CAE which the importance of this issue should be considered in future investigations.
Keywords: Absence epilepsy; Jeavons syndrome; Atypical absence; Focal seizure onset; Focal interictal epileptic discharge; LTM; EEG monitoring; V-EEG
Introduction
Absence seizures, are characterized by frequent sudden discontinuation of activities, brief staring episodes, with loss of awareness and abrupt recovery are commonly seen in a few pediatric generalized epilepsy syndromes including childhood and juvenile absence epilepsies (CAE, JAE), and juvenile myoclonic epilepsy (JME), absence with eyelid myoclonias (EMA–EM or Jeavons syndrome), epilepsy with myoclonic-atonic seizures (Doose Syndrome) and Lenox-Gastaut Syndrome (LGS). The EEG feature in CAE and JAE patients usually demonstrates generalized Spike-Wave Discharges (SWD) averaging 3HZ frequency with the normal background. This type of absence seizure respond to specific antiepileptic drugs including ethosuximide and valproic acid, however some patients with absence seizures may having drug-resistant epilepsy by International League Against Epilepsy (ILAE) definition [1]. failure rate is about 53% and 58% for ethosuximide and valproic acid, after 16 weeks of therapy [2]. Atypical Absence Seizures (AAS) have slower SWD on EEG (1.5-2.5 HZ), Interictal Epileptic Discharges (IEDs) usually have multifocal epileptiform features. This type of seizure begins before 5 years of age and sometimes associated with diminished postural tone, tonic, or myoclonic activity. AAS often diagnosed as a component of LGS [3]. Eyelid myoclonia with or without absences (EMA-EM) is recognized as a seizure type by the International League Against Epilepsy (ILAE). Idiopathic EMA-EM (or JS) has been described as a long-lasting condition beginning in childhood and having a higher incidence in girls [4,5]. The EEG presentation of JS has been described as focal occipital or frontal predominant SWD in both interictal and ictal stages [6,7].
To diagnose this syndrome presence of the following triad is mandatory:
a. Eyelid myoclonia,
b. Photosensitivity
c. Eye-closure sensitivity, or fixation off sensitivity (EEG paroxysm or absence seizure within 0.5 to 4 second after eye closure). All subjects of EMA-EM are normal at disease onset and it is a life-long condition and can be difficult to treat and should be considered in the patients with drug-resistant absence epilepsy [3]. Brief 20–30 min standard EEG recording with or without video is not useful for differentiating patients with refractory absence epilepsy. Misdiagnosis of epilepsy subtypes can lead to inappropriate treatment, or no treatment, with considerable associated costs in health and economic terms [8,9]. Clinicians should consider long term EEG- monitoring to provide answers in such cases as well as ILAE recommendation [10].
The objective of this study is to review the clinical and EEG features of patients with drug-resistant absence epilepsy to observe epilepsy syndromes featuring absence seizures.
Methods
a. Twenty-five children referred with refractory absence epilepsy were retrospectively enrolled from more than 1100 VEEG recordings monitored in our hospital between August 2014 and August 2019. Inclusion criteria
b. Absence epilepsy, Childhood Absence Epilepsy (CAE), or Juvenile Absence Epilepsy (JAE) were identified by history.
c. Normal findings on neurological examination,
d. Normal epilepsy protocol magnetic resonance imaging (EPMRI),
e. Normal metabolic screening tests
f. Normal developmental status before seizure beginning 6) Normal CSF analysis including CSF glucose for GLUT1- deficiency.
Exclusion criteria
a. Subjects with focal epilepsy syndromes for instance frontal lobe epilepsy or temporal lobe epilepsy that referred to as refractory absence,
b. Subjects with LGS that they had atypical absence epilepsy. According to exclusion criteria we had had only 16 patients that 4 of them had CAE and 2 of them had Atypical Absence Epilepsy (AAE) and 10 had EMA–EM.
VEEG monitoring was performed by two Nihon Kohden digital video-EEG-1100 K instruments for approximately 24-72 hours, in both awake and asleep states. Electrodes were placed on the scalp according to the international 10-20 system, with standard montages including bipolar and referential montages with some extra leads and surface electromyography to record the activities of the deltoid muscle. At wakefulness, hyperventilation, open-close eyes test, and IPS were performed in all patients. all VEEG reviewed by authors for the following aspects: background activity, sleep architecture, normal variants, artifacts, PPR (photo paroxysmal response), PCR (Photo Convulsive Response), HV (hyperventilation) response, IED (Interictal Epileptic Discharge) during asleep and wakefulness and ictal electrographic features. Clinical history and VEEG recordings were studied to find data including age, sex, age at seizure onset, seizure types, electrographic features, and family history of epilepsy as well as treatments. Psychomotor development was evaluated clinically in all patients. This study was approved by the Ethical Committee of children’s medical center, and written informed agreements were attained from parents of the children. All investigations were performed with related guidelines. All data were analyzed by the de-identified manner.
Results
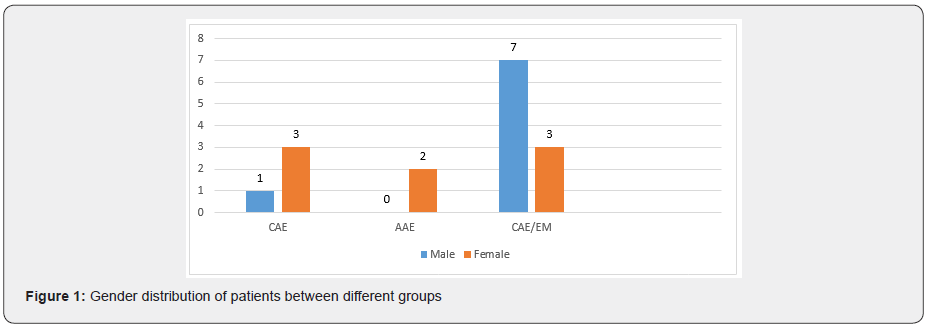
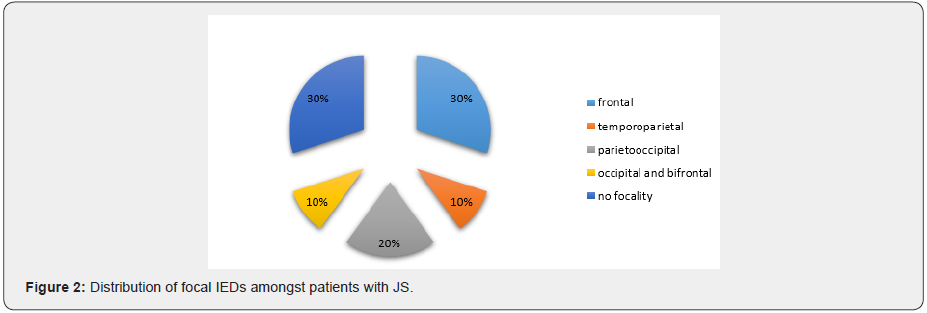
Out of 1100 patients that referred from epilepsy clinic of children medical center for long term video EEG monitoring (LTM) 25 patients had refractory staring spells but 16 patients met inclusion criteria. Then we analyzed the LTM of 16 patients. The mean age was 7yr (2m to 16y7m). The mean age of seizure onset was 2.5(2m to7). 8 patients were female and 8 were male. 4 patients had CAE, 2 had atypical absence and 10 of them had EMA–EM. There were male predominate among the EMA–EM patients and female predominates in the CAE and atypical absence group. Both atypical absences had the previous history of GTCs, but only two of 10 EMA–EM had pure staring and most of them had mixed type of seizures. Background activity was normal in the group of CAE and atypical absence patients but in 3 patients of EMA–EM was slow regarding the patient’s age. 10 patients (62.5%) had focal interictal SWD. Focal interictal SWD was seen in both atypical absence patients (100%), 2 from 4(50%) patients of CAE, and 7 of 10(70%) patients EMA–EM. The most common focal interictal was seen in the frontal region (80%) commonly in the EMA–EM and multifocality was seen in one of atypical absence patient. Ictal focal SWD onset was seen in 3(18.75%) which has happened in one patient (25%) of CAE and 2 (20%) patients of EMA–EM. PPR and PCR were seen in all patients of CAE and EMA– EM but it was not seen in atypical absence patients. AII EMA–EM and atypical absence patients were diagnosed after LTM and they had other diagnoses before LTM. CAE patients did not get any medication during the LTM but some patients in EMA–EM and atypical absence used their medication with minimum dosage due to the previous history of GTCs. The family history of epilepsy and febrile seizure was seen commonly in the EMA–EM patients. Fixation off sensitivity or eye closure sensitivity (ECS) is positive in all cases of EMA–EM patients.
Discussion
This study examines the diagnostic value of long-term EEGmonitoring in patients who do not respond to common treatment of absence epilepsy. The most common diagnosis between children with refractory absence epilepsy is EMA–EM (Jeavons syndrome). This is an important point because they had other diagnoses before LTM. The following reasons may be responsible for this issue. First, conventional standard EEG recording in our country is recorded by undertrained EEG technician who does not detect fixation off sensitivity(Figure 1&2), characterized by the absence seizure or EEG paroxysmal activity within 0.5 to 4 second after eye closure and we usually miss it in the conventional EEG recording but it could be recorded and determined by LTM. Secondly, standard EEG does not have synchronized video recording and as a consequence, minor staring or absence seizures after eye closure could be overlooked. We recommend, therefore, that standard EEG in tertiary centers should have the video recording and EEG technicians should be selected from well-trained technicians. Thirdly under-diagnosis of Jeavons syndrome is common in our country because this condition is very rare and child neurologists do not have enough information about it. This finding is compatible with the survey on Jeavons syndrome in china that conducted by [11]. The majority of Jeavons syndrome is male that is compatible with Chinese patients but not supported by other studies. It could be due to patients’ selection because our center is a referral center or could be due to different genetic characteristics between the western and eastern populations. Two types of IEDs are reported in Jeavons syndrome; those which are more frontal predominant and those which are occipital predominant. Our study shows a case with both of them and some cases with parieto-occipital or temporo-parietal predominant SWD during tracing but frontal predominant IEDs are most commonly seen just like previous studies [11]. Ictal spiky posterior alpha was reported in previous studies which were concordant with EEG findings of one of our cases [12]. JS is believed to have a genetic etiology, and, in our study, 90 percent of JS has a positive history of epilepsy or febrile seizure but in CAE patient only one patient had a family history of febrile seizure. It can be understood the genetic basis of CAE and JS is totally different. This point is mentioned in previous studies [13] (Figure 3&4).
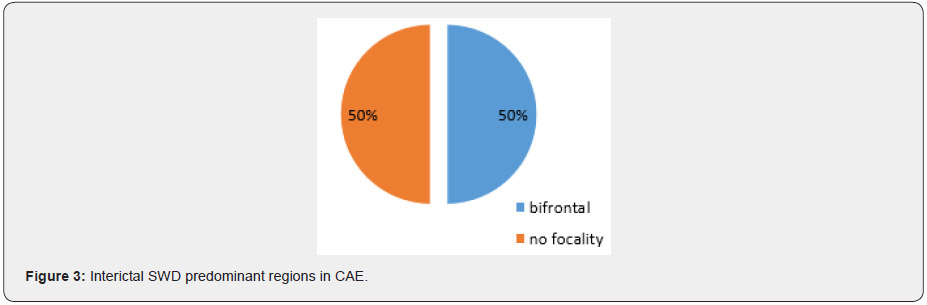
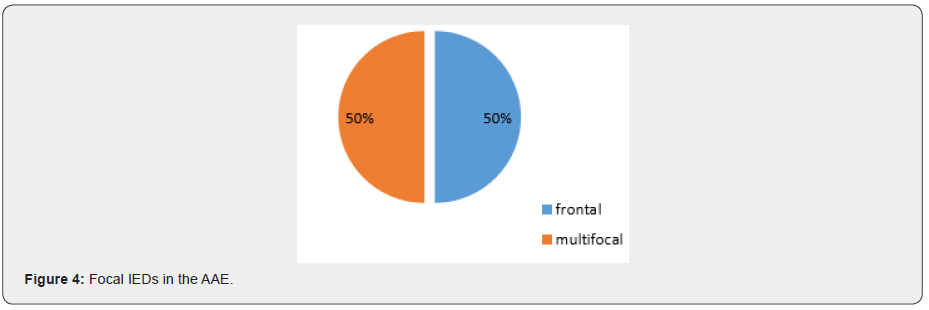
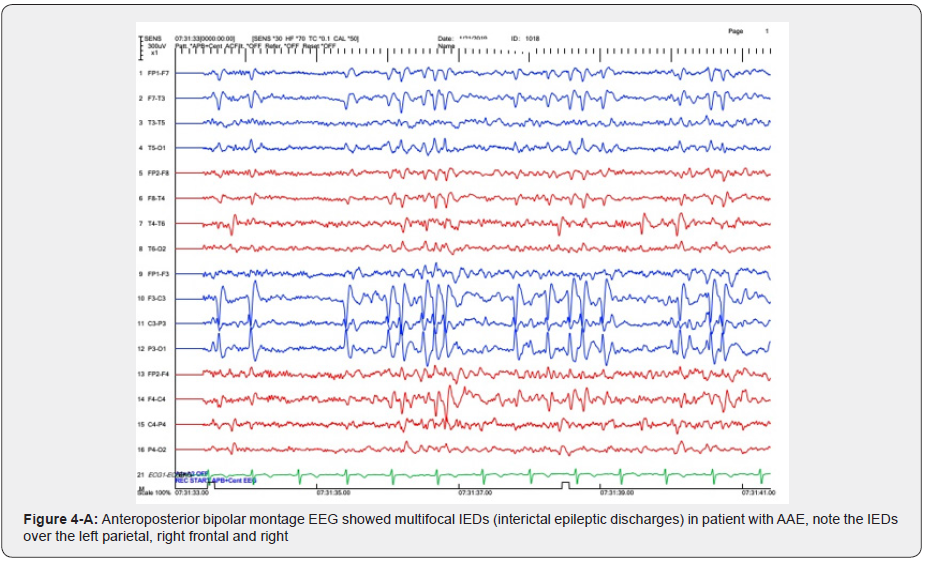
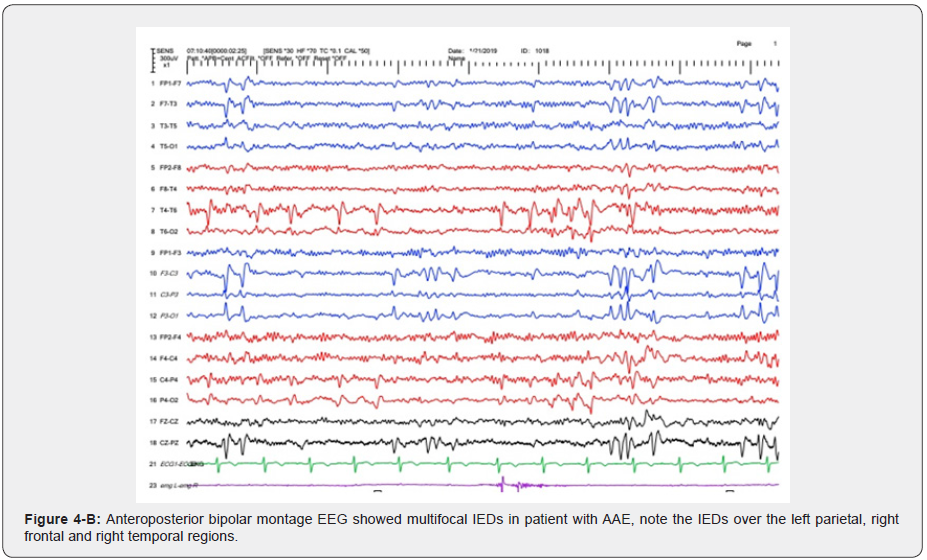
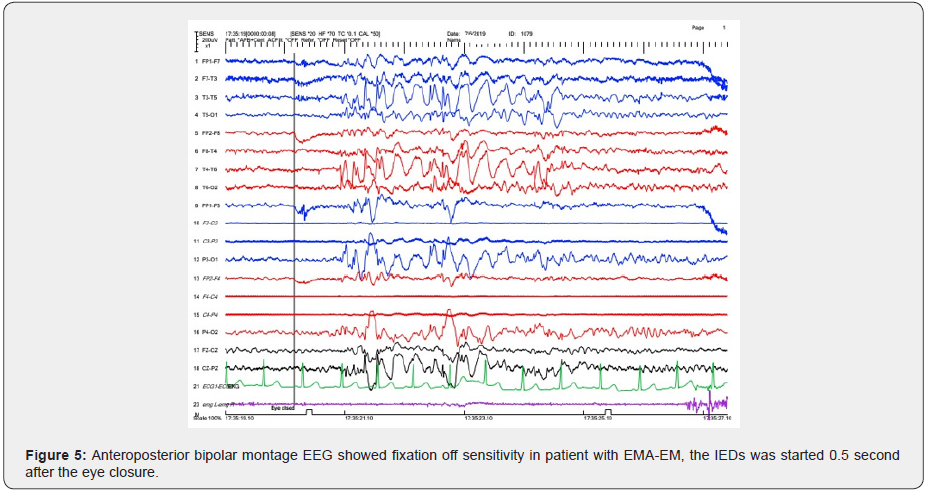
In the majority of JS background activity is normal for the patient’s age but in three (30%) is slower than normal for age. All of these patients had intellectual disabilities. This finding is similar to other studies [3] (Figure 4A, 4B). Focal interictal spikes in JAE patients is common (50%) and frontocentral predominant SWD also is common in the CAE patients (Focal and generalized SWD) [14]. one of the most interesting points in our study is a case of CAE with ictal focal onset from right posterior which according to our knowledge has not reported so. In this patient’s epilepsy protocol, MRI was normal and there was not any focal abnormality in the right posterior regions (Figure 5,6). This issue should be observed carefully in future investigations about CAE. Clinically, AAE is often a component of Lennox–Gastaut syndrome associated with mental retardation and behavioral problems, for instance, inattention hyperactivity, aggressiveness, and autistic features [3]. in the present study we detected two patients with clinical and electrographic findings close to AAE without any intellectual disabilities and also, they had normal development and behavior. These patients had normal Brain MRI but focal IEDs were seen which was bifrontal in one and multifocal in another one. Both of them had a positive family history of epilepsy. It could be due to distinct genetic susceptibility in AAE patients. This issue needs further investigations to report the AAE as a distinct epilepsy syndrome. In conclusion, JS or EMA–EM should be considered in refractory childhood absence epilepsy and video-EEG recording is a useful method if EMA-EM is suspected. Focal ictal onset could be recorded in generalized epilepsies which should be considered in future investigations. Pure Atypical Absence Epilepsy (AAE) without LGS could be added as a distinct epilepsy syndrome in the future.
Acknowledgment
We hereby thank participating parents, children, officials, and personnel of the Epilepsy Monitoring Unit (EMU) and Miss Bakhshi head nurse of EMU who provides all documentation for this study.
The study was supported by Children Medical Center affiliated by Tehran University of Medical Sciences.
References
- Bouma PA, Westendorp RG, van Dijk JG, Peters AC, Brouwer OF (1996) The outcome of absence epilepsy: a meta-analysis. Neurology 47(3): 802-808.
- Glauser TA, Cnaan A, Shinnar S, Hirtz DG, Dlugos D, et al. (2010) Ethosuximid valproic acid, and lamotrigine in childhood absence epilepsy. New England Journal of Medicine 362(9): 790-799.
- Pellock, John M, Douglas R Nordli, Raman Sankar, James Wheless (2016) Pellock's Pediatric Epilepsy Diagnosis and Therapy. 309-335.
- Panayiotopoulos CP (2005) Reflex seizures and reflex epilepsies. In: Panayiotopoulos CP, Eds. The epilepsies: seizures, syndromes and management. Oxford: Bladon Medical Publishing pp. 449-96.
- Pérez-Errazquin F, Chamorro-Muñoz MI, García-Martín G, Romero-Acebal M (2010) Does Jeavons syndrome exist? A report of a series of 10 cases. Rev Neurol 2010;50(10): 584-590.
- Striano S, Capovilla G, Sofia V, Romeo A, Rubboli G, et al. (2009) Eyelid myoclonia with absences (Jeavons syndrome): a well-defined idiopathic generalized epilepsy syndrome or a spectrum of photosensitive conditions. Epilepsia 50(Suppl 5): 15-19.
- Viravan S, Go C, Ochi A, Akiyama T, Carter Snead III O, et al. (2011) Jeavons syndrome existing as occipital cortex initiating generalized epilepsy. Epilepsia 52(7): 1273-1279.
- Jennum P, Gyllenborg J, Kjellberg J (2011) The social and economic consequences of epilepsy: a controlled national study. Epilepsia 52(5): 949-956.
- Juarez-Garcia A, Stokes T, Shaw B, Camosso-Stefinovic J, Baker R (2006) The costs of epilepsy misdiagnosis in England and Wales. Seizure 15(8): 598-605.
- Velis D, Plouin P, Gotman J, da Silva FL (2007) Neurophysiology IDSo recommendations regarding the requirements and applications for long-term recordings in epilepsy. Epilepsia 48(2): 379-84.
- Wang XL, Bao JX, Deng YC, Zhao G, Swa B, et al. (2014) Jeavons syndrome in China. Epilepsy & Behavior 32: 64-71.
- Viravan S, Go C, Ochi A, Akiyama T, Carter Snead III O, et al. (2014) Jeavons syndrome existing as occipital cortex initiating generalized epilepsy. Epilepsia 52(7): 1273-1279.
- Sadleir LG, Vears D, Regan B, Redshaw N, Bleasel A, et al. (2012) Family studies of individuals with eyelid myoclonia with absences. Epilepsia 53(12): 2141-2148.
- Japaridze G, Kasradze S, Lomidze G, Zhizhiashvili L, Kvernadze D, et al. (2016) Focal EEG features and therapeutic response in patients with juvenile absence and myoclonic epilepsy. Clinical Neurophysiology. 127(2): 1182-1187.






























