Evaluation of Haematological Manifestations of Myopia Patients in Nigeria
Emmanuel Ifeanyi Obeagu1*, Getrude Uzoma Obeagu2 and Emmanuel Asuquo Etim3
1Department of University Health Services, Michael Okpara University of Agriculture, Nigeria
2 Department of Nursing Science, Ebonyi State University, Nigeria
3Laboratory Department, Federal Medical Centre, Nigeria
Submission: September 10, 2018; Published: October 09, 2018
*Corresponding author: Obeagu Emmanuel Ifeanyi, Department of University Health Services, Michael Okpara University of Agriculture, Umudike, Abia State, Nigeria.
How to cite this article: Emmanuel I O, Getrude U O, Emmanuel A E. Evaluation of Haematological Manifestations of Myopia Patients in Nigeria. Open Acc Blood Res Trans J. 2018; 2(5): 555598. DOI: 10.19080/OABTJ.2018.02.555598
Abstract
Myopia is a shortsightedness of the eye which is a refractive index abnormality and highly associated to near range of light exposure to the eyes especially those using computers and smart phones. Many persons are coming down with different eye problems both the young and old but myopia is among the most frequently reported cases of the eyes in the hospitals. This research was carried out to ascertain the degree of alterations in some haematological features of subjects with myopia in Nigeria. The research was carried out in a secondary health Care in Umuahia. A total of 180 subjects were chosen for the research. Ninety subjects were myopia patients and ninety subjects were the control. A venous blood sample of 2ml was collected into EDTA container for full blood count (FBC) assay and results analysed using t-test and significance level set at P<0.05. The study revealed significant increase (P<0.05) in ESR, Lymphocyte, monocyte, eosinophil among the myopia patients (13.0± 3.7mm/hr, 38.0±10.2%, 4.0±0.7%, 2.0±0.5%) in relation to the control (6.8±2.1 mm/hr, 34.0±9.4%, 2.4 ±0.3, 1.0±0.2%), pronounced reduction (P<0.05) among the myopia patients in neutrophil, PCV, haemoglobin, red blood cells (56±.08.5%, 35.0± 5.8%, 11.67±0.7g/dl, 3.89±0.2 X1012/L) compared to control (62.0±7.2%, 43.0±8.9%, 14.33±0.5 g/dl, 4.78± 0.5 X 1012/L) and no reduction (p>0.05) in Mean cell volume, Mean cell haemoglobin and Mean cell haemoglobin concentration among the myopia patients (89.97±10.6fl, 30.0±8.4pg, 333.43±20.6g/dl) in relation to the control (89.96±18.3fl, 29.98±10.20pg, 333.26±15.4g/dl). The results indicated reduction in red cell lines and elevation in the total white cell. There was increased ESR may be because of reduction in RBCs, PCV and haemoglobin. The patients with myopia should be monitored especially as it concerns haematological parameters to ensure their well-being. People who are diagnosed with myopia should be requested to include full blood count as part of their routine tests to ensure their health status is in order.
Keywords: Haematological manifestations; Myopia Patients; Nigeria; White blood cells; Neutrophils; Lymphocytes; Haemoglobin
Abbrevations: ESR: Erythrocyte Sedimentation Rate; WBC: White Blood Cells; PCV: Packed Cell Volume; MCV: Mean Cell Volume; MCH: Mean Cell Haemoglobin; MCHC: Mean Cell Haemoglobin Concentration; FBC: Full Blood Count
Introduction
Myopia as shortsightedness is the most common refractive abnormality of the eye and has continued to be more prevalent in the recent times. Though the exact cause may not be known but it is suggested that it has to do with eye fatigue from computer use and other extended near vision tasks coupled with genetic predisposition for myopia. Myopia is reported as a frequent refractive index case disturbing about 100 million persons in the developed world. Its occurrence continues to rise for over past ten years now raising interest in both public and scientific community [1,2]. The occurrence of myopia changes in many parts of the society [3-6]. Myopia is shown to be more dominant in developed nations and places in relation to undeveloped places [7-11].
The fast increase in the prevalence of myopia shows strong sign that present extrinsic factors must have a serious association to the formation of myopia that cannot be explained by a genetic model alone [12,13]. Myopia has been implicated as the sixth leading cause of vision loss [14].
To control myopia, the degree of eye elongation should be reduced. The level of myopia development is more among young subjects who usually become normal around 16 years of age [15]. Both environmental and genetic factors have been associated with the onset and progression of myopia [16].
The phenomenon that myopia spring up from the practice of the eyes during near vision activities was first described Cohn in 1886 and has been connected since to Kepler [17]. The belief in most use and abuse theories is that close sight focusing, such as reading, and computer use is somehow indirectly connected to axial length elongation. The usual belief is the frequent viewing at objects at [18-21] inches leads the focusing system to get stuck at the close reading or computer distance Some researchers have opined that the amount of time spent outside in sunlight is highly linked to the development of myopia than the amount of time spent reading, studying, or working on a computer [22-24].
Optometrists first began using bifocal lenses to attempt to slow myopia progression in the 1940s. The rationale was that if accommodation or focusing caused an increase in myopia, then bifocals or multifocals should lower the accommodative reaction and then reduce myopia development [25].
Aim
This study was done to determine the changes in some haematological features of myopia subjects in Nigeria.
Materials and Method
Study area
The research was carried out at Daughters of Mary Mother of Mercy Hospital, Umuahia, Nigeria.
Subjects
A total of 180 subjects were selected for the study, 90 subjects were myopia patients and 90 subjects were apparently healthy individuals as the control.
Ethical consideration
This research was done in adherence to the guidelines of the Helsinki Declaration on biomedical research on human subjects. The subjects’ vital information was kept confidential.
Statistical analysis
The findings were shown in tables as mean and standard deviation and were analysed using student t-test and the level of significance was set at P<0.05.
Haematological Investigation
The full blood count was done using Mindray BC-5300. The parameters investigated include Erythrocyte Sedimentation Rate (ESR) total white blood cells (WBC), neutrophils, lymphocytes, red blood cells, haemoglobin, packed cell volume (PCV), mean cell volume (MCV), mean cell haemoglobin (MCH) and mean cell haemoglobin concentration (MCHC) (Table 1).
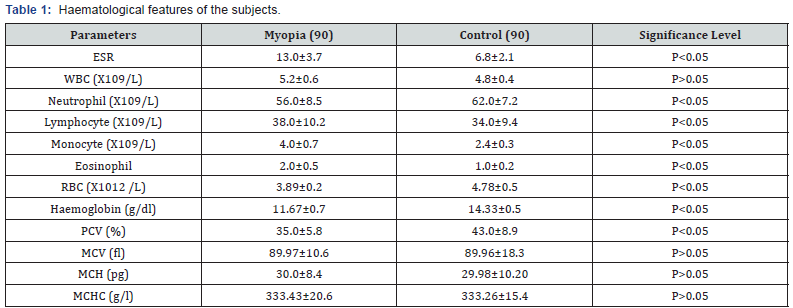
ESR= Erythrocyte Sedimentation Rate,WBC=Total white blood cell, RBC= Red blood cell, PCV= Packed cell volume, MCV= Mean cell volume,
MCH= Mean cell haemoglobin, MCHC= Mean cell haemoglobin concentration
Results
The study indicated significant increase (P<0.05) in ESR, Lymphocyte, monocyte, eosinophil among the myopia patients (13.0± 3.7mm/hr, 38.0±10.2%, 4.0±0.7%, 2.0±0.5%) compared to the control (6.8±2.1 mm/hr, 34.0±9.4%, 2.4 ±0.3, 1.0±0.2%), significant decrease (P<0.05) among the myopia patients in neutrophil, PCV, haemoglobin, red blood cells (56±.08.5%, 35.0± 5.8%, 11.67±0.7g/dl, 3.89±0.2 X1012/L) compared to control (62.0±7.2%, 43.0±8.9%, 14.33±0.5 g/dl, 4.78± 0.5 X 1012/L) and no significant difference (p>0.05) in MCV, MCH and MCHC of the myopia patients (89.97±10.6fl, 30.0±8.4pg, 333.43±20.6g/ dl) compared to the control (89.96±18.3fl, 29.98±10.20pg, 333.26±15.4g/dl).
Discussion
The study was done in myopia patients who have no other recorded and proven disease conditions except myopia and the apparently healthy subjects as the control. The study was done to ascertain the level of changes in haematological parameters associated to myopia. The research indicated elevated ESR among the myopia patients which may be because of increased inflammation, cytokines and raised acute-phase protein with reduced PCV as observed in the myopia patients. All the differential counts were raised except neutrophil that were reduced and no change in the total white cells. This may show increased release of cytokines that may have negative implication on the haematological features. The study showed reduction in red cells, PCV and haemoglobin. This could be that there was suppression in erythropoiesis due to suppression of the bone marrow and may be linked to raise damage of cells. The red cell indices indicated no change. This shows that anaemia in myopia patients is normocytic normochromic as a chronic disease. Haematological parameters have been reported to be a vital indicator of the status of individuals in health and disease [26,27]. It could be used to monitor the progress of disease as well as treatment. The prevalence of myopia continues to rise may be due to exposure to lights such as increase use of computer and smart phones. Smart phones can cause a serious damage to the eye due to the proximity to the eye and especially when used in a poorly lighted environment especially in the nights. Those using computer and smart phones are advised to wear lenses as protective devices to the eyes. The Sight is important to all human being not minding your profession. The study had shown a great alteration in the haematological parameters studied. Those involved in the management of these myopia patients should take note of these haematological changes.
Conclusion
Myopia is shortsightedness which is a refractive abnormality of the eye and has prevalent in recent times may be linked to exposure to computers and smart phones which are placed at a close range to the eyes. The study showed reduction in red cell lines and elevation in the total white cell. There was increased erythrocyte sedimentation rate may be as a result of reduction in red blood cells, packed cell volume and haemoglobin. The patients with myopia should be monitored especially as it concerns haematological parameters to ensure their well-being. People who are diagnosed with myopia should be requested to include full blood count as part of their routine tests to ensure their health status is in order.
References
- Saw SM, Katz J, Schein OD, Chew SJ, Chan TK (1996) Epidemiology of myopia. Epidemiol Rev 18(2): 175-87.
- Matsumura H, Hirai H (1999) Prevalence of myopia and refractive changes in students from 3 to 17 years of age. Surv Ophthalmol 44 (Suppl 1): S109-S115.
- Fotouhi A, Hashemi H, Khabazkhoob M, Mohammad K (2007) The prevalence of refractive errors among schoolchildren in Dezful, Iran. Br J Ophthalmol 91(3): 287-292.
- Rudnicka AR, Owen CG, Nightingale CM, Cook DG, Whincup PH (2010) Ethnic differences in the prevalence of myopia and ocular biometry in 10 and 11 year-old children: the Child Heart and Health Study in England (CHASE). Invest Ophthalmol Vis Sci 51(12): 6270-6276.
- Naidoo KS, Raghunandan A, Mashige KP, Govender P, Holden BA, et al. (2003) Refractive error and visual impairment in African children in South Africa. Invest Ophthalmol Vis Sci 44(9): 3764-3770.
- Saw SM, Goh PP, Cheng A, Shankar A, Tan DT, et al. (2006) Ethnicityspecific prevalences of refractive errors vary in Asian children in neighbouring Malaysia and Singapore. Br J Ophthalmol 90(10): 1230- 1235.
- Uzma N, Kumar BS, Khaja Mohinuddin Salar BM, Zafar MA, Reddy VD (2009) A comparative clinical survey of the prevalence of refractive errors and eye diseases in urban and rural school children. Can J Ophthalmol 44(3): 328-333.
- Saw SM, Hong RZ, Zhang MZ, Fu ZF, Ye M, et al. (2001) Near-work activity and myopia in rural and urban schoolchildren in China. J Pediatr Ophthalmol Strabismus 38(3): 149-155.
- Garner LF, Owens H, Kinnear RF, Frith MJ (1999) Prevalence of myopia in Sherpa and Tibetan children in Nepal. Optom Vis Sci 76(5): 282-285.
- Sapkota YD, Adhikari BN, Pokharel GP, Poudyal BK, Ellwein LB(2008) The prevalence of visual impairment in school children of uppermiddle socioeconomic status in Kathmandu. Ophthalmic Epidemiol 15(1): 17-23.
- Nangia V, Jonas JB, Sinha A, Matin A, Kulkarni M (2010) Refractive error in central India: the Central India Eye and Medical Study. Ophthalmology 117(4): 693-699.
- Smith EL (2011) Prentice Award Lecture 2010. A Case for Peripheral Optical Treatment Strategies for Myopia. Optom Vis Sci 88(9): 1029- 1044.
- Bar Dayan Y, Levin A, Morad Y, Grotto I, Ben-David R, et al. (2005) The changing prevalence of myopia in young adults: a 13-year series of population-based prevalence surveys. Invest Ophthalmol Vis Sci 46(8): 2760-2765.
- Saw SM (2003) A synopsis of the prevalence rates and environmental risk factors for myopia. Clin Exp Optom 86(5): 289-294.
- Tan NW, Saw SM, Lam DS, Cheng HM, Rajan U, et al. (2000) Temporal variations in myopia progression in Singaporean children within an academic year. Optom Vis Sci 77(9): 465-472.
- Curtin BJ (1979) Physiologic vs pathologic myopia: genetics vs environment. Ophthalmology 86(5): 681-691.
- Rosenfield M (1998) Myopia and Nearwork. In: Rosenfield M, Gilmartin B, (Eds.) Boston: Butterworth Heinemann, USA, pp. 91.
- Morgan I, Rose K (2005) How genetic is school myopia? Prog Retin Eye Res 24(1): 1-38.
- Saw SM, Tan SB, Fung D, Chia KS, Koh D, et al. (2004) IQ and the association with myopia in children. Invest Ophthalmol Vis Sci 45(9): 2943-2948.
- Peckham CS, Gardiner PA, Goldstein H (1977) Acquired myopia in 11-year-old children. Br Med J 1(6060): 542-545.
- Xiang F, Morgan IG, He MG (2011) New perspectives on the prevention of myopia. Yan Ke Xue Bao 26(1): 3-8.
- Dirani M, Tong L, Gazzard G, Zhang X, Chia A, et al. (2009) Outdoor activity and myopia in Singapore teenage children. Br J Ophthalmol 93(8): 997-1000.
- Rose KA, Morgan IG, Ip J, Kifley A, Huynh S, et al. (2008) Outdoor activity reduces the prevalence of myopia in children. Ophthalmology 115(8): 1279-1285.
- Zhang M, Li L, Chen L, Lee J, Wu J, et al. (2010) Population density and refractive error among Chinese children. Invest Ophthalmol Vis Sci 51(10): 4969-4976.
- Saw SM, Gazzard G, Au Eong KG, Tan DT (2002) Myopia: attempts to arrest progression. Br J Ophthalmol 86(11): 1306-1311.
- Obeagu EI, Azuonwu O, Didia BC, Obeagu GU, and Onyenweaku F (2017) Determination of Haematological Changes Associated with Syphilis in Subjects in Umudike, Abia State, Nigeria. Cohesive Journal of Microbiology & Infectious Disease. 1(1). CJMI.000505.
- Obeagu EI, Obeagu GU (2017) Evaluation of Some Haematological Features of Tandem Spinal Stenosis Subjects In a Tertiary Hospital in Enugu, South East, Nigeria. Orthopedics and Rheumatology Open Access Journal 9(4): 555758.