Surgical Treatment of Brain Metastasis of Axillary Apocrine Cell Carcinoma - Case Report
Luis Cardoso*, Ricardo Nogueira, Lino Fonseca, Pedro Branco, Gonçalo Novais, Miguel Correia and Pedro Roque
Department of Neurosurgery, Centro Hospitalar e Universitário de Lisboa, Portugal
Submission: November 27, 2019; Published: December 10, 2019
*Corresponding author: Luis Cardoso, Department of Neurosurgery, Centro Hospitalar e Universitário de Lisboa Central – Hospital São José, Rua José António Serrano, 1150-199 Lisboa, Portugal
How to cite this article: Luis C, Ricardo N, Lino F, Pedro B, Gonçalo N, et al. Surgical Treatment of Brain Metastasis of Axillary Apocrine Cell Carcinoma - Case Report. Open Access J Neurol Neurosurg. 2019; 12(2): 555835. DOI: 10.19080/OAJNN.2019.12.555835.
Abstract
Apocrine Cell Carcinoma (ACC) is an extremely rare malignant tumor, that manifests by nipple-like plaques or asymptomatic nodules. Are slowly progressive growth lesions, but may be locally aggressive and metastases occur, which affects the prognosis. Due to the rarity of this clinical entity, there are naturally very few reported cases of metastasis, especially in the brain. The authors propose to describe a case of a female patient with ACC brain metastasis at the left parieto-occipital lobe surgically treated. That is the second case in the literature of ACC brain metastasis operated and the first case operated, of ACC brain metastasis that comes from a primary axillary tumor. The authors considered that there was an advantage in the recovery of neurological deficits to allow survival, longer than 1 year.
Keywords: Apocrine cell carcinoma Aggressive Brain Neurological deficits Surgical excision Chemotherapy Immunohistochemical study Cytoplasm, Pleomorphic, Vesicular nucleus Radiosurgery
Introduction
Apocrine Cell Carcinoma (ACC) is an extremely rare malignant tumor that originates at the level of the sweat glands. In more than 50% of cases the primary tumor is located in the axilla, the ceruminous glands of the ear, glands of Moll in the eyelid, scalp, anogenital area, and even the chest, lip, foot, and wrist have been reported sites of occurrence [1]. Clinically, ACCs are manifested by nipple-like plaques or asymptomatic nodules. They are slowly progressive growth lesions but may be locally aggressive and metastases occur particularly in the lungs, liver, brain and bone [2-4]. Although there are relatively few reported cases, most patients with localized ACC undergo wide surgical excision, with margins of 1 to 2 cm whenever possible [1], and in the presence of metastases, the treatment is chemotherapy. The prognosis is better in the absence of lymph node involvement and metastatic forms, and in the presence of metastatic disease patients have a median survival of 14.5 months and a 5 years survival of 10% [1]. Due to the rarity of this clinical entity, there are naturally very few reported cases of metastasis [5], especially in the brain. The authors propose to describe a case of ACC brain metastasis surgically treated.
Case Report
The case reported here refers to a 63-year-old female patient with a low differentiated apocrine cell carcinoma with 4 years of evolution. The patient had a history of smoking and type II diabetes mellitus. Started with a slowly growing axillary nodule, and in the first medical consult was found that she has a skin surface lesion of 4 cm by 4 cm in size, purple-like, without fluctuation or any pain on palpation. Despite being elastic, it had a stiff consistency and apparently was not adhering to the superficial or deep planes of the skin. The patient underwent surgery with total removal of the lesion. Histopathological analysis revealed a low differentiated neoplasia, consisting of a cell population with large and granular eosinophilic cytoplasm, pleomorphic, vesicular nucleus and prominent nucleolus. The tumor had solid pattern, with apparent ducts, signet ring cells and some secreted cells. The immunohistochemical study was positive for GCDFP-15, EMA, CK AE1 / AE3, CK CAM 5.2, CK 7 and CEA-polyclonal. The final histological diagnosis was low differentiated apocrine cell carcinoma (Figure 1).
The patient underwent a systematic study to obtain the staging of the disease. Radiologic examination revealed multiple lesions, namely nodular lesion in the right lung upper lobe of 4.2 cm x 3.3 cm; right hilar adenomegaly 1.5 cm x 1.0 cm; cystic nodule in the right kidney about 6cm in diameter; 2 cm ovoid nodule of greatest diameter at adrenal gland; nodule less than 1 cm in the spleen and; cutaneous lesion in the abdominal wall of 2.1 cm x 1.7 cm. Due to evidence of metastatic disease, she started chemotherapy with epirubicin, cyclophosphamide and 5-Fluorouracil, posteriorly changed to paclitaxel and carboplatin. She maintained follow-up for 4 years, without aggravation of the identified lesions. There was even a reduction in lung (1.9cm x 1.3cm) and kidney (3.9 cm x 3.8 cm) lesions. At this time, she had a 90% Karnofsky Performance Status (KPS) Scale.
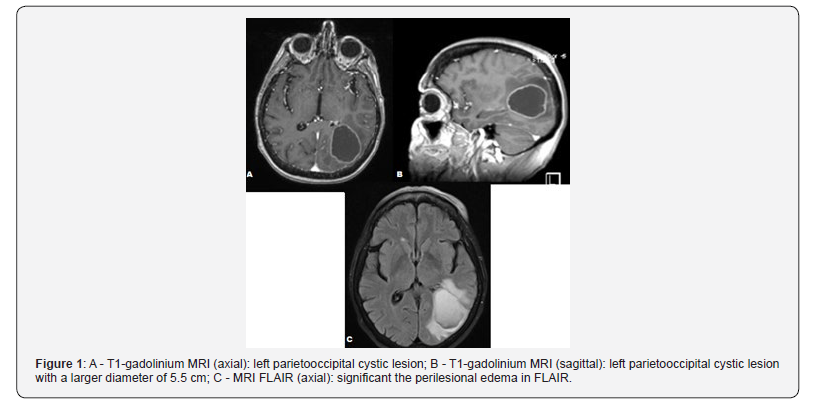
At the 4th year of the disease onset, she began a confusional state, associated with right hemiparesis, with grade 4 muscle strength. She performed the MRI that revealed a huge left parietooccipital cystic lesion with the largest diameter of 5.5 cm, in cortico-subcortical location with deep extension. In T1 weighting with gadolinium, it captured contrast peripherally, being notorious the perilesional edema in FLAIR. multidisciplinary meeting, considering the patient’s previous good condition and the possibility of reversing the focal neurological deficit, it was decided to proceed with the surgery. A left parieto-occipital craniotomy was performed, centered on the lesion, with brain neuron avigation support. After drainage of the cystic content of the lesion, the total microscopic removal of the cyst wall was performed. The surgery and the postoperative period were free of complications, so the patient was discharged without neurological deficits and with a KPS Scale of 90%. Histological analysis of the lesion was compatible with apocrine cell carcinomametastasis. The patient was treated with dexamethasone, with remission of neurological deficits. After a multidisciplinary meeting, considering the patient’s previous good condition and the possibility of reversing the focal neurological deficit, it was decided to proceed with the surgery. A left parieto-occipital craniotomy was performed, centered on the lesion, with brain neuron avigation support. After drainage of the cystic content of the lesion, the total microscopic removal of the cyst wall was performed. The surgery and the postoperative period were free of complications, so the patient was discharged without neurological deficits and with a KPS Scale of 90%. Histological analysis of the lesion was compatible with apocrine cell carcinoma metastasis. The patient was followed up by Oncology, where she kept control of the lesions, and died 15 months after cranial surgery, in the context of the worsening of the disease, with a total of 73 months of disease progression since diagnosis.
Discussion
Apocrine cell carcinomas are very rare entities that usually arise from the sweat glands of axilla. However, some reports illustrate other origin sites in the eyelids, ears, scalp, anogenital region and breasts that usually have indolent clinical courses [6]. From the histopathological point of view, these carcinomas are organized in papillary and tubular structures. Usually these cells are eosinophilic. The diagnosis of apocrine cell carcinoma implies the presence of decapitation images of secretion cells into a cyst, associated with tubular structures or papillary projections [7,8]. Most cases of skin localized ACC are treated by wide surgical excision, with margins of 1 to 2 cm [1]. No effective treatment is currently established for metastatic ACCs and clinical trials remain difficult because of the rarity of this neoplasm [5]. Giventhe lack of controlled studies, the efficacy, the dose and schedule recommendations for adjuvant radiation treatment are lacking [9]. Nevertheless, the longest complete response in a case of nodal and visceral metastasis, which was two years old, was reported with a four-drug regimen using doxorubicin, cyclophosphamide, vincristine, and bleomycin [10]. For patients with primary lesion without evidence of spread, overall median survival is 51.5 months. The lymph node extension and the presence of distant metastases have a huge and bad impact on survival [1]. If the lymph node is involved and there is a metastatic disease, the survival is 33 and 14.5 months, respectively and a 5 years survival is 10% [1]. The authors report the case of a patient with apocrine cell carcinoma brain metastasis of primary origin at the axilla who was surgically treated with brain metastasis removal (Figure 2).

Gallerani et al. [4] describe the case of a patient with primary axilla ACC who, after more than 5 years of development of the disease and had multiple brain metastases. The patient received whole-brain radiotherapy at 30 Gy without any clinical benefit and died a few months later [4]. Shimato et al. [11] reported a patient with multiple brain tumor metastasis originated in the scalp 6 years before. A tumor in the right frontal lobe was successfully operated. However, the small tumor in the right occipital lobe was not cured by Gamma Knife radiosurgery and required second operation. Shimato and his co-authors considered that both operations had contributed to his neurologically independent life for about a year until the patient die for gradual progression of lung metastases [11].
Conclusion
Apocrine cell carcinoma is a rare condition and brain metastases are poorly described in the literature. Due to the lack of published cases and references for treatment, each case is a challenge for the clinical group, particularly in the case of brain metastases. The authors describe the second case in the literature of ACC brain metastasis operated. However, this is the first case operated, of ACC brain metastasis that comes from a primary axillary tumor. Like the first operated patient, the authors considered that there was an advantage in the recovery of neurological deficits to allow survival, longer than 1 year.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Hollowell KL, Agle SC, Zervos EE, Fitzgerald TL (2012) Cutaneous apocrine adenocarcinoma: defining epidemiology, outcomes, and optimal therapy for a rare neoplasm. J Surg Oncol 105(4): 415-419.
- Pai RR, Kini JR, Achar C, Rau A, Kini H (2008) Apocrine (cutaneous) sweat gland carcinoma of axilla with signet ring cells. A diagnostic dilemma on fine-needle aspiration cytology. Diagn Cytopathol 36(10): 739-741.
- Tlemcani K, Levine D, Smith RV, Brandwein-Gensler M, Staffenberg DA, et al. (2010) Metastatic apocrine carcinoma of the scalp: prolonged response to systemic chemotherapy. J Clin Oncol 28: 412-414.
- Gallerani E, Ciriolo M, Rossini C, Cavalli F (2007) Axillary apocrine carcinoma with brain metastases. J Clin Oncol 25(35): 5655-5656.
- Hicham T, Mohammed B, Naoufal H (2018) Primary Cutaneous Apocrine Carcinoma with Distant Metastasis. J Cancer Clin Trials 3:2
- Brichkov I, Daskalakis T, Rankin L (2003) Sweat gland carcinoma. Am Surg 70: 63-66.
- Warkel RL, Helwig EB (1978) Apocrine gland adenoma and adenocarcinoma of the axilla. Arch Dermatol 114(2): 198-203.
- Paties C, Taccagni GL, Papotti M, Valente G, Zangrandi A, et al. (1993) Apocrine carcinoma of the skin. A clinicopathologic, immunocytochemical, and ultrastructural study. Cancer 71(2): 375-381.
- Arden RL (2014) J Cancer Res Ther 2(7): 96-99.
- Mezger J, Remberger K, Schalhorn A, Wohlrab A, Wilmanns W (1986) Treatment of metastatic sweat gland carcinoma by a four-drug combination chemotherapy: response in two cases. Med Oncol Tumor Pharmacother 3(1): 29-34.
- Shimato S, Wakabayashi T, Mizuno M, Norimoto Nakahara, Hisashi Hatano, et al. (2006) Brain metastases from apocrine carcinoma of the scalp: case report. Journal of Neuro-Oncology 77(3): 285-289.






























