Combined Transcranial and Endonasal Approach to Olfactory Groove Recurrent Meningioma Case Report
Orestes López Piloto*, Tania Margarita Cruz Hernández, Yurledys Jhohana Linares Benavides and Mercedes Rita Salinas Olivares
Department of Neurology, Neurology and Neurosurgery Institute, Cuba
Submission: March 20, 2020; Published: April 20, 2020
*Corresponding author: Orestes López Piloto, Department of Neurology, Neurology and Neurosurgery Institute, Cuba
How to cite this article: Orestes L P, Tania M C H, Yurledys J L B, Mercedes R S O. Combined Transcranial and Endonasal Approach to Olfactory Groove Recurrent Meningioma Case Report. Open Access J Neurol Neurosurg. 2020; 13(3): 555862.DOI: 10.19080/OAJNN.2020.13.555862.
Abstract
Objective: To evaluate the efficacy of combining an endonasal endoscopic approach and transcranial approach in a patient with a recurrent olfactory groove meningothelial meningioma.
Case Report: A 57-years-old female caucasian patient was referred to our institution with a previous history hypertension and a right frontal craniotomy for a World Health Organization (WHO) grade I meningioma with 70% removal of the lesion. A second frontal craniotomy was performed with a 95% resection of the tumor. She received adjuvant treatment with Conformal Radiotherapy (30 sessions) and Nimotuzumab (33 doses). Seven months after was treated surgically for a bone flap osteomyelitis with removal of the bone flap. An endonasal endoscopic transcribiform approach was performed with a partial removal of the lesion. Few weeks after the patient started again with frontobasal soft tissue growing and frontal headache. CT and RMI scans showed regrowing of the tumor. A combined simultaneous endonasal endoscopic approach-transcraneal approach through bilateral frontal craniotomy was performed. There were not intra-operative or postoperative complications. The hospital stay was 9 days.
Conclusion: Olfactory groove meningiomas can extend into the paranasal sinuses. The cranial base and paranasal sinuses are the most common sites of tumor recurrence even after gross total resection. Radical tumor resection, by a combined endonasal and transcranial approach is the best way to reduce the chances of recurrence.
Keywords: Recurrent meningioma; Nasal invasion; Cranio-endoscopic approach
Introduction
Olfactory groove meningiomas arise in the midline over the cribriform plate and occupy the floor of the anterior cranial fossa, extending all the way from the crista galli to the tuberculum sellae [1]. However, in rare cases the tumor may show extension into the nasal cavity and paranasal sinuses, simulating a nasosinusal tumor like esthesioneuroblastoma thus representing a diagnostic and therapeutic challenge [2]. This article presents the result from the surgical treatment of a patient with a recurrent olfactory groove meningioma treated in Neurology and Neurosurgery Institute in order to evaluate the efficacy a combining of endonasal endoscopic approach and transcranial approach. Surgical considerations and a critical literature review is presented.
Case report
A 57-years-old female caucasian patient was referred to our institution with a previous history hypertension and a right frontal craniotomy for a World Health Organization WHO grade I meningioma with 70% removal of the lesion. Four months after she started with facial deformity, and right ocular proptosis. The CT scan showed tumor regrooving and a second frontal craniotomy was performed with a 95% resection of the tumor. The biopsy confirmed a clear cell meningioma (WHO grade II). She received adjuvant treatment with Conformal Radiotherapy (30 sessions) and Nimotuzumab (33 doses). Seven months after was treated surgically for a bone flap osteomyelitis with removal of the bone flap. Eight months after she was referred to our institution with left nasal obstruction left nasal deformity bifrontal headache, anosmia, right ocular pain and bilateral visual loss. There were not cervical lymph nodes associated. The rhinoscopy showed a left nasal tumor surrounded by normal mucosa reaching the nasal septum. The tumor sample was revised and the anatomopathological study reported an esthesioneuroblastoma. The initial laboratory findings were normal. CT revealed a not well-circumscribed isodose tumor with avid contrast enhancement and some necrotic zones in the right ethmoid and frontal sinuses, extended into the soft tissue and anterior cranial base invasion. An endonasal endoscopic transcribiform approach was performed with a partial removal of the lesion. Few weeks after the patient started again with frontobasal soft tissue growing and frontal headache (Figure 1, A-B). CT and RMI scans showed regrowing of the tumor (Figure 1, A-F).
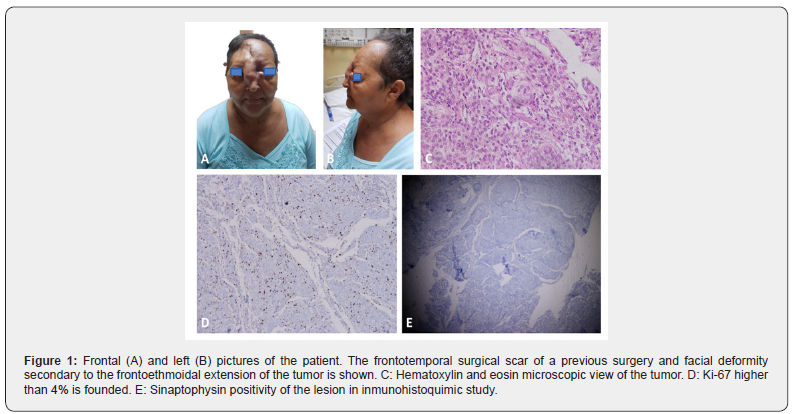
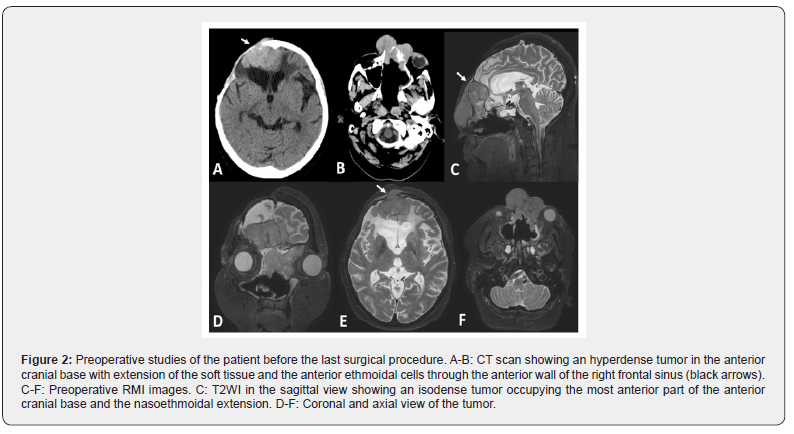
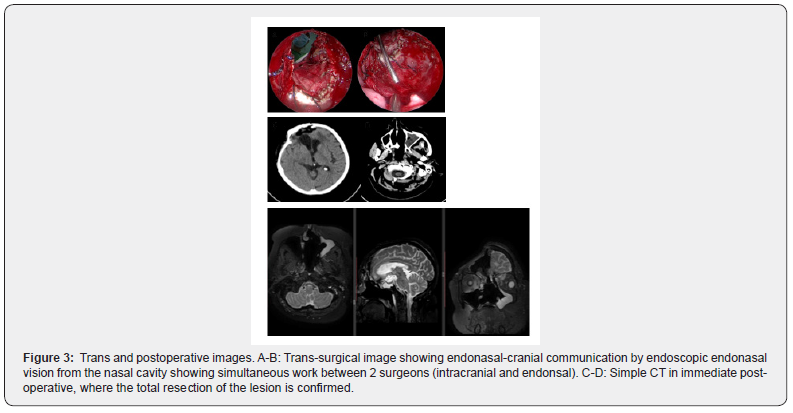
The definitive anatomopathological study showed a meningothelial meningioma (WHO grade I) with Ki-67 higher than 4% and positivity to synaptophysin protein (Figure 1, C-E). Because of the large size of the tumor mass extending into the ethmoid-sphenoidal complex, a combined simultaneous endonasal endoscopic approach-transcraneal approach through bilateral frontal craniotomy was performed. A 0-degree straight and 30-degree endoscopes 4 mm in diameter and 18 cm in length (Karl Storz Endoscopy, Tuttlingen, Germany) were used during the nasal step. A digital endoscopic HD video camera and a full High Definition (HD) flat monitor and a 300 W Xenon light source were used during the procedures. Ceftriaxone was administered via the intravenous route within 1 hour before surgery (1.5 g) and continued for 5 post-operatively (1.5 g twice a day) until nasal packing (Foley balloon) were removed. After orotracheal intubation under general anesthesia, the patient was placed supine with head fixed in the three-point Mayfield-Kees skeletal headrest and turned 10 ̊ - 15 ̊ on the horizontal plane, towards the surgeon. The head was extended 20 degrees to facilitate the anterior cranial base exposure during the endonasal approach and the frontal lobe retraction during the transcranial approach. The nasoethmoidal tumor was removed in a piecemeal fashion. After that, a wide sphenoidotomy was performing in order to expose the postero-inferior margin of the dissection and to use both optocarotid recess as landmarks. A frontotemporal incision and craniotomy was performed. A secondary incision was made in the left naso-orbital region in order to remove the facial component of the tumor. One surgeon dissected the tumor from the inferior (endoscopic) view while a second surgeon dissected the tumor from an intracranial view with a microscope. Thus, four hands, two surgeon’s technique was done (Figure 2).
The frontal sinus was approached by Draft type III sinusotomy that represents the anterosuperior margin of the dissection. The resulting skull base defect was reconstructed by using a multilayer technique with fat, fascia lata and pericranium under endoscopic visualization. A Foley catheter balloon maintained the nasoseptal flap until the fifth day postoperative when it was removed. Surgical bleeding was 900 ml and surgical time was 520 minutes. There were not intra-operative or postoperative complications. The patient was extubated in the operating room and passes the first 48 hours in Intensive Care Unit. The hospital stay was 9 days (Figure 3).
Discussion
Olfactory groove meningiomas account for 8 to 13% of all intracranial meningiomas. This tumor arise in the midline of the anterior fossa along the dura of the cribriform plate and planum sphenoidale [1]. Occasionally, the tumor reaches the paranasal sinuses and nasal cavity by a direct extension and erosion of the bone barrier [2]. The paranasal sinuses are not commonly the primary location of a meningioma [3]. Because this tumor arise from the region of the cribriform plate and the planum sphenoidale, they are in direct relation to the ethmoid and sphenoid sinuses. Derome & Guiot [4] found that 15% of olfactory groove meningiomas has extension to the paranasal sinuses. However, some series of olfactory groove meningiomas fail to report cases with significant tumor extension into the paranasal sinuses [2] Paranasal sinus involvement in the recurrent cases was by direct extension of an olfactory groove meningioma that was not completely removed during primary surgery [5] like in this patient. Due they low growing rate they are commonly diagnosed when their size is significant and causes local pressure initial symptoms. Many patients have asymptomatic meningiomas that have been discovered only during an autopsy [1]. Anosmia is one of the earliest presenting symptoms with more than 50% at the time of diagnosis. Later on, the patients start complaining of headaches and personality changes, such as apathy and abulia. Rarely, seizures as well as aggressiveness which has been reported as a result of frontal lobe dysfunction in some studies. Later stages of this disease can lead to visual problems resulting from compression of the optic nerve or optic chiasm, dementia, urinary incontinence, nasal obstruction and epistaxis. Less commonly patients presented as case of Foster Kennedy syndrome in which the triad of anosmia and unilateral optic atrophy with contralateral papilledema are observed simultaneously. On the other hand, presentation with facial deformity like in this patient is uncommon and related to soft tissue compression [1]. Many different surgical interventions have been recommended [7-10]. Resection has traditionally been performed using a bifrontal or pterional approach, both of which require some degree of brain retraction or manipulation to expose the tumor that affecting the general outcomes [7]. Instead, the purely endoscopic endonasal trans cribriform approach that has been done and reported in certain studies with the advantage of removal of olfactory groove meningiomas without brain retraction and manipulation of neurovascular structures [8,9]. Extracapsular dissection with preservation of the arachnoid planes can be achieved using bimanual microsurgical techniques through a keyhole craniectomy directed at the ventral skull base. However, in patients with significant intracranial extension, soft tissue invasion and nasal component of the tumor, a combined endonasal and transcranial approach is recommended [10]. Excision of these tumors is frequently incomplete because of the surgeon’s tendency to leave the anterior fossa undisturbed for fear of traversing the sinuses and risking a leakage of cerebrospinal fluid. This fact could be the cause of recurrence in this patient [2]. Recurrence in grade I olfactory groove meningiomas can be as high as 41% at 10 years [1].
It is well known that completion of the initial surgical resection is the most important factor in preventing both early and late recurrence of meningiomas (Simpson scale). In a study of four cases of recurrent olfactory groove meningiomas, Snyder et al. [11] found that three of the patients had Simpson Grade 2 resection and one had subtotal resection, but none had both dura and bone resected. All four tumors recurred both inferiorly and posteriorly, with minimal intracranial extensions. Similarly, in our patient, the recurrence was present in the cranial base and paranasal sinuses, and it stemmed from the original conservative handling in the cranial base and soft tissue invasion. If a nasosinusal invasion occur, entering the sinus is not a limiting factor for radical resection. In this context, appropriate reconstruction of the cranial base is the critical factor. Nasoseptal flap and pericanium are the commonest flaps employed in the reconstruction of the anterior cranial base [12].
Conclusion
Olfactory groove meningiomas may extend into the paranasal sinuses. The cranial base and paranasal sinuses are the most common sites of tumor recurrence even after gross total resection. Radical tumor resection by a combined endonasal and transcranial approach is the best way to reduce the chances of recurrence.
References
- Obeid F, Al-Mefty O (2003) Recurrence of olfactory groove meningiomas. Neurosurgery 53(3): 534-43.
- Maiuri F, Salzano FA, Motta S, Colella G, Sardo L (1998) Olfactory groove meningioma with paranasal sinus and nasal cavity extension: removal by combined subfrontal and nasal approach. Journal of Cranio-Maxillofacial Surgery 26(5): 314-317.
- Akai T, Shiraga S, Iizuka H, Kishibe M, Kawami S, et al. (2002) Recurrent meningioma with metastasis to the skin incision. Neurologia medico-chirurgica 44(11): 600-2.
- Derome PJ, Guiot G (1978) Bone problems in meningioma invading the base of the skull. Clin Neurosurg 25: 435-451.
- Spektor S, Valarezo J, Fliss DM, Gil Z, Cohen J, et al. (2005) Olfactory groove meningiomas from neurosurgical and ear, nose, and throat perspectives: approaches, techniques, and outcomes. Operative Neurosurgery 57(4): 268.
- Komotar RJ, Starke RM, Raper DM, Anand VK, Schwartz TH (2012) Endoscopic endonasal versus open transcranial resection of anterior midline skull base meningiomas. World Neurosurg 77(5-6): 713-724.
- Van Gompel JJ, Frank G, Pasquini E, Zoli M, Hoover J, et al. (2011) Expanded endonasal endoscopic resection of anterior fossa meningiomas: report of 13 cases and meta-analysis of the literature. Neurosurg Focus 30: 15.
- Fernandez-Miranda JC, Gardner PA, Prevedello DM, Kassam AB (2009) Expanded endonasal approach for olfactory groove meningioma. Acta Neurochir (Wien) 151: 287-288.
- Gardner PA, Kassam AB, Thomas A, Snyderman CH, Carrau RL, et al. (2008) Endoscopic endonasal resection of anterior cranial base meningiomas. Neurosurgery 63(1): 36-52.
- Attia M, Patel KS, Kandasamy J, Stieg PE, Spinelli HM, et al. (2013) Combined cranionasal surgery for spheno-orbital meningiomas invading the paranasal sinuses, pterygopalatine, and infratemporal fossa. World neurosurgery 80(6): 367-373.
- Snyder WE, Shah MV, Weisberger EC, Campbell RL (2000) Presentation and patterns of late recurrence of olfactory groove meningiomas. Skull Base Surg 10: 131–139.
- Hadad G, Bassagasteguy L, Carrau RL, Mataza JC, Kassam A (2006) A novel reconstructive technique after endoscopic expanded endonasal approaches: vascular pedicle nasoseptal flap. Laryngoscope 116: 1882-1886.






























