Transient Acute Obstructive Hydrocephalus Following Mild Head Injury in an Infant: A Case Report
Anastasia Tasiou*, Christos Tzerefos, Thanasis Paschalis and Kostas N Fountas
Department of Neurosurgery, University Hospital of Larissa, Greece
Submission: March 10, 2020; Published: March 18, 2020
*Corresponding author: Anastasia Tasiou, Department of Neurosurgery, University Hospital of Larissa Biopolis, Building A, 3rd Floor Larissa 41110, Greece
How to cite this article: Anastasia T, Christos T, Thanasis P, Kostas N F. Transient Acute Obstructive Hydrocephalus Following Mild Head Injury in an Infant: A Case Report. Open Access J Neurol Neurosurg. 2020; 13(2): 555859.DOI: 10.19080/OAJNN.2020.13.555859.
Abstract
Head injuries in infants are very common and usually asymptomatic. We report an eleven-month old female, who suffered repeated episodes of emesis caused by a mild head trauma. At the admission, the girl was neurologically intact, but she quickly became deteriorated and drowsy, presenting the setting sun sign. Brain CT scan revealed acute obstructive hydrocephalus at the level of the aqueduct. Even though there was no evidence of intraventicular hemorrhage, we urgently performed an external ventriculostomy in order to control her intracranial hypertension. Afterwards, the neurological signs, as well as the imaging findings, were rapidly improved. Two years follow-up revealed an absolutely normal psychomotor development of the child. To conclude, transient acute obstructive hydrocephalus in children is an uncommon entity and its pathogenesis remains unclear. However, a mild head trauma could be the underlying pathogenic mechanism for this rare clinico-pathological entity.
Keywords: Setting sun sign; Hydrocephalus; Transient hydrocephalus; Mild head trauma/p>
Introduction
Transient acute obstructive hydrocephalus in infants and children is a very rare clinical entity. Among the causes of this pathology could be Central Nervous System (CNS) infections, mild head injuries, and carbon monoxide, lead, and vitamin A or D poisoning [1-10]. Contrariwise, the setting sun sign is frequently seen in infants and children with hydrocephalus. Periaqueductal dysfunction on the basis of raised intracranial pressure is postulated as a possible mechanism of this ocular manifestation [11]. We present a case of an 11-month old, previously healthy, female infant with spontaneous acute obstructive hydrocephalus after a mild head injury.
Case Report
Clinical data
An 11-month old girl was admitted to our department for observation due to a mild head injury. Her parents described that she fell backwards and slightly hit her head. At the admission, she suffered repeated episodes of emesis, but she was neurologically intact. Birth and family history were unremarkable. An hour after her admission, she became deteriorated and drowsy with upward gaze palsy, presenting the setting sun sign.
Diagnostic work-up and surgical management
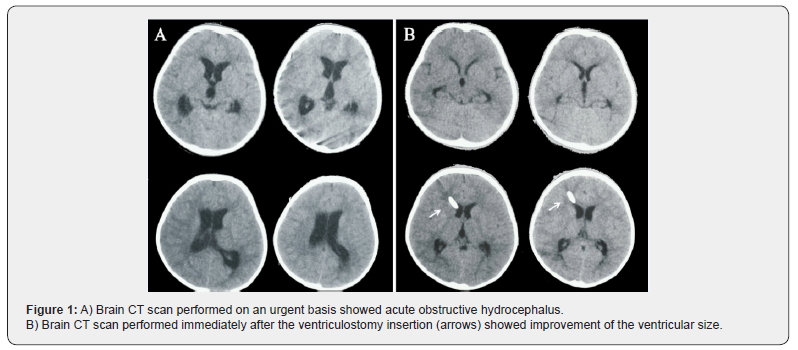
We decided to perform an urgent brain CT scan, in order to identify the cause of her neurological deterioration. The brain CT scan revealed acute obstructive hydrocephalus at the level of the aqueduct (Figure 1A), and the infant directly underwent an external ventriculostomy on an emergent basis, in order to control the intracranial hypertension. A jet of CSF was spurted up into the air through the catheter but there was no evidence of blood tinged. The neurological signs, as well as the imaging findings on the postoperative brain CT scan, were immediately improved after the ventriculostomy insertion (Figure 1B). However, she was transferred intubated to the Pediatric Intensive Care Unit (PICU).
Postoperative findings and outcome
Two days after its insertion the ventricular catheter was removed without clamping or any other maneuver, and the very next day she came back to the neurosurgical ward. Magnetic Resonance Imaging (MRI) of the brain confirmed normal ventricular size and a completely patent aqueduct, with no further pathological signs (Figure 2). Our patient was entirely intact upon her discharge. Two-year clinical follow-up revealed completely normal psychomotor development of the child.

Discussion
Acute obstructive hydrocephalus in infants and children is a rare condition. It is usually caused by mass effect of an intracranial and/or intraventricular lesion [12]. Conversely, upward gaze palsy is a frequent sign, seen in infants and children with hydrocephalus [11]. However, transient acute obstructive hydrocephalus in children is uncommon. According to the literature, the cause of this condition may be the result of an underlying CNS infection, carbon monoxide or lead poisoning, or hypervitaminosis A or D [1- 10]. Another cause could be the occlusion of the aqueduct due to a blood clot following a head trauma. In 1981, Sasaki et al., reported a case of transient obstructive hydrocephalus in an 18-month old boy following a mild head trauma [13]. Several years later, Gupta et. al described a case of an 11-month old infant with aqueductal obstruction caused by a blood clot after a mild head injury [14]. The obstruction was resolved by a ventriculo-peritoneal (VP) shunt insertion [14]. Additionally, Garcia et al. reported the case of an 8-month patient presented with acute hydrocephalus after a head trauma [15]. A blood clot was identified at the level of the aqueduct [15]. However, structural anomalies of the aqueduct can manifest with episodes of hydrocephalus. In 2010, Castellano et al. presented a case of a 4-month old infant with recurrent episodes of transient obstructive hydrocephalus [16]. There was an aqueduct arachnoidal web, which was finally resolved with a third ventriculostomy [16]. Moreover, Vakis et al. described a case of transient acute obstructive hydrocephalus of unknown origin in a 13-month old female infant [17]. In our patient, the imaging workup up showed hydrocephalus with obstruction at the level of the aqueduct without the presence of a lesion and/or hemorrhage, either intraventricular or subarachnoid. Regarding the medical history there was an incident of a mild head injury with no indication of infection or intoxication. As the most common causes of transient hydrocephalus were excluded, the only possible cause of this condition to incriminate was the previously sustained mild head injury.
The actual pathophysiological mechanism of the occlusion of the aqueduct remains unclear in our case. One hypothesis was that formation of a clot led to plugging of the aqueduct [18]. Although, intraventricular or subarachnoid hemorrhage was excluded by brain CT scan in our current case, the possibility of automatic resolution of a clot corresponded to hydrocephalus treatment was not unlike. Another hypothesis was that posttraumatic intracranial hypertension could be the possible mechanism for periaqueductal dysfunction and development of edema, and therefore functional obstruction, which was responsible for the development of hydrocephalus and the associated ocular manifestations presented. Normalization of the intracranial pressure resulted in the resolution of hydrocephalus itself, and its associated symptomatology.
The sunset eye sign is a clinical phenomenon encountered in infants and young children with raised intracranial pressure. It consists of an up-gaze paresis with the eyes appearing driven downward. The lower portion of the pupil may be covered by the lower eyelid, and sclera may be seen between the upper eyelid and the iris. Pathogenesis of this sign seems to be related to the compression of the periaqueductal structures secondary to increased intracranial pressure. However, this phenomenon could be observed in healthy infants, too. There are a few case reports, which have described setting sun eye in normal infants. This benign form may represent immaturity of the reflex systems controlling eye movements [19-23]. When persistent, this sign is one of the most frequent markers of elevated intracranial pressure, appearing in 40% of children with hydrocephalus (of any cause), and in 13% of patients with ventriculo-peritoneal shunt dysfunction [24]. It is an early sign of hydrocephalus, much earlier than increases in head circumference, fontanelle bulging, separation of cranial sutures, and irritability or emesis. Consequently, this sign is a valuable primary warning of an ominous neurological condition requiring prompt neuroimaging and urgent surgical intervention [25]. Certainly, in our case the setting sun sign revealed that the neurological deterioration was due to increased intracranial pressure.
Transient acute obstructive hydrocephalus in infants and children is a rare entity, whose pathogenesis remains unclear. A mild head injury could be one of the eliciting pathogenic mechanisms. Despite that, early diagnosis and immediate surgical intervention, seems to be the best way to efficiently manage it.
References
- Alp H, Tan H, Orbak Z, Keskin H (2005) Acute hydrocephalus caused by mumps meningoencephalitis. Pediatr Infect Dis J 24(7): 657-658.
- Dybey AK, Rao KL (1997) Pathology of post meningitic hydrocephalus. Indian J Pediatr 64(6 Suppl): 30-33.
- Gottrand F, Leclerc F, Chenaud M, Vallee L, Gaudier B (1986) A rare cause of hydrocephalus in an infant: chronic vitamin A poisoning. Arch Fr Pediatr 43(7): 501-502.
- Johnson RT, Johnson KP (1968) Hydrocephalus following viral infection: the pathology of aqueductal stenosis developing after experimental mumps virus infection. J Neuropathol Exp Neurol 27(4): 591-606.
- Prabhu SS, Sharma RR, Gurusinghe NT, Parekh HC (1993) Acute transient hydrocephalus in carbon monoxide poisoning: a case report. J Neurol Neurosurg Psych 56(5): 567-568.
- Romero Garcia-Pelayo D (1952) Case of acute benign hydrocephalus in infant following ingestion of massive doses of vitamin A and D. Acta Pediatr Esp 10(119): 946-947.
- Sharma RR, Chandy MJ, Lad SD (1990) Transient hydrocephalus and acute lead encephalopathy in neonates and infants. Report of two cases. Br J Neurosurg 4(2):141-145.
- So GM, Kosofsky BE, Southern JF (1997) Acute hydrocephalus following carbon monoxide poisoning. Pediatr Neurol 17(3): 270-273.
- Upadhyhya P, Bhargava S, Sundaram KR, Mitra DK, George J, et.al. (1983) Hydrocephalus caused by tuberculous meningitis: clinical picture, CT findings and results of shunt surgery. Z Kinderchir 38(Suppl 2): 76-79.
- Van Toorn R, Rabie H (2005) Pseudocystic cryptococcal meningitis complicated by transient periaqueductal obstruction in a child with HIV infection. Eur J Pediatr Neurol 9(2): 81-84.
- Chattha AS, Delong GR (1975) Sylvian aqueduct syndrome as a sign of acute obstructive hydrocephalus in children. J Neurol Neurosurg Psychiatry 38(3): 288-296.
- Shemie S, Jay V, Rutka J, Armstong D (1997) Acute obstructive hydrocephalus and sudden death in children. Ann Emerg Med 29(4): 258-268.
- Sasaki O, Furasawa Y, Takahara Y (1981) Transient obstructive hydrocephalus of an infant following mild head trauma. No Shinkei Geka 9(3): 407-409 (Jpn).
- Gupta SK, Sharma T (2009) Acute post-traumatic hydrocephalus in an infant due to aqueductal obstruction by a blood clot: a case report. Childs Nerv Syst 25(3): 373-376.
- Garcia Iniguez JP, Madurga Revilla P, Palanca Arias D, Monge Galindo L, Lopez Pison FJ (2013) Transient obstructive hydrocephalus following traumatic brain injury. An Pediatr (Barc) 78(6): 413-420 (Spn).
- Castellano-Chiodo D, Pavone P, Pratico A, Romantshik O, Rossi A, et al. (2010) Recurrent obstructive hydrocephalus in a 4-month-old infant. Child Nerv Syst 26(1): 133-136.
- Vakis AF, Karabetsos DA, Koutentakis DI, Flouris G, Fasoulaki M (2006) Transient acute obstructive hydrocephalus of unknown origin in a 13-month-old infant. Eur J Paediatr Neurol 10(4): 197-201.
- Abubacker M, Bosma JJ, Mallucci CL, May PL (2001) Spontaneous resolution of acute obstructive hydrocephalus in the neonate. Childs Nerv Syst 17(3):182-184.
- Cernerud L (1975) The setting-sun eye phenomenon in infancy. Dev Med Child Neurol 17(4): 447-455.
- Haverkamp F, Weimann E (1995) Familial benign setting-sun phenomenon in healthy newborns. Clin Genet 47(3): 167.
- Kleiman MD, DiMario FJ Jr, Leconche DA, Zalneraitis EL (1994) Benign transient downward gaze in preterm infants. Pediatr Neurol 10(4): 313-316.
- Nejat F, Yazdani S, El Khashab M (2008) Setting Sun Eye in Normal Healthy Infants. Pediatr Neurosurg 44(3): 190-192.
- Yoshikawa H (2003) Benign setting sun phenomenon in full-term infants. J Child Neurol 18(6): 424-425.
- Tzekov C, Cherninkowa S, Gudeva T (1991) Neuroophthalmological symptoms in children treated for internal hydrocephalus. Pediatr Neurosurg 17(6): 317-320.
- Boragina M, Cohen E (2006) An infant with the setting sun eye phenomenon. CMAJ 175(8): 878.






























