Surgical Treatment of Eloquent Area Metastatic Brain Lesions from Unusual Primaries: Early Outcome
Jaggi Ramandeep S1* and Mahawar Vivek2
1 Department of Neurosurgery, Rajiv Gandhi Cancer Institute and Research Centre, India
2Department of Radiology, Rajiv Gandhi Cancer Institute and Research Centre, India
Submission: May 26, 2018; Published: September 10, 2018
*Corresponding author: Jaggi Ramandeep S, Department of Neurosurgery, Surgical Oncology OPD, Rajiv Gandhi Cancer Institute and Research Centre, New Delhi-85, India, Tel: +91-11-47022059; Email: rsjaggi2000@yahoo.com
How to cite this article: Jaggi Ramandeep S, Mahawar Vivek. Surgical Treatment of Eloquent Area Metastatic Brain Lesions from Unusual Primaries: Early Outcome. Open Access J Neurol Neurosurg. 2018; 9(1): 555753. DOI: 10.19080/OAJNN.2018.09.555753.
Abstract
Aim:Brain is one of the commonest sites for metastases in cancer patients and incidence of brain metastases in increasing by the day due to improved survival of cancer patients. Eloquent area Brain metastases may present significant treatment challenges. Very few reports deal with management of eloquent area metastases arising from unusual sources. We present a short series of patients harboring metastatic lesions in eloquent brain region from unusual primary sources.
Methods: During a 2-year period from 2013 to 2015, 10 consecutive patients harboring a cerebral metastasis within the eloquent area of brain from an unusual primary source underwent stereotaxy assisted microsurgical resection. No cortical mapping was used for any of the patients. Eloquent locations included the primary sensorimotor and speech cortices. Unusual source was defined as primary cancer not commonly known to metastasize to brain (all sources except lung, breast, melanoma). All patients were discussed at a multi-disciplinary tumor board. We present the clinical results after operative treatment of metastases within the eloquent brain area, with functional outcome at 3 months.
Results:There were 5 men and 5 women (mean age 47.6 years) who underwent 10 microsurgical operations after stereotactical localization to remove metastatic lesions in eloquent region of brain. There were no perioperative complications. At 3 months follow up, all patients were alive. There was symptomatic improvement or stabilization after neurological improvement in all of the patients. Karnofsky scores improved in all of the patients at 3 months evaluation.
Conclusion: Lot of unusual primary cancers do metastasize to eloquent areas of brain. Complete microsurgical resection of eloquent area metastases from unusual primaries is feasible and beneficial. Patient selection and consequent surgical treatment can lead to significant improvement in the quality of life of such patients.
Keywords: Eloquent; Brain; Metastases; Surgery; Unusual
Introduction
Brain metastasis is a significant cause of morbidity and mortality in cancer patients and its incidence is increasing as a result of advanced imaging techniques and improved survival of cancer patients due to better contemporary treatments available [1]. Moreover, brain metastases are being detected in primary malignancies not usually known to spread to brain [2].
Surgery followed by whole Brain RadioTherapy (WBRT) has been the main modality of treatment for single or limited intracranial metastasis. This is supported by randomized trials and various treatment guideline committees [3-5].
Stereotactic radiosurgery (SRS) has come up and advocated by many as first line treatment for single/multiple metastases or in combination with surgical resection [6]. The ability of SRS to deliver focused radiation to a specified area of brain and theoretical advantage of avoiding risks associated with surgery and deleterious neurocognitive effects of WBRT makes it an attractive choice, especially in lesions located in eloquent region of brain [7]. However, recent studies have highlighted the complications (around 20-40%) such as new neurologic deficits, worsening cerebral edema, persistent seizures and radiation necrosis associated with SRS which negates its projected harmless profile [8].
The treatment of eloquent area metastatic lesions remains a challenge for clinicians [9]. Traditionally, these lesions are approached with caution and less invasive approaches due to the risk of creating new deficits or worsening the existing ones. But as the survival of such cancer patients has increased, it has generated more interest in pursuing aggressive surgical treatment of eloquent area lesion coupled with postoperative radiotherapy, especially with the availability of techniques such as intraoperative imaging, intraoperative tumor visualisation and neuronavigation [10-14].
There is paucity of literature regarding management of eloquent area metastases arising from rare primary malignancies [15]. We present our experience after surgery for 10 consecutive patients harbouring eloquent area metastasis from rare primary malignancies to illustrate the safety and effectiveness of microsurgical resection leading to good early outcome.
Materials and Methods
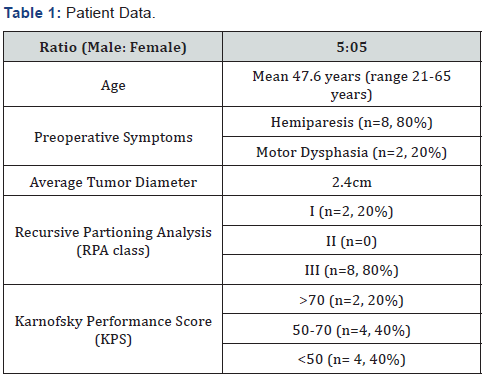
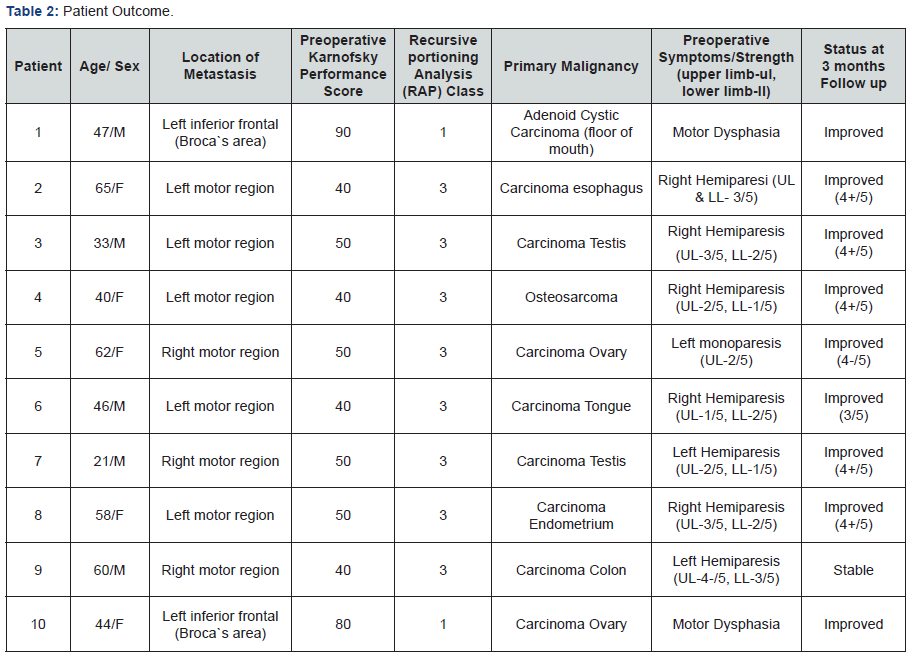
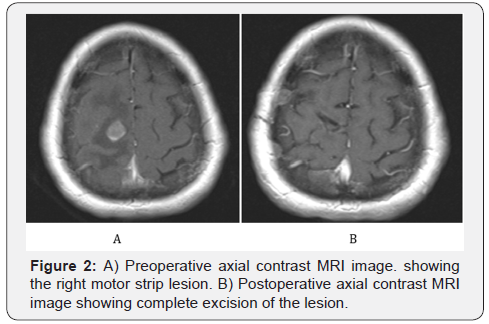
During a 2-year period from 2013 to 2015, 10 consecutive patients harboring a metastatic lesion in the eloquent cortex from an unusual primary source underwent stereotaxy assisted microsurgical resection. Patients with common malignancies metastasizing to brain such as lung, breast, kidney and melanoma were excluded from the study. Prerequisite for neurosurgical treatment was stable systemic disease and life expectancy more than 6 months as discussed with treating oncologist. All patient was discussed in the institutional multidisciplinary board and consensus obtained regarding surgical management. Craniotomy site for surgical resection was decided with frameless or frame based stereotactical localization. Best and safe trajectory for approaching the lesions was decided after studying the different MRI sequences and consultation with the neuroradiologist. No cortical mapping or stimulation was used in any case. All patients were operated by the same surgeon. Preoperative data and patient characteristics with early outcomes are outlined in (Table 1 & 2) respectively. Exemplary preoperative and postoperative brain images are shown in (Figures 1 & 2).

Results
We present outcome at 3 months for this group of patients. There was no surgical complication and hospital stay was uneventful. Gadolinium enhanced brain MRI`s were obtained in all patients on first postoperative day and after 3 months. After surgery, patients were seen at the outpatient department 2-3 weeks after surgery. At 3-months follow up all patients remained alive. Each of the 10 patients received either SRS or WBRT at the discretion of the treating radiation oncologist. Karnofsky Performance Score improved in all patients. Eight out of the 10 patients who presented with a hemiparesis had improved or stable strength at their 3-month follow up visit. The two patients who presented with motor dysphasia also showed complete improvement in speech.
Discussion
Few studies have addressed the issue of treatment of metastatic lesion in the eloquent brain cortex [2,9-12]. It is still an evolving area of cancer care. Very few studies have further reported about treatment of rare brain metastases [15]. Our study focuses on surgical treatment of eloquent region metastases arising from unusual primary malignancies.
Walter et al. [9] showed that 83.3% of patients had improved or unchanged motor deficits after surgery for lesions within the central area. Another series by Weil et al. [10] showed that 94.1% patients who underwent surgical resection of metastases located in eloquent cortex had improved motor strength at a 3-month follow up visit. Kellogg et al [11] also reported improvement in 94% of their patients who were operated for motor area metastatic lesions. Our results also show improvement in 90% of the patients along with stable deficit in the rest, matching the results reported in literature. In majority of the reported series, extensive preoperative functional mapping and intraoperative cortical mapping and stimulation were performed [9,10]. Intraoperative monitoring by motor evoked potential is also not straightforward and can be difficult to interpret. It can vary in sensitivity, specificity, and predictive values when aiming on preservation of motor function and awareness has to be raised among neurosurgeons for these differences when performing surgery in motor eloquent cortex or fiber tracts for these tumor entities because it involves a steep learning curve [12].
We did not use intraoperative cortical stimulation in any of the patient. The same has been supported by Kellogg et al in their study [11]. Nests of tumor cells exist for several millimeters outside the confines of the distinct metastatic brain lesion and its gliotic capsule. Aggressive resection of this microscopic margin, when feasible, can reduce the local recurrence of brain metastases [13]. Therefore, the intraoperative ability to visualize and resect these microscopic margins using fluorescence-guided surgery using 5-aminolevulinic acid (5-ALA) is of considerable interest. In some studies, residual cavity fluorescence was detected in most patients (75%) after gross-total resection of the distinct metastasis. Unfortunately, only one-third of those patients with available histological tissue samples were found to harbor microscopic disease at these 5-ALA-positive margins. Therefore, in non-eloquent areas, the use of 5-ALA seems to drive “supra-maximal” resection of surrounding reactive tissue, which means that caution is required in eloquent areas because 5-ALA positivity was not particularly sensitive for residual micro metastasis. These studies and others demonstrate the pressing need for additional research into novel fluorescent compounds to better define microscopic tumor margins in brain metastases [14]. Majority of studies in the literature have reported on metastatic lesions arising from common primary malignancies. Our study shows that with meticulous preoperative planning and choice of the right operative corridor, excellent results can be achieved in patients harbouring eloquent area metastatic lesions from unusual primary malignancies.
SRS is generally considered as an effective tool for managing eloquent area metastatic brain lesions. However, Williams et al showed in their institution`s comprehensive study that SRS has a significant complication rate of about 40%, more so in the lesions of eloquent cortex [8].
Conclusion
Lot of unusual primary cancers do metastasize to eloquent areas of brain. Complete microsurgical resection of eloquent area metastases from unusual primaries is feasible and beneficial. Careful patient selection and subsequent surgical treatment can lead to significant improvement in the quality of life of such patients.
References
- Minniti G, Clarke E, Lanzetta G, Osti MF, Trasimeni G, et al. (2011) Stereotactic radiosurgery for brain metastases: Analysis of outcome and risk of brain radionecrosis. Radiat Oncol 6: 48.
- Mut M (2012) Surgical treatment of brain metastasis: A review. Clin Neurol Neurosurg 114(1): 1-8.
- Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, et al. (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: A randomised controlled trial. Lancet Oncol 10(11): 1037-1044.
- Kalkanis SN, Kondziolka D, Gaspar LE, Burri SH, Asher AL, et al. (2010) The role of surgical resection in the management of newly diagnosed brain metastases: A systematic review and evidence-based clinical practice guideline. J Neurooncol 96(1): 33-43.
- Patchell RA, Tibbs PA, Regine WF, Dempsey RJ, Mohiuddin M, et al. (1998) Postoperative radiotherapy in the treatment of single metastases to the brain: A randomized trial. JAMA 280(17): 1485-9.
- Dea N, Borduas M, Kenny B, Fortin D, Mathieu D (2010) Safety and efficacy of Gamma Knife surgery for brain metastases in eloquent locations. J Neurosurg 113(Suppl): 79-83.
- Robbins JR, Ryu S, Kalkanis S, Cogan C, Rock J, et al. (2012) Radiosurgery to the surgical cavity as adjuvant therapy for resected brain metastasis. Neurosurgery 71(5): 937-943.
- Williams BJ, Suki D, Fox BD, Pelloski CE, Maldaun MV, et al. (2009) Stereotactic radiosurgery for metastatic brain tumors: A comprehensive review of complications. J Neurosurg 111(3): 439-448.
- Walter J, Kuhn SA, Waschke A, Kalff R, Ewald C (2010) Operative treatment of subcortical metastatic tumours in the central region. J Neurooncol 103(3): 567-573.
- Weil RJ, Lonser RR (2005) Selective excision of metastatic brain tumors originating in the motor cortex with preservation of function. J Clin Oncol 23(6): 1209-1217.
- Kellogg RG, Munoz LF (2013) Selective excision of cerebral metastases from the precentral gyrus. Surg Neurol Int 4: 66.
- Obermueller T, Schaeffner M, Shiban E, Droese D, Negwer C (2015) Intraoperative neuromonitoring for function-guided resection differs for supratentorial motor eloquent gliomas and metastases. BMC Neurol 15: 211.
- Berghoff AS, Rajky O, Winkler F, Bartsch R, Furtner J, et al. (2013) Invasion patterns in brain metastases of solid cancers. Neuro Oncol 15(12):1664-72
- Hardesty DA, Nakaji P (2016) The Current and Future Treatment of Brain Metastases. Front Surg 3: 30.
- Krammer, MJ, Tomasino A, Schul DB, Astner ST, Meier MP, et al. (2011) Modern management of rare brain metastases in adults. J Neurooncol 105(1): 9-25.






























