Number of Coils for Parent Artery Occlusion of Ruptured Vertebral Artery Dissecting Aneurysm Delta Coil Case Series and Literature Review
Masahito Katsuki1,2, Yasuhiro Suzuki1*, Yoshimichi Sato1, Keisuke Sasaki1, Ryo Matsuoka1, Shoji Mashiyama1 and Teiji Tominaga2
1Department of Neurosurgery, Iwaki City Medical Center, Japan
2Department of Neurosurgery, Tohoku University Graduate School of Medicine, Japan
Submission: October 30,2019;Published: December 11, 2019
*Corresponding author: Yasuhiro Suzuki Department of Neurosurgery, Iwaki City Medical Center, 16 Kusehara, Mimayamachi, Uchigo, Iwaki, Fukushima 973-8555, Japan
How to cite this article: Masahito K, Yasuhiro S, Yoshimichi S, Keisuke S, Ryo M, Shoji M, Teiji T. Number of Coils for Parent Artery Occlusion of Ruptured Vertebral Artery Dissecting Aneurysm:Delta Coil Case Series and Literature Review. Open Access J Neurol Neurosurg. 2019; 12(3): 555836. DOI: 10.19080/OAJNN.2019.12.555836.
Abstract
Background: Parent Artery Occlusion (PAO) by simple coiling for Vertebral Artery Dissection (VAD) sometimes needs a large number of coils, increasing both operative time and medical costs. DELTA coils (Johnson and Johnson, USA) provide a homogenous coil distribution and high packing density due to their triangular shape. They have the potential to decrease the number of coils used in PAO. In this study, we retrospectively investigated the number of coils required for PAO using the simple coiling to treat VAD-induced Subarachnoid Hemorrhage (SAH).
Methods: We analyzed 11 of our own SAH patients who underwent PAO for VAD by simple coiling. A literature search was performed using PubMed and Japan Medical Abstracts Society for VAD, endovascular treatment, and coil.
Results: The mean number of coils used in our hospital was 6.8 (3-10); the mean operative time was 77.8 (49-140) minutes. In the literature review, 20 of the 112 acquired reports stated the number of coils used for PAO by simple coiling for VAD-induced SAH. Of the 33 cases in the 20 reports, the mean number of coils used was 10.4 (3-60).
Conclusion: DELTA coils and their characteristic triangular shape have the possibility to save medical costs by reducing the number of coils used for PAO.
Keywords: Vertebral artery dissection Parent artery occlusion Endovascular treatment Coiling; DELTA coils Medical cost Subarachnoid hemorrhage Minimally invasive surgery
Abbrevations: CT: Computed Tomography; DSA: Digital Subtraction Angiography; PAO: Parent Artery Occlusion; SAH: Subarachnoid Hemorrhage; VAD: Vertebral Artery Dissection; VAG: Vertebral Angiography
Introduction
Intracranial Vertebral Artery Dissection (VAD) represents an important cause of ischemic and hemorrhagic stroke, especially in young adults. VAD sometimes causes aneurysms; the intracranial aneurysms associated with VAD frequently rupture and result in massive Subarachnoid Hemorrhage (SAH). These aneurysms tend to rerupture, with a rebleeding rate ranging from 30 to 58% within 24 hours of the initial bleed [1-5]. Therefore, early obliteration of VAD aneurysms should be considered. At present, parent artery occlusion (PAO) viaendovascular procedures is more popular than open surgical treatment for SAH due to VAD-associated aneurysm [4-39].
Endovascular therapy offers clear advantages over open surgical treatment, as it has a dramatically reduced operative time and is minimally invasive [5]. However, PAO by endovascular simple coil embolization sometimes requires multiple coils, up to a total of 60, [8] increasing operative time and medical costs. Rounded and triangular, DELTA coils (Johnson and Johnson, New Jersey, USA) ring precess and establish natural deflection pointsevery quarter millimeter along the initial coil wind, helping coils change direction more easily. This technology provides a more homogenous coil distribution and higher packing density because of the triangular coil shape, increased length, and softness [24]. We posited that DELTA coils could reduce the number of coils used for PAO by the simple coiling technique. We herein report our case series to analyze the number of coils used and compare our findings to that described in previous reports.
Materials and Methods
Retrospective analysis of hospital records
From our hospital’s medical records, we retrieved the data for patients with spontaneous VAD-induced SAH from 2009 to 2019. We only included those who had undergone PAO by simple coiling using DELTA coils for more than 70% of all coils. Data extracted included age, sex, parent artery diameter, dissection maximum diameter and length, number and the total length of coils used, and operative time. Operative time was defined as the period of time from sheath insertion to sheath removal. We obtained written informed consent from all patients for their inclusion in this study; the hospital’s research ethics committee approved this study.
Diagnosis of SAH and spontaneous VAD was based on clinical history, the presence of SAH on Computed Tomography (CT), angiographic findings of dissection including a string sign, tapered stenosis or occlusion or flame-shaped occlusion, intimal flap, dissecting aneurysm, distal pouch on CT angiography, magnetic resonance imaging, and Digital Subtraction Angiography (DSA). Endovascular procedures for VAD weresimilar in all cases; patients underwent DSA under sedation, including left and right Vertebral Angiography (VAG). Dissection maximum diameter and length and parent artery diameter were evaluated. Coil mass was made as tight and small as possible to avoid rerupture and thrombotic complication. Operations were deemed finished when PAO was confirmed.
Literature review
A comprehensive literature review was performed by searching PubMed and Japan Medical Abstracts Society with the keyword’s vertebral artery dissection, endovascular treatment, and coil. Both and OR combinations were used. Inclusion criteria were as follows: reports in English or Japanese including case series and case reports published up to May 2019 with clear, detailed descriptions of VAD-associated SAH pathological condition and endovascular treatment. If an article described cases with other endovascular treatments, such as stentassisted coil embolization, or with other pathological conditions, including ischemic or asymptomatic VAD, trauma, malignant tumor, and extracranial vertebral artery dissection, it was excluded from the analysis. Conference abstracts, review articles, and guidelines were also excluded. Four investigators selected literature independently according to the above inclusion criteria. The initial selection was based on reviewing titles and abstracts. For the second selection, investigators reviewed the full text (where available). Investigators then discussed to find a consensus on which articles to include. From each article, the following clinical information was extracted: age, sex, and number and the total length of coils used. We compared these results to those from our hospital.
Results
Hospital record characteristics
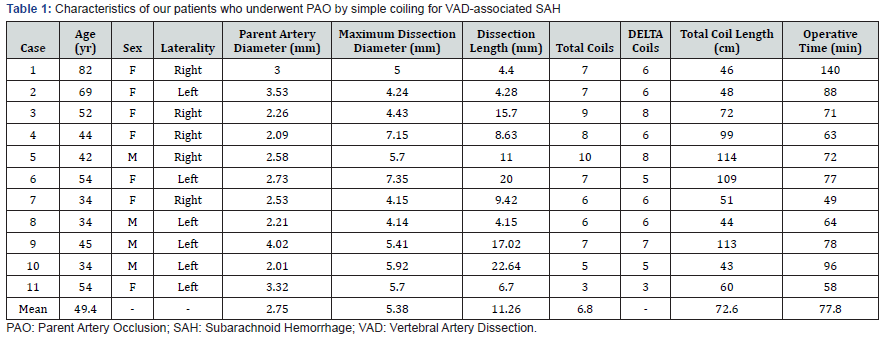
From our medical records, we retrieved the data from 11 patients with VAD-induced SAH. These patients had undergone PAO by simple coiling; DELTA coils made up more than 70% of the total coils. The mean utilization rate of DELTA coils was90% (ranging from 72% to 100%). Overall, four men and seven women were included, and the mean values are summarized in Table 1. The mean number of coils used was 6.8 (3-10); their mean total length was 72.6 (43-114) centimeters. The mean operative time was 77.8 (49-140) minutes. One patient had symptomatic cerebellar infarcts as a perioperative complication; another had postoperative takotsubo cardiomyopathy. Except for three patients whose Hunt and Kosnik grade was V and who died of primary brain injury due to severe SAH, the mean observation period was 57.5 (1-103) months. No patients had recanalization
Representative case (case 6)
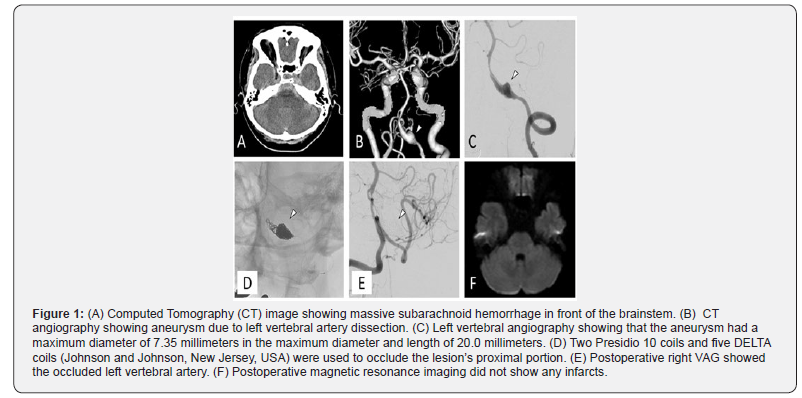
A 54-year-old woman presented to our hospital with a sudden headache and repetitive vomiting. She had a mild disturbance of consciousness (Figure 1). CT showed massive SAH in front of the brainstem (Figure 1A). CT angiography revealed left VAD aneurysm (Figure 1B, arrowhead). We diagnosed her with SAH (Hunt and Kosnik grade II) due to left VAD aneurysm rupture. Under general anesthesia, we performed DSA to evaluate the left VAD aneurysm. The aneurysm had a 7.35-millimeter maximum diameter and was 20.0 millimeters in length (Figure 1C, arrowhead). The parent artery was 2.73 millimeters in diameter. We decided to perform PAO to prevent rerupture and to make the coil mass as tight as possible. Through a six French guiding catheter (Fubuki, Asahi Intecc, Aichi, Japan) from the right femoral artery, an SL-10 microcatheter (Boston Scientific, CA, USA) was advanced over a micro guidewire (Chikai 14, Asahi Intecc, Aichi, Japan) and positioned in the distal part of the dilated portion. Two Presidio 10 coils (Johnson and Johnson, New Jersey, USA) were advanced and successfully detached. Five DELTA coils were deployed to occlude the proximal portion of the lesion (Figure 1D, arrowhead). Postoperative right VAG showed occlusion of the left vertebral artery (Figure 1E, arrowhead). Postoperative magnetic resonance imaging did not show any infarcts in the posterior circulation territory (Figure 1F). The patient was discharged on the 18th postoperative day without any neurological deficits and has lived independently since discharge.
Literature review results
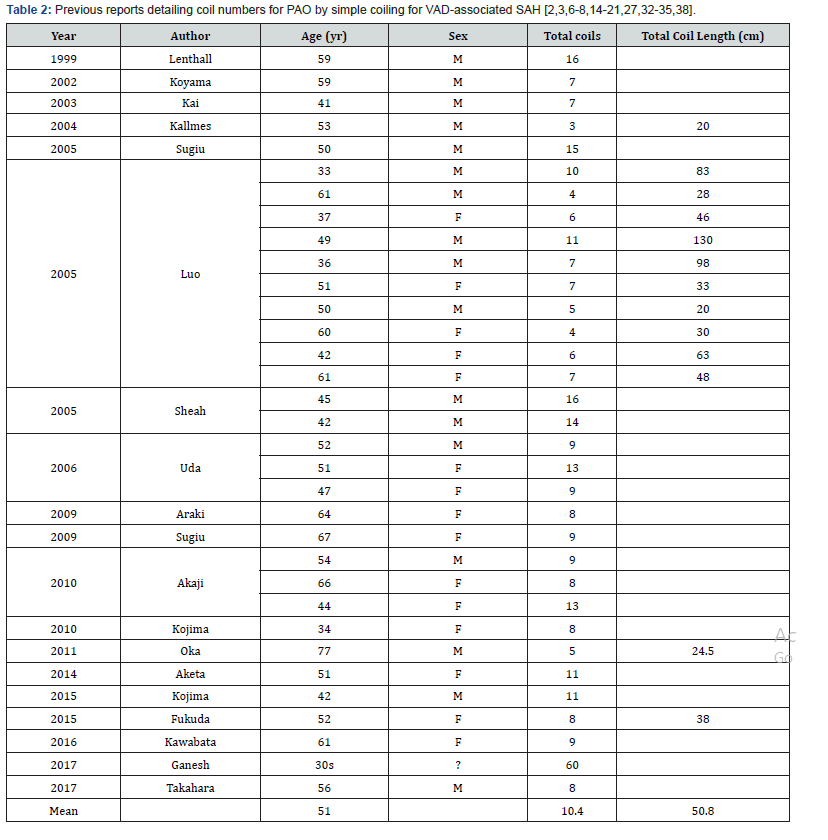
PubMed yielded 368 studies, Japan Medical Abstracts 110. After excluding duplicate studies by reviewing the title, abstracts were screened. Those that failed to meet the inclusion criteria were removed; 160 articles remained. Of those, we acquired 112 reports with full text. Of the 112, 20 studies described the number of coils used and so were eligible for inclusion in the present study [2,3,6-8,14-21,27,32-35,38]. We performed a systematic review using the 20 studies, which comprised 33 cases. Overall, 17 men and 15 women (one patient’s sex was unknown) were included, with a mean age of 51 (33-77) years. The mean number of coils used was 10.4 (3-60); their mean total length was 50.8 (20-130) centimeters (Table 2). We did not know what coil types were used or the operative time.
Discussion
Alternatives for VAD treatment
Open surgical intervention, consisting of proximal ligation of the dissected vessel and clipping or wrapping of the aneurysm, is the traditional VAD treatment [5,12]. However, these procedures need extended operative times and microsurgical techniques [5]. Consequently, alternative endovascular procedures have become more popular [4,12,28,31,39,40]. Economic comparisons between endovascular coiling and clipping for intracranial aneurysms have been performed [26,37,41]. but these do not yet exist for VAD. Solitary stenting and stentassisted coil embolization for ruptured VAD aneurysms reduce the number of coils and preserve blood flow. However, solitary stenting and stent-assisted coil embolization sometimes result in rerupture,[40] recanalization,[1] or aneurysm recurrence [22]. Antithrombotic medications are also generally required due to the thrombogenicity of a stent, contributing to delayed aneurysm thrombosis and the possibility of rerupture. In some cases, sacrificing parent artery flow via the simple coiling technique is preferable in order to guarantee the prevention of fatal rebleeding. Therefore, discussion on PAO by the simple coiling technique is both relevant and valuable.
New hydrogel [15] or fibered coils [10] that favor early thrombosis contribute to a reduction in the total number of coils required for artery occlusion. However, PAO with hydrogel and fibred coils for VAD has not got consensus to reduce coil numbers. Another alternative, a vascular plug, has been developed toreduce the number of coils and costs. The Amplatzer vascular plug (Abbott, Illinois, USA) is composed of an expandable nitinol wire mesh and acts as focal coil and embolic material immobilizer. However, it is porous, so additional coils [11] or several plugs [29] are needed for complete PAO. Therefore, PAO using the simple coiling technique still has relevance despite the rise of new technologies.
Therapeutic and economic effects of coil number reduction
Tight packing is necessary to avoid recanalization due to incomplete thrombosis and ischemic complications resulting from flow obstruction of the many vertebral artery perforating branches [23]. Coils for neuro-endovascular surgery cost approximately 144,000 JPY per unit as of 2019. As such, it is desirable to use as few coils as possible. Furthermore, using many coils requires a long operative time. Longer operative times mean patients and medical staff are exposed to more radiation [13]. Therefore, tight packing and reduced coil numbers are crucial to avoid ischemic complication, save medical costs, and shorten the operative time. In our review, several case reports and case series described the numbers of coils used, but they did not go into detail. Only Grigoryan reported PAO for nonhemorrhagic VAD using a single oversized coil as well as the safety, speed, and cost [9].
Therefore, our case series is one of the few studies highlighting the number of coils used in PAO for VAD. It is also the first report comparing different case and study coil numbers. Of the 160 reports found on PubMed and Japan Medical Abstracts Society discussing PAO for VAD-induced SAH by the simple coiling technique, only 20 described the number of coils used. Although we could not perform further statistical analysis, the mean number of coils used in our DELTA coil approach, 6.8, appears fewer than the 10.4 found in the literature review. We could not clarify whether the reduction of coil numbers contributes to the shortening the operative time. The patient of case one took 140 minutes as the operative time, even though the coil number was seven. This is because she was well aged, so it was difficult and took a long time to advance the guiding catheter and microcatheter due to her severe atherosclerosis. The operative time depends on various factors, so it was uncertain that DELTA coils shorten it via the reduction of coil numbers
Limitations
We only investigated the number of coils used. Other factors, such as radiographic coil density, morphological evaluation, and rheological effects during the procedure, were not taken into account. Whether DELTA coils really reduce coil number is unknown due to a lack of information regarding coil type in the reviewed reports and no statistical analysis. Neither could we analyze operative time since previous reports did not describe it. Accumulation of additional cases detailing this information and further comparative study are required
Conclusion
Reducing the number of coils is important in PAO with the simple coiling technique for VAD-associated SAH. DELTA coils can pack tightly and necessitate smaller coil numbers, therefore contributing to lower medical costs.
Acknowledgement
M Katsuki, Y Suzuki, Y Sato, K Sasaki, R Matsuoka and S Mashiyama contributed to data acquisition. M Katsuki and Y Suzuki wrote the manuscript. T Tominaga conceived the study. All authors have read and approved the final manuscript. We would like to thank Edit age (www.editage.com) for English language editing.
References
- Ahn JY, Han IB, Kim TG, Yoon PH, Lee YJ, et al. (2006) Endovascular treatment of intracranial vertebral artery dissections with stent placement or stent-assisted coiling. AJNR Am J Neuroradiol 27(7): 1514-1520.
- Akaji K, Akiyama T, Hiraga K, Tanizaki Y, Kojima A (2010) Early embolizations for the poorest grade patients with ruptured dissecting aneurysms of the vertebral artery. Surg Cereb Stroke 38(1): 24-28.
- Aketa S, Wajima D, Kotsugi M, Yonezawa T (2014) Subarachnoid hemorrhage due to vertebral artery dissection combined with contralateral vertebral artery occlusion: case report. Curr Pract Neurosurg 24: 1348-1352.
- Albuquerque FC, Fiorella DJ, Han PP, Deshmukh VR, Kim LJ, et al. (2005) Endovascular management of intracranial vertebral artery dissecting aneurysms. Neurosurg Focus 18(2): E3.
- Ali MS, Amenta PS, Starke RM, Jabbour PM, Gonzalez LF, et al. (2012) Intracranial vertebral artery dissections: evolving perspectives. Interv Neuroradiol 18(4): 469-83.
- Araki S, Fujita T, Kawakami M. (2009) Endovascular trapping for a ruptured right vertebral dissecting aneurysm after reconstruction of the occluded left subclavian artery. Japanese J Neurosurg 18: 139-144.
- Fukuda K, Higashi T, Yoshioka T, Shigemori Y, Iwaasa M, et al. (2015) Stent-assisted embolization for ruptured vertebral artery dissection involving the origin of the posterior inferior cerebellar artery: A case report of staged strategy. Neurol Surg 43(4): 331-337.
- Ganesh Kumar N, Ladner TR, Kahn IS, Zuckerman SL, Baker CB, et al. (2017) Parent vessel occlusion for treatment of cerebral aneurysms: Is there still an indication? A series of 17 patients. J Neurol Sci 372: 250-255.
- Grigoryan M, Cordina SM, Khatri R, Hassan AE, Rodriguez GJ (2013) Vessel occlusion using a single long oversized coil in vertebral artery dissection: a technical note. J Neurointerv Surg 5(3): e11.
- Halbach VV, Dowd CF, Higashida RT, Balousek PA, Urwin RW (1998) Preliminary experience with an electrolytically detachable fibered coil. AJNR Am J Neuroradiol 19(4): 773-777.
- Hoit DA, Schirmer CM, Malek AM (2006) Use of the Amplatzer vascular plug as an anchoring scaffold for coil-mediated parent vessel occlusion: technical case report. Neurosurgery 59(1): ONSE171-172.
- Iihara K, Sakai N, Murao K, Sakai H, Higashi T, et al. (2002) Dissecting aneurysms of the vertebral artery: a management strategy. J Neurosurg 97(2): 259-267.
- Imazeki M, Kawasaki K, Hasegawa R, Takahashi H, Suzuki H (2014) Evaluation of patients’ radiation exposure in neuroendovascular therapy estimated dose by questionnaire investigation. J Neuroendovascular Ther 8: 305-312.
- Kai Y, Hamada J-I, Morioka M, Todaka T, Mizuno T, et al. (2003) Endovascular coil trapping for ruptured vertebral artery dissecting aneurysms by using double microcatheters technique in the acute stage. Acta Neurochir 145(6): 447-451.
- Kallmes DF, Cloft HJ (2004) The use of hydrocoil for parent artery occlusion. AJNR Am J Neuroradiol 25(8): 1409-1410.
- Kawabata Y, Tsukahara T, Fukuda S, Kawarazaki S, Aoki T, et al. (2016) Successful endovascular treatment of a dissecting aneurysm of vertebral artery associated with double origin of the posterior inferior cerebellar artery. Interv Neuroradiol 22(1): 62-66.
- Kojima A (2015) Vertebral artery dissecting aneurysm treated by internal trapping via the contralateral vertebral artery: A case report. Interv Neuroradiol 21(5): 576-579.
- Kojima A, Okui S, Onozuka S (2010) Long-term follow up of antegrade recanalization of vertebral artery dissecting aneurysm after internal trapping: case report. Neurol Med Chir (Tokyo) 50(10): 910-913.
- Koyama S, Fukuda O, Takaba M, Kameda H, Saitou T (2002) Vertebral artery dissection with subarachnoid hemorrhage after neck pain: A case report. Japanese J Neurosurg 11: 546-550.
- Lenthall RK, White BD, McConachie NS (1999) Endovascular Management of Complete Vertebral Artery Dissection Presenting with Subarachnoid Haemorrhage. Interv Neuroradiol 5(2): 161-166.
- Luo CB, Chang CY, Teng MMH, Chang FC (2005) Endovascular Treatment of Ruptured Vertebral Dissecting Aneurysms with Electrodetachable Coils. J Chinese Med Assoc 68(12): 578-584.
- MacKay CI, Han PP, Albuquerque FC, McDougall CG (2003) Recurrence of a vertebral artery dissecting pseudoaneurysm after successful stent-supported coil embolization: case report. Neurosurgery 53(3): 754-759.
- Mahmood A, Dujovny M, Torche M, Dragovic L, Ausman JI (1991) Microvascular anatomy of foramen caecum medullae oblongatae. J Neurosurg 75(2): 299-304.
- Mehra M, Hurley MC, Gounis MJ, King RM, Shaibani A, et al. (2011) The impact of coil shape design on angiographic occlusion, packing density and coil mass uniformity in aneurysm embolization: an in vitro study. J Neurointerv Surg 3(2) :131-136.
- Mizutani T, Aruga T, Kirino T, Miki Y, Saito I, et al. (1995) Recurrent Subarachnoid Hemorrhage from Untreated Ruptured Vertebrobasilar Dissecting Aneurysms. Neurosurgery 36(5): 905-913.
- Monsivais D, Morales M, Day A, Kim D, Hoh B (2019) Cost analysis of endovascular coiling and surgical clipping for the treatment of ruptured intracranial aneurysms. World Neurosurg 124: e125-e130.
- Oka F, Ishihara H, Kato S, Shinoyama M, Suzuki M (2011) Endovascular treatment of a vertebral artery aneurysm via puncture of the surgically exposed vertebral artery. Interv Neuroradiol 17(1): 74-77.
- Rabinov JD, Hellinger FR, Morris PP, Ogilvy CS, Putman CM (2003) Endovascular management of vertebrobasilar dissecting aneurysms. AJNR Am J Neuroradiol 24(7): 1421-1428.
- Ross IB, Buciuc R (2007) The vascular plug: a new device for parent artery occlusion. AJNR Am J Neuroradiol 28(2): 385-386.
- Sasao R, Katayama M, Inoue S, Suga S (2017) A case of ischemia-onset-type vertebral artery dissection enlarged in a short period and reduced after internal trapping. J Neuroendovascular Ther 11(1): 35-40.
- Satow T, Ishii D, Iihara K, Sakai N, JR-NET Study Group (2014) Endovascular treatment for ruptured vertebral artery dissecting aneurysms: results from Japanese Registry of Neuroendovascular Therapy (JR-NET) 1 and 2. Neurol Med Chir (Tokyo) 54(Suppl 2) : 98-106.
- Sheah K, Lim W, Chan C (2005) Endovascular and surgical management of vertebral artery dissecting aneurysms presenting with subarachnoid haemorrhage: medium-term experience. Ann Acad Med Singapore 34(3): 262-270.
- Sugiu K, Tokunaga K, Watanabe K, Sasahara W, Ono S, et al. (2005) Emergent endovascular treatment of ruptured vertebral artery dissecting aneurysms. Neuroradiology 47(2): 158-164.
- Sugiu K, Tokunaga K, Ono S, Nishida A, Date I (2009) Rebleeding from a vertebral artery dissecting aneurysm after endovascular internal trapping: adverse effect of intrathecal urokinase injection or incomplete occlusion? -case report. Neurol Med Chir (Tokyo) 49(12): 597-600.
- Takahara K, Amano T, Tsurusam Y, Koga N, Murao K, et al. (2017) Ruptured dissecting aneurysm of the fenestrated vertebral artery: A case report. No Shinkei Geka 45(12): 1075-1080.
- Tomura N, Kono K, Okada H, Yoshimura R, Shintani A, et al. (2016) A ruptured vertebral artery dissecting aneurysm involving the anterior spinal artery: A case report. No Shinkei Geka 44(7): 575-581.
- Twitchell S, Abou-Al-Shaar H, Reese J, Karsy M, Eli IM, et al. (2018) Analysis of cerebrovascular aneurysm treatment cost: retrospective cohort comparison of clipping, coiling, and flow diversion. Neurosurg Focus 44(5): E3.
- Uda T, Murata K, Ichinose T, Ikeda H, Kusakabe T, et al. (2006) Endovascular treatment for vertebral artery dissecting aneurysm: effectiveness of internal trapping with proximal flow arrest. No Shinkei Geka 34(10): 1009-1015.
- Yuki I, Murayama Y, Viñuela F (2005) Endovascular management of dissecting vertebrobasilar artery aneurysms in patients presenting with acute subarachnoid hemorrhage. J Neurosurg 103(4): 649-655.
- Zenteno MA, Santos-Franco JA, Freitas-Modenesi JM, Gómez C, Murillo-Bonilla L, et al. (2008) Use of the sole stenting technique for the management of aneurysms in the posterior circulation in a prospective series of 20 patients. J Neurosurg 108(6): 1104-1118.
- Zhang X, Li L, Hong B, Xu Y, Liu Y, et al. (2018) A systematic review and meta-analysis on economic comparison between endovascular coiling versus neurosurgical clipping for ruptured intracranial aneurysms. World Neurosurg 113: 269-275.






























