Suprasellar Alveolar Hydatid Disease Mimicking a Craniopharyngioma: Diagnostic and Therapeutic Management: Case Report
Berete Ibrahima1*, Diawara Seylan1, Alpha Boubacar Bah1, Cherif Mohamed1, Mohammed Faiz Chaoui2 and Khalid Chakour2
1Department of Neurosurgery, Hassan II University Hospital Fez, Morocco
2Department of Neurosurgery, Donka University Hospital, Conakry, Guinea
Submission: December 20, 2019; Published: January 27, 2020
*Corresponding author: Ibrahima Berete, Department of Neurosurgery, University of Conakry, Guinea
How to cite this article: Berete Ibrahima, Diawara Seylan, Alpha Boubacar Bah, Cherif Mohamed, Mohammed Faiz Chaoui, Khalid Chakour. Suprasellar Alveolar Hydatid Disease Mimicking a Craniopharyngioma: Diagnostic and Therapeutic Management: Case Report. Open Access J Neurol Neurosurg. 00110 2020; 12(5): 555847. DOI: 10.19080/OAJNN.2020.12.555847.
Abstract
We report the case of a 16-year-old female patient with an alveolar hydatid cyst disease referred to our hospital for a rapid bilateral decrease in visual acuity and a seller lesion with suprasellar extension on Brain CT. On Examination she had no other neurologic symptoms and the fundoscopic examination revealed a stage II papilledema. Brain MRI showed a seller and suprasellar cystic lesion resembling a craniopharyngioma. Pituitary function was normal on laboratory testing. Patient underwent surgical resection of the lesion and histopathological examination confirmed the diagnosis of echinococcosis multilobularis. Albendazole Chemotherapy was initiated, and the patient did well postoperatively and at 1 year follow up. The present report intends not only to show a rare case of seller region lesion but also to remind clinicians of the Mediterranean area that Intracranial hydatid cyst is a rare but possible parasitic infestation of the seller region and should be kept in mind in the differential diagnosis of multiloculated cystic mass of that anatomic region
Keywords: Echinococcus multilocularis Hydatid cyst Albendazole Surgery
Introduction
Intracranial hydatid cyst is a rare parasitic infestation and account for 1-2% of all cystic echinococcosis [1]. Hydatid disease is endemic in the Mediterranean region. Several cases of primary hydatid cysts have been reported, however cerebral alveolar echinococcosis has rarely been described [2]. Intracranial hydatid cysts should be removed in tot without rupture. The preoperative diagnosis is a very important step in planning the surgical management.
Case Report
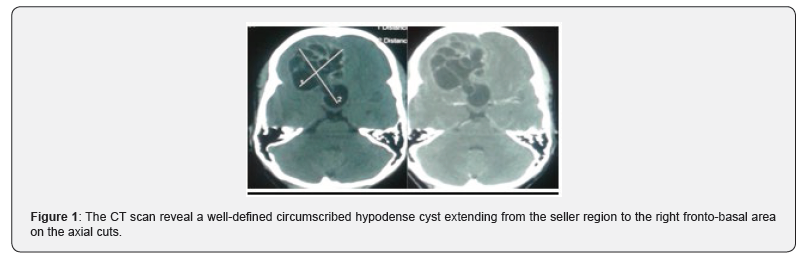
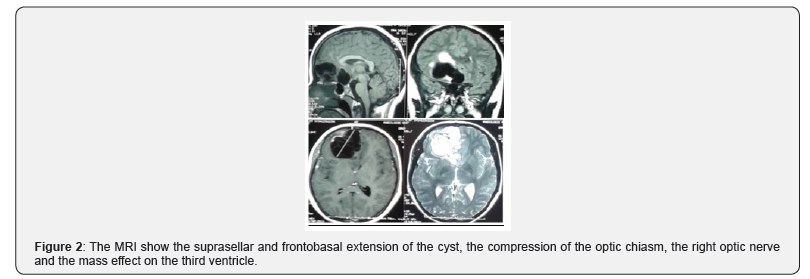
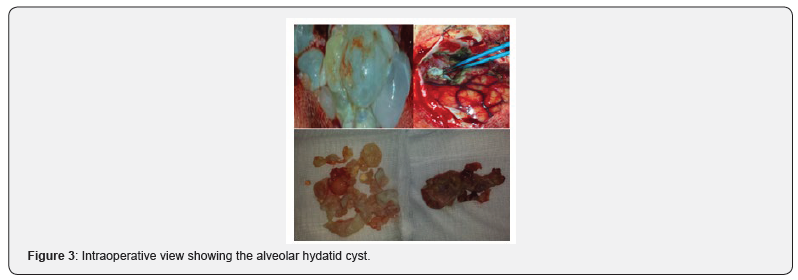
A 16-year-old right-handed female was referred to our department with a 2 weeks history of decreasing visual acuity. There was no past medical history and physical examination was otherwise unremarkable. Brain CT obtained from the referring hospital revealed suprasellar cystic lesions (Figure 1) and MRI of the brain demonstrated increased T2 signal and deviation of the optic chiasma on the right, with patchy lobular wall enhancement following the administration of a contrast agent (Figure 2). A Craniopharyngioma diagnosis was suggested and routine laboratory test, were unremarkable. Chest X ray and Abdominal Ultrasound where normal. A Right frontopterional craniotomy was performed, an alveolar cyst that extended from the dura mater to the rectus gyrus at the optic nerve junction was identified as well as the feeding vessels; The cyst was a large multilobulated firm with an irregular surface, originating from the suprasellar cistern with adhesions to the chiasma and optic tracts, and the right gyrus rectus (Figure 3). The resection was completed along with copious irrigation of the dissection plan with warm saline, leaving a thin layer of cyst wall to vascular structures. Multiples samples were sent for histopathological studies. Postoperatively, the patient was ambulatory, did not have any focal deficit and her visual acuity improved in 3 weeks. The control Brain CT scan were satisfactory. The histopathologic examination showed several multiloculated coalescing cystic structures surrounded by fibrosis. The cysts had a hyaline capsule wall with an inner lining of basophilic matrix containing occasional calcareous corpuscles. This findings along the macroscopic observations were consistent with an alveolar cystic echinococcosis. The patient was treated on one year with Praziquantel 5 mg-Kg. She was neurologically intact, symptom free with a normal visual acuity at 1 year follow up.
Discussion
Primary cerebral hydatid cyst is a rare manifestation of E. multilocuraris that occurs by direct infestation of the brain by the larvae [3]. The commonest site is the supratentorial region on the parietal lobe in the distribution of the middle cerebral territory [4]. A primary cyst is always solitary. Multiple alveolar hydatid cyst is uncommon and develop after embolization from a cardiac cyst [5]. The pathogenesis is still not fully understood. Since the larval masses proliferates indefinitely by exogenous budding and invades the surrounding tissues, they might resemble the appearance and behavior of malignancy [6]. Ingestion of multiple larvae leads to bilateral and multiple primary cerebral lesions. In such cases, larvae pass through the capillary filter of the liver and lungs [7]. Prostoscolioces are rarely observed in samples from infected humans and the parasite is microscopically described as a thin cuticle with non-germinative membrane so the cerebral alveolar hydatid cyst may not be the cause for larval distant metastasis[2]. The symptoms begin when the cyst become large enough to increase the intracranial pressure. Based on the size and location of the lesion clinical manifestations such as headache, vomiting, nausea, papilledema, ambulate, convulsion and hemiparesis can be seen [8]. Neuroimaging, especially MRI, plays the main role in detecting the cerebral hydatid cyst. Alveolar cysts are usually associated with contrast enhancement, perilesional edema and calcification [9]. Extracranial hydatid cyst must be investigated by chest x-ray and abdominal ultrasonography. Serological tests are of less importance and the diagnosis is only confirmed by histopathological examination of the cyst [6]. The preferred treatment for cerebral hydatid cyst is surgery and the patients normally undergo a radical resection [10]. The aim of the surgical procedure is to remove the cyst without rupture to prevent recurrence or anaphylaxis. A large craniotomy is made, and the cyst is opened over that area and removed out while abundantly irrigating the dissection bed with warm saline [11]. In our case, we have to leave a layer of cyst capsule that was firmly attached to the middle cerebral artery branches and the gyrus rectus. Medical therapy with Albendazole carbonate derivatives such as Albendazole and Mebendazole is also necessary. Albendazole is important in intracranial hydatidosis to decrease anaphylaxis and recurrence rate [11]. Prolonged medical treatment is highly recommended for some patients and was applied in our patient due to the subtotal nature of our resection and the complexity of the regional neuro-vascular structures.
Conclusion
Hydatid cyst can involve the seller region mimicking a craniopharyngioma. It is a highly surgical lesion with recurrence being the major concern. Patients should remain on long-termmedical therapy following the surgery for this highly eloquent area and needs long-term follow up.
References
- Ersahin Y, Mutluer S, Guzelbag E (1993) Intracranial Hydatid Cysts in Children. Neurosurgery 33(2): 219-224.
- Senturk S, Oguz KK, Soylemezoglu F (2006) Cerebral alveolar echinoccosis mimicking primary brain tumor. AJNR Am J Neuroradiol 27(2): 420-422.
- Altnors N, Bavbek M, Caner HH, Erdogan B (2000) Central Nervous System Hydatidosis in Turkey: A cooperative study and literature survey analysis of 458 cases. J Neurosurgery 93: 1-8.
- Izci Y, Tüzün Y, Seçer HI, Gönül E (2008) Cerebral hydatid cysts: Technique and pittfalls of surgical management. Neurosurg focus (6): E15.
- Turgut M, Benli K, Erylmaz M (1997) Secondary multiple intracranial hydatid cysts caused by intracerebral embolism of cardiac echinococcosis: an exceptional case of hydatidosis. Case report. J Neurosurg 86(4): 714-718.
- Binesh F, Mehrabanian M, Navabli H (2012) Primary Brain Hydatosis. BMJ Case Report.
- Lunardi P, Missori P, Di-Lorenzo N, Fortuna A (1991) Cerebral hydatidosis in childhood. A retrospective survey with emphasis on longterm follow-up. Neurosurgery 29(4): 515-518.
- Polat P, Kantarci M, Alper F, Suma S, Koruyucu MB (2003) Hydatid disease from head to toe. Radiographics 23(2): 475-494.
- Coates R, Von Sinner W, Rahm B (1990) MR Imaging of Intracranial Hydatid Cyst. AJNR Am J Neuroradiol II:1249-1250.
- Ulutas M, Cinar K, Secer M (2005) Removal of large hydatid cysts with balloon-assisted modification of Downligs method: Technical report. Acta Neurochirurgica Wien 157(7): 1221-1224.
- Gok H, Baskurt O (2019) Giant Primary Intracranial Hydatid Cyst in Child with Hemiparesis. World Neurosurgery 129: 404-406.






























