Technical Aspects on the Surgical Treatment of Special Tibial Plateau Fractures Types
Reynders-Frederix Peter*1, Reynders Frederix Cristina2, PHAN Dinh Qui Du1 and Illès Tamas1,3,4
1University Hospitals Brussels, campus Brugmann, Belgium
2 University Hospitals Brussels, campus Saint-Pierre, Belgium
3 Odense University Hospital and Institute of Clinical Research, University of Southern Denmark, National Medical Academy, Paris, France
4Odense University Hospital and Institute of Clinical Research, University of Southern Denmark, National Medical Academy, Paris, France
Submission: April 14, 2018; Published: April 26, 2018
*Corresponding author: Reynders Frederix Peter, University Hospitals Brussels, campus Brugmann, Belgium.
How to cite this article: Reynders-F P, Reynders F C, PHAN D Q D,Illès T. Technical Aspects on the Surgical Treatment of Special Tibial Plateau Fractures Types. Nov Tech Arthritis Bone Res. 2018; 2(5) : 555597. DOI: 10.19080/NTAB.2018.02.555597
Introduction
Complex Bicondylar Tibial Plateau Fractures
Bicondylar fractures are often classified as belonging to the Schatzker8 V group. Since the work of Luo CF in 2010 6 we know that we have to pay more attention to the posterior column fractures of the tibial plateau. Intimate reduction of the medial and lateral column is not feasible without first reducing the posterior column. Posterior buttress plating via posterior approach is mandatory. In this approach the patient is put in a prone position with the knee slightly bend . After prepping and draping the lower limb, a sterile disposable tourniquet, Hemaclear (OHK ,Sderot HaPalyam,Haifa Israel) is used to control the venous and arterial bleeding. These sterile tourniquets are small in width, enlarging the surgical field Figure 1.

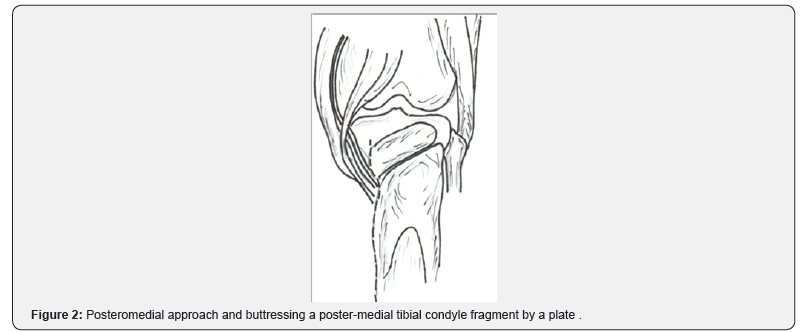
A large postero-medial incision with detachment of the medial border of the soleus and popliteus muscles will bring you to the posterior surface of the medial and lateral tibial condyle [1]. This is an extensile approach giving the surgeon a wide and comfortable exposure to the posterior aspect of the proximal tibia. In these difficult cases one should avoid the so called minimal invasive approaches. In contrast with the postero-lateral approach the posterior approach with medial extension, the muscle layer of the popliteus and triceps surae with neurovascular bundle is lifted and brought aside in one block. Sometimes one needs to clamp the terminal branches of the medial inferior genicular artery Figure 2. The pure postero-lateral approach, entering lateral from the neurovascular bundle is possible but rather cumbersome in avoiding the anterior tibial artery and the posterior recurrent arteries Figure 3. Be careful with the lateral placement of Homann retractors, they can violate the anterior tibial artery and its recurrent tributaries. Placement of two Muller’s distractors can be of great help. In using the Muller distractors one should avoid using only one distractor. Laterally placed they tend to put the knee in a varus position Figure 4. Often is the reduction by a buttress plate the easiest way. In young persons a normal prebend DCP plate with standard cortical screws is helpful. In case of osteopenic bone, LCP technology is mandatory [2]. The plate is secured distally, pushing the console of the fracture to a more proximal and reduced position Figure 2. There is no need for proximal screw placement. One plate at the postero-medial corner and another at the postero-lateral corner will keep the whole posterior column in an upright position.


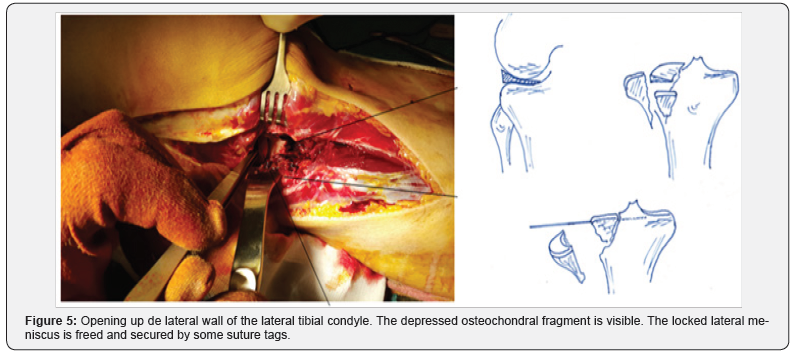
After hemostasis and wound closure , the plate is covered with a lyophilized collagen fleece impregnated with 2 gram of gentamycine sulphate per cm 2 Duracoll ( Eusa Pharma Antwerp Belgium) and 1 gram of vancomycin powder. The patient is turned in the supine position. Same prepping and draping technique and use of a sterile tourniquet [3]. An anterolateral approach is used, large enough for allowing plating to the lateral tibial condyle. The arthrotomy is done anteriorly , which is easier to detach the menisco-capsular junction . The intraarticular view is much better than the pure lateral submeniscal arthrotomy. After rinsing out the knee joint of blood clots, the lateral bone ridge is opened Figure 5.
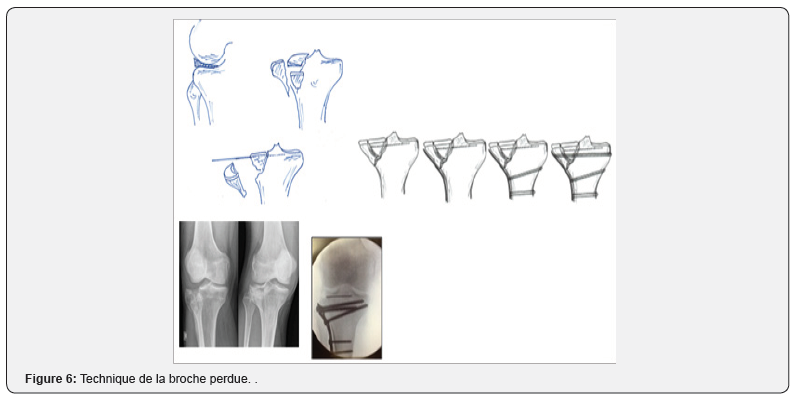
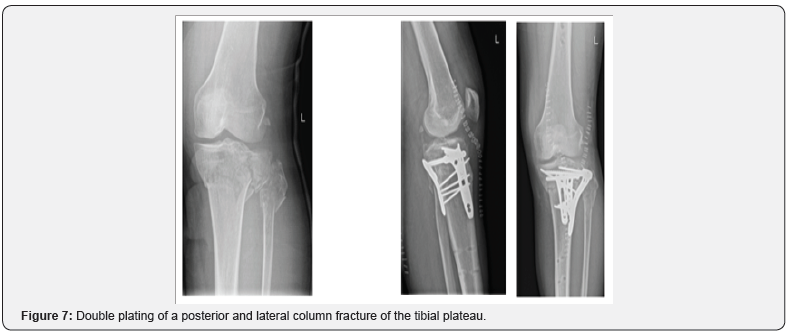
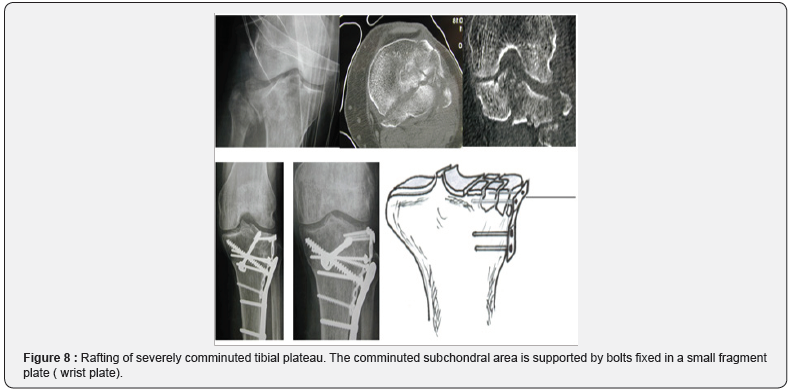
The locked lateral meniscus is freed and secured with some suture tags. The intermediate fragment is anatomical reduced and fixed with two smooth 1.6 mm Kirschner wires and cut off flush at the bone edge. The lateral wall is closed and secured with compression screws. These screws needs to be protected with a buttress plate. This technique calls the “Technique de la broche perdue” Figure 6. In the presented clinical case, the radiographs show the posterior buttressing with anatomical shaped plates.(Dupuy-Synthes Zaventem Belgium) Figure 7. In rare extreme comminution the technique of rafting with a small fragment plate and bolts which holds into the plate can be a solution, Figure 8. After image intensifier control, local antibiotics are used; Vancomycin powder 1 gram and Gentamycin resorbable fleece 40 mg. Hemostasis and wound closure. Even disrupted, the meniscus can heal in these trauma cases, as a consequence the torn meniscus should be retained at all cost.
Set Up In Theatre
a) Patient is in de the prone position on a radiolucent operating table. Inform your anaesthesiologist clearly about this prone position and the need for changing to the supine position during surgery.
b) Free access of the image intensifier is mandatory
c) Patient is prepped and draped in the usual way.
Instruments Needed
a) Battery driven power system.
b) 3.5 and 4.5 mm fragment set with reduction forceps.
c) Set of regular small fragment plates and in osteoporotic cases LCP material.
d) Big and small lamina spreader. Muller distractor, if possible two.
e) Lyophilized collagen implant impregnated with the amino glycoside antibiotic gentamicin fleece.
Postoperative Regime
Immediate active mobilization. Non-weight bearing for two months and touch weight bearing for an additional month with knee brace.
Percutaneous Stabilization of Type III Schatzker Fracture
Type III fractures according to Schatzker represents a central depression of the tibial plateau, often lateral tibial condyle. It happens more with an older group of patients. It’s typically a low energy trauma on a weaker bone [4]. When valgus instability is found , reduction and internal fixation is worthwhile. Depending also on patient expectation , biological age and medical comorbidities. Typically a lateral based bone window is created afterwards a bone punch is needed to elevate the depressed fragment. This manoeuver often results in an additional fracture of the lateral tibial wall Figure 9.

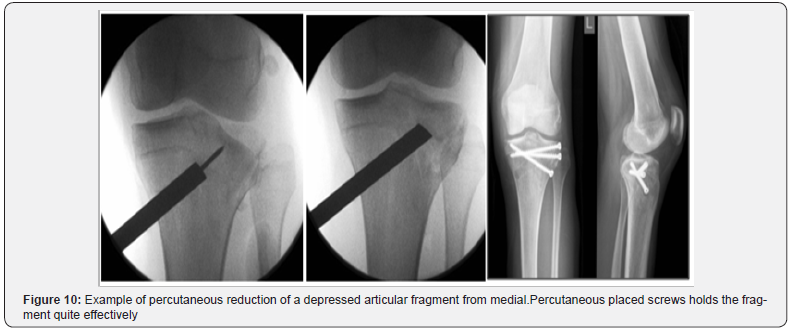
In these cases an additional instability is created necessitating a more complex surgery with buttress plating. These fractures, which happens often in our aging population, can be treated simple and effectively by a lateral directed , cannulated beveled bone punch ( diameter 10 mm). This bone pusher enters from a medially created bone window Figure 10. A Kirchner wire is advanced just under the depressed articular area. Care is taken not to enter into the joint. A tip apex distance of at 2 cm is needed. The medial cortex is perforated with a cannulated drill (8mm) [5]. Care is taken not to advance the cannulated drill into the cancellous bone of the metaphysis. With the bone punch a swiping movement is done to scrape enough cancellous bone. This creates a bone wall, which is progressed towards the depressed fragment . This wave of bone will push the depressed articular fragment on its place without violating the lateral wall of the tibial condyle. To monitor the progression of the bone lifting, fluoroscopy in two planes is mandatory. Important detail is given to the gently pushing of the bone in its place. If the lifting of bone goes too fast, the articular fragment splits with a risk of ending with the bone punch into the joint.
Special care is taken to reduce the most anterior part of the depressed articular fragment. After reduction, percutaneous placed 7.3 mm screws in a triangulated construct is needed to contain the reduction. The screws are orientated from lateral to medial, depending on the exact location of the depressed area. The intact lateral bone wall act as a biological plate where the screws are anchored on. This construction has the same strength as a classically buttress plate and screws. Elevating the depressed fragment under arthroscopic control can be useful to monitor also the position of the torn lateral meniscus. If the meniscal fragment is not incarcerated into the depressed bone fragment, no further action is needed and spontaneous healing of the ruptured meniscus is often seen [6].
In every circumstances a lengthy arthroscopic procedure needs to be avoided for risk of massive leakage of arthroscopic fluid into the lower limb. This swelling of the lower limb can be responsible only to a transient ischemic insult. In some rare cases with extensive squashing of the lateral articular area, a fibular strut graft can be used [7]. The beveled strut graft can be orientated (rotated) in such way as to give maximal support to buttress the articular fragment Figure 11. In this case the massive fibular strut graft needs to be secured at its base by a medio-lateral placed screw to prevent the backing out of the strut.

Preoperative Planning
Plain radiographs and CT scanning Figure 9 is essential for exact location of the depressed articular fragment. Although 3D reconstruction images are interesting, it’s not really mandatory in your preoperative planning. Clinical examination and anamnesis is very helpful to detect an instability and to have an idea about the energy absorbed during the incident.
Set Up in Theatre
a) Patient is in de the supine position on a radiolucent operating table with the image intensifier positioned obliquely on the lateral site of the patient Figures 1 & 2
b) It’s essentially a percutaneously executed operation, so an inflated tourniquet is not necessary.
c) For security reasons a deflated tourniquet is put on.
d) Patient is prepped and draped in the usual way [8].
Instruments Needed Figure 11
a) Battery driven power system.
b) Set of bone punches.
c) Set of cannulated 7.3 mm screws.
d) Hammer.
e) Kirchner wires 1.6 mm.
Postoperative Regime
Immediate active mobilization. Non-weight bearing for two to four months depending on the amount and severity of the depressed articular fragment . The use of an additional hinged knee brace is mandatory.
References
- Schatzker J, McBroom R, Bruce D (1979) The tibial plateau fracture: The Toronto experience 1968-1975. Clin Orthop Relat Res 138: 94- 104.
- Rockwood CA, Green DP, Bucholz RW, Court Brown CM, Tornetta P, et al. (2010) Rockwood & Green’s fractures in adults. Lippincott Williams & Wilkins 1: 53-85.
- Mallina R, Kanakaris NK, Giannoudis PV (2010) Peri-articular fractures of the knee: an update on current issues. Knee 17(3): 181-186.
- N Ahearn Oppy A, Halliday R, Rowett Harris J, Morris SA (2014) The outcome following fixation of bicondylar tibial plateau fractures. Bone Joint J 96(7): 956-962
- Matthias Krause, Preiss A, Müller G, Madert J, Fehske K (2016) Intraarticular tibial plateau fracture characteristics according to the “Ten segment classification”. Injury Int J Care Injured 47(11): 2551-2557
- Zhang W, Luo CF, Putnis S, Sun H, Zeng ZM, et al. (2012) Biomechanical analysis of four different fixations for the posterolateral shearing tibial plateau fracture. Knee 19(2): 94-98.
- Egol KA, Su E, Tejwani NC, Sims SH, Kummer FJ, et al. (2004) Treatment of complex tibial plateau fractures using the less invasive stabilization system plate: clinical experience and a laboratory comparison with double plating. J Trauma 57(2): 340-346.
- Joseph Schatzker, Marvin Tile (1987) The rationale of Operative Fracture Care. Springer Verlag.






























