Malignant Peripheral Nerve Sheath Tumor: A Case Report in a 8-Year-Old Patient
Juan L Segura Masís, Edgar Jiménez Masis*, Mónica Nuñez, Juan Luis Segura Valverde, Justiniano Zamora Chaves
Department of Neurosurgery, National Children Hopsital Costa Rica
Submission: June 05, 2020; Published: July 02, 2020
*Corresponding author: Edgar Jiménez Masis, Department of Neurosurgery, National Children Hospital Costa Rica
How to cite this article: Juan L S M, Edgar J M, Mónica N, Juan L S V, Justiniano Z C. Malignant Peripheral Nerve Sheath Tumor: A Case Report in a 8-Year-Old Patient. 2020; 13(5): 555871.DOI: 10.19080/OAJNN.2020.13.555871.
Abstract
Background
Malignant tumors of the Peripheral Nerve Sheath (MPNST) are extremely rare tumors that occur mainly in adulthood. These tumors are mainly present on the trunk and lower limbs with a high association with neurofibromatosis 1
Case report
A 8 years-old male patient without NF1 with a mass at the L3 level of the vertebral column that dilates the right neural foramen and compressed the spinal cord, probably related to neoplasia of the nervous sheath. The tumor corresponded MPNST according to pathology. The diagnostic approach and management are presented, highlighting the complications and sequelae during the evolution of the patient.
Conclusion
It is important to be aware of the existence of the MPNSTs because despite their low incidence, they constitute a very aggressive type of tumor, and should be considered upon the detection of a tumor located at paravertebral level or limbs, especially in patients with NF1. The main treatment is a complete surgical resection due to the high rate of recurrence and limited therapeutic response to radiotherapy and chemotherapy. Also, it is important to remember that the absence of NF1 does not exclude the diagnosis of MPNST.
Keywords:Malignant tumors; Peripheral nerve sheath; limbs; Radiotherapy; Diagnosis; Soft tissue sarcomas
Introduction
Malignant tumors of the peripheral nerve sheath are extremely rare soft tissue sarcomas (with an incidence of 0.001% in the general population and 0.16% of patients with neurofibromatosis type 1 (NF1)) [1] that arise predominantly from Schwann cells [2] and occur mainly in adulthood[3,4]. Its appearance is mainly associated with neurofibromatosis type 1 (Recklinghausen’s disease) and the election treatment is the complete resection of the lesion with extended margins [5,6].
Clinical case
Male patient, 8 years old, with a history of occasional pain at the right knee level for 6 months, mainly of nocturnal occurrence, that was relieved with acetaminophen. He did not present a limitation for mobilization or to execute his daily activities, however the pain exacerbated after 22 days and it was characterized by pain in both knees, intermittent pattern and associated with low back pain that on this occasion did not improve with analgesia. Patient reported that pain was oppressive and because of that, he walked slower and with loss of strength in the lower extremities. No edema, heat, erythema on knees. He did not present arthralgias in other joints or weight loss, fever or history of falls or traumas. In the initial physical examination, the only evident sign was a slight hypotrophy of the right hamstring muscle. Due to not having a clear diagnosis, it is decided to admit the patient to complete studies. First, he had hip x-rays and abdominal ultrasound, which were within normal limits. Afterwards, a tomography with double contrast medium of the abdomen and pelvis was performed, which showed a mass at the L3 level of the vertebral column that dilates the right neural foramen and compressed the spinal cord, probably related to neoplasia of the nervous sheath.
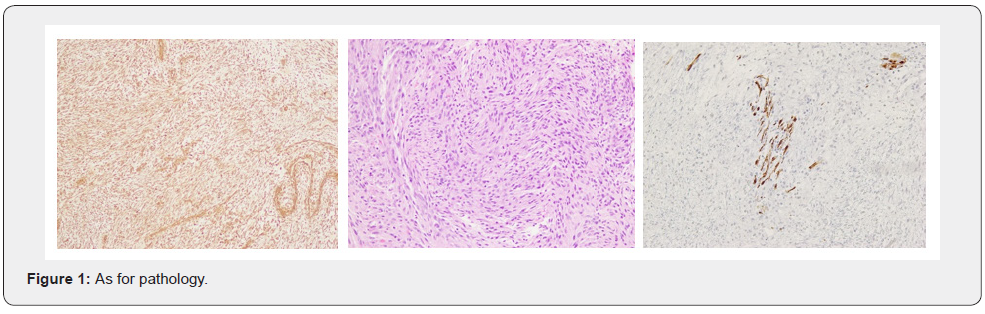
Once the lesion is evidenced, surgery is carried out, which consisted of a laminotomy from T12 to L5, where an extradural tumor of 4x2x3 cm was found that projected towards the right conjunctival hole. When the dura was opened, a solid tumor measuring 2x2x3 cm was observed, displacing the nerve roots contralaterally and, furthermore, that lesion originated from the nerve roots of L2-L3, which had to be removed. Approximately 95% of the total of the lesion found is removed, the displaced vertebral sheets were repositioned and fixed with microplates (Figure1). The patient evolves satisfactorily without neurological deterioration added to that previously described and is discharged with scheduled appointment to perform Magnetic Resonance Imaging (MRI) control. At the post-operative appointment, the MRI is evaluated, and it is described as: At the level of the right foramen of L3 there is a mass already known in the patient that originates intradurally and extends through the intervertebral foramen towards the vertebral region. Located below the right psoas muscle, the lesion in its largest diameters reaches 3.1 cm CC x 1.6 cm T and 1.9 cm in AP, without producing evident infiltration of the psoas muscle or clear erosions of the vertebra. The other foramina are preserved. IDx: Mass of the right nerve root on the foramen of L3. At the moment, there are no other radicular lesions. In a second surgery, a horizontal lateral incision is made on the right iliac crest, it is dissected by planes until it reaches the right psoas, retroperitoneal fat and right paravertebral tumor are observed. Once located and with the help of electrical potentials, the nerve fibers of L3 and L4 are dissected, achieving maximum resection. In the same way, the patient evolves satisfactorily. The patient is neurologically evaluated at the control appointment where only hyperesthesia is detected in the distal L3 territory
Discussion
Malignant tumors of the peripheral nerve sheath are tumors that are derived from Schwann cells or pluripotent cells of the neural crest [3], also there have been reports of MPNST that originated from cranial nerves [6] and also from the parapharyngeal space [7].This type of neoplasia is rare (0.001% in the general population and 0.16% in patients with neurofibromatosis type 1) [3] and very aggressive, which usually occur in adulthood, where its location will be mainly in trunk and lower extremities (ciatic nerve [8]), in addition to this, they have a high association to neurofibromatosis type 1. [5] These tumors occur mainly between 20-50 years old and the cases in children are few [9,10]. In a study carried out by Bates et al, the team found a total of 139 reported cases of MPSNT in patients under 19 years old between 1973 and 2009, and just 5 cases in children between 1 and 4 years old in the SEER (Urvival Epidemiology and End Results) database. They didn´t find significant differences between ethnic groups, although no specific data on Hispanics were mentioned [11]. It is important to recognize this type of tumors within the differential diagnosis since it usually does not cause destruction of the affected nerve and presented a little specific symptomatology [8]. The Mayo Clinic conducted one of the most important studies in this topic. They examinated the files from 1912 to 1983 in which registered 120 patients with MPNST. Also this helped to determine which symptoms appeared more often being pain, enlarged mass and nerve deficit the ones who were found in most patients [12] The recurrence of these lesions is described between 32 to 65% with an interval of 5 to 32 months [13,5], distant metastasis is present in 40 to 68% of the patients [5,13] and the treatment of choice is complete resection with wide margins which will be subjected to the location of the tumor reaching ranges of 20% in paraspinal lesions and 95% in lesion limbs [8,5,14].
References
- Megha Ralli, Sunita Singh, Sonia Hasija, Renuka Verma (2015) Intrathoracic Malignant Peripheral Nerve Sheath Tumor: Histopathological and Immunohistochemical Features. Iran J Pathol 10(1): 74-78.
- E Susan Amirian, J Clay Goodman, Pamela New, Michael E Scheurer (2014) Pediatric and adult malignant peripheral nerve sheath tumors: an analysis of data from the surveillance, epidemiology, and end results program. Texas: J Neurooncol 116(3): 609-616.
- (2016) Retroperitoneal malignant peripheral nerve sheath. Arenas, Ernesto Rueda. Mé Bol Med Hosp Infant Mex 73(3): 188-195.
- Modesto Carli, Andrea Ferrari, Adrian Mattke, Ilaria Zanetti, Michela Casanova, et al. (2005) Pediatric Malignant Peripheral Nerve Sheath Tumor: The Italian and German Soft Tissue Sarcoma Cooperative Group. Rome: J Clin Oncol 23(33): 8422-8430.
- Baena-Ocampo LC, Reyes-Sánchez A, Alpízar-Aguirre A, Rosales-Olivares LM (2009) Tumor de vaina nerviosa periférica maligno asociado a neurofibromatosis tipo 1 Reporte de 2 casos. Cirugía y Cirujanos 391-395.
- Jeffrey A. Stone, Hector Cooper, Mauricio Castillo and Suresh K. Mukherji (2001) Malignant Schwannoma of the Trigeminal Nerve. American Journal of Neuroradiology 22(3): 505-507.
- Massimiliano Sperandio, Isabelle Di Poce, Aurora Ricci, Roberta Di Trapano, Elisa Costanzo, et al. (2013) Malignant Peripheral Nerve Sheath Tumour: CT and MRI Findings. Case reports in radiology.
- RH Hruban, MH Shiu, RT Senie, JM Woodruff (1990) Malignant Peripheral Nerve Sheath Tumors of the Buttock and Lower Extremity. A Study of 43 Cases. Cancer 66(6):1253-1265.
- Modesto Carli, Andrea Ferrari, Adrian Mattke, Ilaria Zanetti, Michela Casanova, et al. (2005) Pediatric malignant peripheral nerve sheath tumor: the Italian and German soft tissue sarcoma cooperative group. J Clin Oncol 23(33): 8422-8430.
- Samin Alavi, MT Arzanian, Yalda Nilipour (2013) Retroperitoneal Malignant Peripheral Nerve Sheath Tumor Replacing an Absent Kidney in a Child. Case Rep Oncol Med 2013: 627472.
- James E Bates, Carl R Peterson, Sughosh Dhakal, Ellen J Giampoli, Louis S Constine (2014) Malignant peripheral nerve sheath tumors (MPNST): A SEER analysis of incidence across the age spectrum and therapeutic intervention in the pediatric population. Pediatric Blood Cancer 61(11): 1955-1960.
- Barbara S Ducatman, T Bernd W Scheithauer, David G Piepgras, Herbert M Reiman, Duane M Ilstrup(1985) Malignant Peripheral Nerve Sheath Tumors A Clinicopathologic Study of 120 Cases. Rochester: Cancer 57(10): 2006-2021.
- Joachim M Baehring, Rebecca A Betensky, Tracy T Batchelor (2003) Malignant peripheral nerve sheath tumor. The clinica spectrum and outcome of treatment. Neurology 61(5): 696-698.
- VF Mautner, RE Friedrich, A von Deimling, C Hagel, B Korf, et al. Malignant peripheral nerve sheath tumors in neurofibromatosis type I MRI supports the diagnosis of malignant plexiform neurofibroma. Neuroradiology 45(9): 618-625.






























