Spinal Clear Cell Meningioma without Dural Attachment: Case Report and Review of Literature
Kais Maamri1*, Mohamed Amine Hadj Taieb1, Ghassen Elkahla1, Maher Hadhri1, Souheil Khalfaoui1, Manel Njima2, Beya Soula1 and Mehdi Darmoul1
1Department Neurosurgery, Faculty of Medicine of Monastir, Fatouma Bourguiba Hospital, Tunisia
2Department of Pathology, Faculty of Medicine of Monastir, Fatouma Bourguiba Hospital, Tunisia
Submission: July 8, 2020; Published: November 05, 2020
*Corresponding author: Kais Maamri, Department Neurosurgery, Fatouma Bourguiba Hospital, Faculty of Medicine of Monastir, Monastir, Tunisia
How to cite this article: Kais M, Mohamed A H T, Ghassen E, Maher H, Souheil K, et al. Spinal Clear Cell Meningioma without Dural Attachment: Case Report and Review of Literature. Open Access J Neurol Neurosurg 2020; 14(3): 555889.DOI: 10.19080/OAJNN.2020.14.555889.
Abstract
Background: Clear Cell Meningioma (CCM) is a very rare histologic subtype of meningioma usually affecting younger patient. The reported data on spinal CCMs are extremely rare. Furthermore, only few cases without dural attachment have been reported in literature.
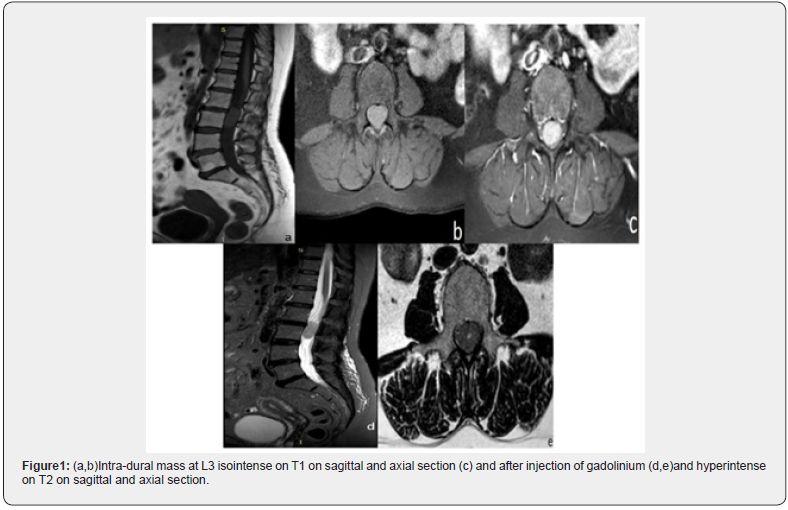
Methods: We report a case of a 58-year-old female patient who was presented to our department with pain in her lower back and bilateral sciatica for 6 months. Magnetic resonance imaging (MRI) showed an intra-dural well demarcated lesion at L3. The mass had an iso-intense signal on both T1 and T2 weighted images with intense and homogeneous gadolinium enhancement.
Result: Via a posterior approach, a total resection was possi¬ble due to lack of dural adhesion of the tumor. Histologic diagnosis was clear cell meningioma. Patient’s recovery course after the operation was uneventful.
Conclusion: Gross total resection is recommended in treating spinal CCM whenever possible. However, radiotherapy could be considered for patients who have undergone STR or younger patients, regardless of the extent of resection.
Keywords:Clear cell; Meningioma; Spine; Dural attachment; Lumbar
Introduction
Clear Cell Meningioma (CCM) is a rare histologic subtype of meningioma. It accounts for less than 1% of all meningiomas [1]. Compared to ordinary meningiomas, CCMs have higher recurrence rate (~50%) and higher tendency to metastasize (4.1%) [2,3]. For these reasons, the World Health Organization (WHO) classification system has classified them as grade II tumors. Among the few CCMs’ reported cases, the majority of them had an intracranial location. Intra-spinal CCMs were even rarer since only less than 100 cases have been reported until 2019 [4]. Most meningiomas are attached to the dura mater, therefore it is exceptional to witness a meningioma without any dural attachment. To the day we speak, only 19 cases of non-dura attached spinal CCM have been reported [4]. In this article, we present an unusual case of a spinal CCM characterized by the absence of dural attachment
Case Report
A 58-year-old female patient was admitted with complaints of low back pain and bilateral sciatica. Her symptoms started 6 months before her admission and have worsened over time. The patient took a symptomatic treatment without any amelioration. On examination, her general condition as well as her cardiorespiratory system was normal. The neurologic examination did not reveal any specific signs except a classical lumbar spinal syndrome. Nevertheless, it is important to mention that there was no neurologic deficit. A provisional clinical diagnosis of lumber disc herniation was made and a Magnetic Resonance Imaging (MRI) was suggested. The MRI showed an intra-dural lesion at L3 measuring 31 mm of height. The mass was well demarcated and had an isointense signal on both T1-and T2-weighted images with intense and homogeneous gadolinium enhancement (Figure1). There was no foraminal extension and no associated bone destruction.
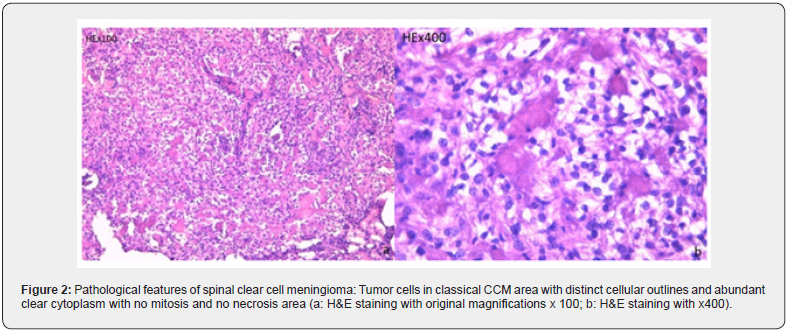
Based on the clinical condition of the patient and the MRI findings, we decided to operate the patient. We started with a L2-L3 laminectomy. The intra-dural exposure revealed an elliptic, encapsulated yellow mass of firm consistency. The tumor was found to be draped by and adhered to the nerve roots without any dural attachment. After an easy dissection, we managed to perform a total resection. On microscopic examination (Figure 2), the tumor was composed of layers of polygonal cells with a clear glycogenrich cytoplasm and monomorphic non-mitotic nuclei. There were prominent perivascular and interstitial collagen. Whorl formation and psammoma bodies were absent. The pathological diagnosis was a CCM (WHO II). The patient’s postoperative course was uneventful. All of her symptoms did disappear and she was able to get up the first day after the operation. A postoperative MRI was scheduled but due to the exceptional situation of COVID19 pandemic, the patient was given an appointment in late 2020 as her case wasn’t judged as urgent.
Discussion

First reported by Manivel and Sung [5] in 1990, CCM is one of the rarest histologic subtype of meningiomas, representing 0.2-0.8% [6-8]. Zorludemir et al. (6) & Oviedo et al. [7] found that this subtype of meningiomas had a higher local recurrence rate and a more aggressive clinical course compared to ordinary meningiomas. These differences led to the classification of a grade II type tumor in 2016 [9]. Around 300 cases of CCMs are reported in the literature, most of them had an intracranial location. The reported data on intraspinal CCMs are extremely rare. To date, only 87 cases of spinal CCMs have been reported since 1996, and only 19 of them had no dural attachment. Detailed information is documented in (Table 1). However, it is noteworthy that the proportion of spinal to total meningiomas is higher for CCMs (45%) than for other meningiomas (the highest being 20% of the reported cases) [10]. In 2019, Zhang et al. (4) found that CCMs mostly attack young patient with a mean age at resection of 24 years old. Amazingly, 36 (42.9%) patients suffered from spinal CCM at an age of under 18 years. As it is the case of other meningiomas, CCMs have a slight female predominance with a female to male ratio at 1.7:1 (53 vs 31). In our review, 37 (42%) patients were under 18 years old and the mean age at resection was 24.6 years. 56 (63.6%) patients were female, 32 (36.4%) patients were male and the female-to-male ratio was 1.75:1. As for the most affected spinal region, the ordinary meningiomas were located in the thoracic region [11-13] whereas (66.7%) of CCMs were located in the lumbar region [4]. The imaging features of CCMs is very similar to those of ordinary meningiomas [15,16]. The MRI of CCMs often reveals an intradural-extramedullary, well-demarcated, homogeneously enhanced mass. It is isointense on both T1-and T2-weighted images, and demonstrates fairly homogeneous enhancement after the injection of gadolinium [8, 17]. Some cases showed foraminal extension and lacking of dural at-tachment, just like schwannomas [18] and other cases showed even an intramedullary CCM [10]. Because of radiologic and gross morphologic similarities between the spinal meningiomas and other intradural extramedullary spinal tumors such as schwannomas, neurofibromas, and ependymomas, an accurate histological diagnosis is mandatory. Just like any other intra-spinal lesion, the bone destruction by a CCM is rare, it was reported only two times until 2018. Both cases were reported by Jian Yang et al. [19]and they showed serious bone destruction at admission. The rarity of bone destruction may be explained with the fact that neurological symptoms usually appear before bone involvement due to the limited space of spine canal, especially in the lumbosacral region. Histologically, CCM contains layers of clear, glycogen-rich (Periodic acid-Schiff positive, diastase-labile), polygonal cells forming only a few vague whorls [6]. Its abundant glycogen is the reason why it is called a clear cell meningioma [14]. These cells are almost Immunoreactive (IR) to Epithelial Membrane Antigen (EMA) and vimentin, while not IR to GFAP, S-100, CK and SMA, with a ki67 index varying from 0 to 40%. The over expression of EGFR, PDGF-receptor and VEGF in CCMs promotes meningioma cell proliferation, a key process in meningioma angiogenesis, the formation of peritumoral edema, and the tumor aggressiveness [15,16]. The potential aggressiveness and recurrence are the main reason of the very challenging management of this tumor [20-45]. For now, for spinal CCMs, total resection should be considered as the optimal treatment. In our review of literature, 79 (89.77%) cases received Gross Total Resection (GTR) as the optimal treatment. However, 20 cases of spinal CCMs (22.72%) still experienced one or more recurrences until the last follow up. The use of postoperative radiotherapy has been increasingly affirmed and highlighted in the treatment of intracranial CCMs [3,21]. However, because of its rarity, the efficacy of postoperative radiotherapy for spinal CCM cannot be irrefutably concluded, therefore it requires further investigation. Tao et al. [21] reported that radiotherapy should not be performed immediately after the first operation of spinal CCMs, because the recurrence rate is lower than the one of intracranial CCM. This may be explained by the higher rate of GTR in spinal CCMs. According to the reported data, it is evident that spinal CCMs are more aggressive, with a much greater progression rate (38.0%) after initial treatment compared with ordinary spinal meningiomas (~3%) [13]. Jiu Hong Li et al. showed in their study that younger patients had better evolution after treatment (54.2%) compared with older ones (23.1%) [22, 46-53].
Conclusion
Spinal CCM, a rare subtype of meningioma, is an aggressive neoplasm with a high rate of local recurrence. It has a predilection for younger patients, and it is mostly located in the lumbar spine. Commonly, the spinal CCM is attached to the dura mater and it is exceptional to see a non-dura linked CCM. Gross total resection remains recommended in treating spinal CCM whenever it is possible. However, radiotherapy could be considered for patients who have undergone subtotal resection or for younger patients, regardless of the extent of resection [54-56].
References
- Li P, Yang Z, Wang Z, Zhou Q, Li S, et al. (2016) Clinical features of clear cell meningioma: a retrospective study of 36 cases among 10,529 patients in a single institution. Acta Neurochir (Wien) 158(1):67‑
- Jallo GI, Kothbauer KF, Silvera VM, Epstein FJ (2001) Intraspinal clear cell meningioma: diagnosis and management: report of two cases. Neurosurgery 48(1):218‑2
- Zhang H, Ma L, Wang YB, Shu C, Kuang W(2017) Intracranial Clear Cell Meningiomas: Study on Clinical Features and Predictors of Recurrence. World Neurosurg 97: 693-700.
- Zhang H, Ma L, Shu C, Dong LQ, Ma YQ, et al. (2019) Spinal Clear Cell Meningiomas: Clinical Features and Factors Predicting Recurrence. World Neurosurg 134: e1062-e1076.
- Manivel JC, Sung JH (1990) Pathology of meningiomas. Pathol Annu 25 Pt 2:159‑1
- Zorludemir S, Scheithauer BW, Hirose T, Van Houten C, Miller G, et al. (1995) Clear cell meningioma. A clinicopathologic study of a potentially aggressive variant of meningioma. Am J Surg Pathol19(5):493‑
- Ohba S, Sasaki H, Kimura T, Ikeda E, Kawase T(2010) Clear cell meningiomas: three case reports with genetic characterization and review of the literature. Neurosurgery 67(3):E870-871; discussion E871.
- Lee W, Chang KH, Choe G, Chi JG, Chung CK, et al. (2000) MR imaging features of clear-cell meningioma with diffuse leptomeningeal seeding. AJNR Am J Neuroradiol 21(1):130‑13
- Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D (2016) The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol (Berl) 131(6):803‑8
- Park SH, Hwang SK, Park YM (2006) Intramedullary clear cell meningioma. Acta Neurochir (Wien) avr 148(4):463‑46
- Solero CL, Fornari M, Giombini S, Lasio G, Oliveri G, Cimino C, et al. Spinal meningiomas: review of 174 operated cases. Neurosurgery 25(2):153‑1
- Spinal meningiomas: surgical management and outcome.
- Raco A, Pesce A, Toccaceli G, Domenicucci M, Miscusi M, et al. (2017) Factors Leading to a Poor Functional Outcome in Spinal Meningioma Surgery: Remarks on 173 Cases. Neurosurgery 80(4):602‑60
- Payano M, Kondo Y, Kashima K, Daa T, Yatsuka T, et al. (2004) Two cases of nondura-based clear cell meningioma of the cauda equina. APMIS Acta Pathol Microbiol Immunol Scand févr 112(2):141‑14
- Oviedo A, Pang D, Zovickian J, Smith M (2005) Clear cell meningioma: case report and review of the literature. Pediatric and Developmental Pathology 8(3):386‑3
- Dhall SS, Tumialán LM, Brat DJ, Barrow DL (2005) Spinal intradural clear cell meningioma following resection of a suprasellar clear cell meningioma. Case report and recommendations for management. J Neurosurg103(3):559‑5
- Wang XQ, Huang MZ, Zhang H, Sun FB, Tao BB, et al. (2014) Clear cell meningioma: clinical features, CT, and MR imaging findings in 23 patients. J Comput Assist Tomogr 38(2):200‑20
- Chen MH, Chen SJ, Lin SM, Chen MH(2004) A lumbar clear cell meningioma with foraminal extension in a renal transplant recipient. J Clin Neurosci Off J Neurosurg Soc Australas. Août 11(6):665‑66
- Jian Yang, Wei Wan, Weibo Liu, Jian Jiao, Qi Jia, et al. (2018) Two novel cases of spinal clear cell meningioma with vertebra involvement. J Orthop Sci S0949-2658(18): 30329-3034.
- Liu PI, Liu GC, Tsai KB, Lin CL, Hsu JS (2005) Intraspinal clear-cell meningioma: case report and review of literature. Surg Neurol 63(3):285‑288 ; discussion 288-289.
- Tao X, Dong J, Hou Z, Hao S, Zhang J, et al. (2018) Clinical Features, Treatment, and Prognostic Factors of 56 Intracranial and Intraspinal Clear Cell Meningiomas. World Neurosurg111:e880‑e88
- Li J, Zhang S, Wang Q, Cheng J, Deng X, et al. (2019) Spinal Clear Cell Meningioma: Clinical Study with Long-Term Follow-Up in 12 Patients. World Neurosurg 122:e415‑e4
- Wu L, Fang J, Yang J, Jia W, Xu Y (2019) Clinical features and surgical outcomes of spinal clear cell meningioma: An institutional experience. J Clin Neurosci 69:55‑
- Inoue T, Shitara S, Ozeki M, Nozawa A, Fukao T, et al. (2018) Hereditary clear cell meningiomas in a single family: three-cases report. Acta Neurochir (Wien) 160(12):2321‑232
- Kawasaki Y, Uchida S, Onishi K, Okanari K, Fujiki M (2013) Pediatric nondura-based clear cell meningioma of the cauda equina: case report and review of literature. Br J Neurosurg 34(2): 215‑
- Tauziede-Espariat A, Parfait B, Besnard A, Lacombe J, Pallud J, et al. (2018) Loss of SMARCE1 expression is a specific diagnostic marker of clear cell meningioma: a comprehensive immunophenotypical and molecular analysis. Brain Pathol 28(4):466‑4
- Wu L, Yang C, Liu T, Fang J, Yang J, et al. (2017) Clinical features and long-term outcomes of pediatric spinal meningiomas. J Neurooncol. Juin 133(2):347‑3
- Smith MJ, Ahn S, Lee JI, Bulman M, Plessis D du, et al. (2017) SMARCE1 mutation screening in classification of clear cell meningiomas. Histopathology 70(5):814‑8
- Kim CH, Chung CK, Lee SH, Jahng TA, Hyun SJ, et al. (2016) Long-term recurrence rates after the removal of spinal meningiomas in relation to Simpson grades. Eur Spine 25(12):4025‑40
- Evans LT, Van Hoff J, Hickey WF, Smith MJ, Evans DG, et al. (2015) SMARCE1 mutations in pediatric clear cell meningioma: case report. J Neurosurg Pediatr 16(3):296‑
- Meguins LC, Ellakkis RF, Adry RAR, Morais DF (2014) Lumbo-sacral clear cell meningioma: Case report and review of the literature. Chir Turin27:337‑33
- Balogun JA, Halliday W, Bouffet E, Kulkarni AV (2013) Spinal clear cell meningioma in a 3-year-old: a case report. Pediatr Neurosurg 49(5):311‑31
- Zhang J, Shrestha R, Li J, Shu J (2013) An intracranial and intraspinal clear cell meningioma. Clin Neurol Neurosurg. 115(3):371‑37
- Kobayashi Y, Nakamura M, Tsuji O, Iwanami A, Ishii K, et al. (2013) Nondura-based clear cell meningioma of the cauda equina in an adult. J Orthop Sci 18(5):861‑86
- Ko JK, Choi BK, Cho WH, Choi CH (2011) Non-dura based intaspinal clear cell meningioma. J Korean Neurosurg Soc 49(1):71‑7
- Prayson RA, Chamberlain WA, Angelov L (2010) Clear cell meningioma: a clinicopathologic study of 18 tumors and examination of the use of CD10, CA9, and RCC antibodies to distinguish between clear cell meningioma and metastatic clear cell renal cell carcinoma. Appl Immunohistochem Mol Morphol18(5):422‑42
- Tong tong W, Li juan B, Zhi L, Yang L, Bo ning L, et al. (2010) Clear cell meningioma with anaplastic features: case report and review of literature. Pathology - Research and Practice 206(5):349‑3
- Nakajima H, Uchida K, Kobayashi S, Takamura T, Yayama T, et al. (2009) Microsurgical excision of multiple clear cell meningiomas of the cauda equina: a case report. Minim Invasive Neurosurg52(1):32‑3
- Chaim B Colen, Mahmoud Rayes, Jamal McClendon, Raja Rabah, Steven D Ham (2009) Pediatric spinal clear cell meningioma. Case report J Neurosurg Pediatr 3(1): 57-60.
- Greene S, Nair N, Ojemann JG, Ellenbogen RG, Avellino AM (2008) Meningiomas in children. Pediatr Neurosurg 44(1):9‑
- Jain D, Sharma MC, Sarkar C, Suri V, Garg A, et al. (2007) Clear cell meningioma, an uncommon variant of meningioma: a clinicopathologic study of nine cases. J Neurooncol81(3):315‑3
- Vural M, Arslantaş A, Ciftçi E, Artan S, Atasoy MA (2007) An unusual case of cervical clear-cell meningioma in pediatric age. Childs Nerv Syst 23(2):225‑22
- Epstein NE, Drexler S, Schneider J (2005) Clear cell meningioma of the cauda equina in an adult: case report and literature review. J Spinal Disord Tech 18(6):539‑5
- Jia Y, Zhong D, Cui Q (2005) Intraspinal clear cell meningioma: a case report. Chin Med J (Engl)118(4):348‑34
- Boet R, Ng HK, Kumta S, Chan LC, Chiu KW, et al.(2004) Lumbosacral clear-cell meningioma treated with subtotal resection and radiotherapy. Journal of Clinical Neuroscience 11(4):432‑43
- Carrà S, Drigo P, Gardiman M, Perilongo G, Rigobello L (2003) Clear cell meningioma in a 22-month-old male: update after five years. Pediatr Neurosurg38(3):162‑16
- Yu KB, Lim MK, Kim HJ, Suh CH, Park HC, et al. (2002) Clear-cell meningioma: CT and MR imaging findings in two cases involving the spinal canal and cerebellopontine angle. Korean J Radiol 3(2):125‑12
- Park HC, Sohn MJ, Kim EY, Han HS, Park HS (2000) Spinal clear cell meningioma presented with progressive paraparesis in infancy. Childs Nerv Syst 16(9):607‑6
- Heth JA, Kirby P, Menezes AH (2000) Intraspinal familial clear cell meningioma in a mother and child. Case report. J Neurosurg93(2 Suppl):317‑3
- Alameda F, Lloreta J, Ferrer MD, Corominas JM, Galitó E, Serrano S(1999) Clear cell meningioma of the lumbo-sacral spine with chordoid features. Ultrastruct Pathol23(1):51‑5
- Dubois A, Sévely A, Boetto S, Delisle MB, Manelfe C (1998) Clear-cell meningioma of the cauda equina. Neuroradiology40(11):743‑74
- Matsui H, Kanamori M, Abe Y, Sakai T, Wakaki K (1998) Multifocal clear cell meningioma in the spine: a case report. Neurosurg Rev 21(2‑3):171‑17
- Cancès C, Chaix Y, Karsenty C, Boetto S, Sévely A, et al. (1998) [Clear cell meningioma: recurrent intraspinal tumor in a child]. Arch Pediatr 5(7):758‑7
- Pimentel J, Fernandes A, Pinto AE, Fonseca I, Moura Nunes JF, et al. (1998) Clear cell meningioma variant and clinical aggressiveness. Clin Neuropathol 17(3):141‑14
- Holtzman RN, Jormark SC (1996) Nondural-based lumbar clear cell meningioma. Case report J Neurosurg 84(2):264‑26
- Prinz M, Patt S, Mitrovics T, Cervós-Navarro (1996) Clear cell meningioma: report of a spinal case. Gen Diagn Pathol 141(3‑4):261‑267.






























