Abstract
This study aimed to examine the effectiveness of eight-week mindful yoga on improving psychosocial outcomes and lowering cortisol levels among cancer patients in Hong Kong. We recruited 15 cancer patients from one local oncology center via stratified sampling, and simple random sampling via online platforms. Psychosocial outcomes including health-related quality of life, perceived stress, mindfulness, and depression were assessed using validated scales before and after the eight-week mindful yoga program which was led by a certified mindful yoga teacher. Participants collected saliva samples using Salivettes four times per day on two consecutive days before and after yoga training, respectively. Analyses using paired t-tests showed that health-related quality of life t (14) = 4.81, p < 0.005, was improved and perceived stress was reduced t (14) =-3.85, p < 0.005, by mindful yoga. Results generated by a 3-way mixed ANOVA with repeated measures (Day and Intervention) and Age (a between-subject factor) showed that the mean cortisol level was lowered by the yoga program, F (1, 12) = 23.96, p < 0.001. There was also a significant Age by Intervention interaction in that the cortisol-lowering effect of mindful yoga was accentuated in older participants, F (1, 12) = 4.93, p = .046. This pilot study demonstrated a significant effect of an eight- week Mindful Yoga course in improving quality of life and reducing perceived stress in cancer patients. Cortisol levels were lowered by the intervention with a stronger effect in older participants. To establish causal relationship reliably, larger-scale randomized controlled trials are indispensable.
Keywords: Mindfulness; Depression; Perceived Stress; Quality of Life; Mindful Yoga; Cancer
Abbreviations: MBIs: Mindfulness-Based Interventions; MBSR: Mindfulness-Based Stress Reduction; MBCT: Mindfulness-based Cognitive Behavioural Therapy; RCTs: randomized controlled trials; IRB: Institutional Review Board; PMH: Princess Margaret Hospital; HRQoL: Health-related Quality of Life; PSS: Perceived Stress Scale; FFMQ-C: Five Facet Mindfulness Questionnaire; PHQ: Patient Health Questionnaire; CPSS: Perceived Stress
Introduction
Mindfulness-Based Interventions (MBIs)
Originating from Buddhism, Kabat-Zinn has defined mindfulness as the awareness arising from paying non-judgmental attention to the present moment [1]. As an evidence-based intervention, MBIs have been shown effective in improving attention focus, discomfort tolerance, cognitive alteration, and stress coping, via relaxation and acceptance [2]. Mindfulness-Based Stress Reduction (MBSR) and Mindfulness-based Cognitive Behavioral Therapy (MBCT) are two major approaches of mindfulness-based interventions. Both of them have demonstrated various clinical and non-clinical significance in different client groups and fostering non-judgmental acceptance of experiences [3,4]. The mental health benefits of both MBSR and MBCT have been verified in recent meta-analytic reviews (MBSR [5]; MBCT [6]).
Mindful (Mindfulness-based) Yoga
MBSR is run in the form of a structured program with a standardized curriculum typically lasting for 8 to 10 weeks in groups of 10 to 40 [5]. It aims to cultivate “mindfulness” progressively in participants with a combination of methods including mediation and yoga. Although yoga is an important component in MBSR through which mindfulness is cultivated, mindful or mindfulness- based yoga is a different approach in which mindfulness is cultivated primarily through the practice of yoga asana, pranayama and meditation with less reliance on mindfulness education sessions [7,8]. In this regard, it is increasing difficult for researchers to differentiate between conventional mindfulness interventions and yoga while attempts to integrate yoga with mindfulness education or teaching is increasing. In addition, a number of recent attempts comparing the mental health effects of yoga with a physical orientation with mindfulness training have found that yoga is as effective as mindfulness training in enhancing mental health outcomes [9].
In a similar vein, another randomized controlled trial with employees suffering from burnout has found that Ashtanga yoga and MBCT, were slightly more effective in improving healthrelated quality of life than CBT, with no difference between yoga and MBCT [10]. Despite evidence showing equal effectiveness of yoga and conventional mindfulness interventions, a recent metaanalysis points to increased effectiveness of yoga in improving physiological parameters of health such as diurnal cortisol levels, systolic blood pressure, resting heart rate, and inflammatory measures, among others, in comparison to MBSR [11]. It has been shown that the effect of yoga training on improved quality of life was mediated by enhanced mindfulness, the same mechanisms mediating the benefits of conventional mindfulness interventions [12]. Taken together, the reviewed evidence suggests that yoga with an emphasis on mindfulness (mindful yoga hereafter) could be a promising alternative to the highly structured group-based MBSR because of its standalone nature and the readiness to be incorporated into people’s daily routines. This is one of the major factors that motivated conduction of the present study to examine the effect of a mindful yoga program on cortisol and psychological outcomes in Chinese cancer patients receiving treatments in a major hospital in Hong Kong.
The Present Study
The psychological and biobehavioral effects of yoga have been extensively reviewed. A meta- analysis comprised of 42 studies has revealed a significant medium effect of yoga on reducing depression and anxiety among cancer populations. Regardless of the type of tumor, control group, treatment regime, and yoga implementation logistics, yoga helped improve depression and anxiety among cancer patients [13]. In a similar vein, another meta-analytic review with 26 RCTs on breast cancer patients has shown that yoga intervention significantly reduced depression, anxiety, stress, fatigue and pain, and improved mental and physical wellbeing, and sleep quality [14]. The psychosocial effects of yoga are similar to that reported in another meta- analysis looking at the effect of MBSR in breast cancer patients in 19 RCTs [15]. Recent reviews or meta-analyses have been showing that yoga effectively reduces diurnal cortisol levels and thus benefits symptom management in oncological populations and improves prognosis [10].
An elevated level of cortisol has been suggested to be a key factor in exacerbating the progression of cancer via its inhibitory effect on apoptosis and defense against oxidative stress [16]. On the other hand, the biobehavioral benefits of yoga were also demonstrated in thirty-nine randomized controlled trials (RCTs) with healthy youth [17]. Despite variations in training duration and number of sessions, yoga demonstrated positive effects in at least one of the three domains, namely physiological/physical, psychological/behavioral, and cognitive functioning in thirtyfour studies. This points clearly to the effectiveness of yoga in improving psychological functioning in young and healthy populations. In addition to the psychosocial and biological benefits of yoga reported in recent reviews, mindful yoga has also demonstrated its potential to be an adjunct therapy for cancer because of, as mentioned earlier, its standalone nature and readiness to be incorporated into patients’ daily life. Keeping this in mind, we designed the present study to examine the effect of an eight-week mindful yoga program on salivary cortisol levels and major psychological outcomes in Chinese cancer patients recruited through a major hospital in Hong Kong.
Method
The study was conducted in full conformance with the Declaration of Helsinki, and granted approval by the Institutional Review Board (IRB) of the Hospital Authority (Ref: KW/EX-23- 06 187-06) and the Research Committee of the City University of Hong Kong. In addition, the study was also designed and conducted in compliance with the STROBE guidelines.
Participants
A total of 29 participants were recruited from the Oncology Department of Princess Margaret Hospital (PMH) via stratified sampling, and simple random sampling via online platform. Cancer patients with different diagnoses were invited to take part in the study voluntarily without any financial inducement. To be eligible to participate in the study, participants must meet the following inclusion criteria:
1) Hong Kong residents who are at least 18 years old
2) Being literate in Cantonese and written Chinese
3) Having completed the surgical operation and scheduled
chemotherapy
4) Physically and mentally fit for practicing mindful yoga
with mild physical intensity
5) Have not attended more than 5 yoga lessons before.
Patients would be considered as not suitable for the study if they met one of following exclusion criteria:
1) Having undergone mindfulness training.
2) Having undergone psychotherapy such as CBT.
3) Mentally and/or cognitively and/or emotionally
impaired.
4) Having damages to the hypothalamic-pituitary-adrenal
axis.
5) Currently on oral contraceptives that may or may not
affect the risk of cancer.
6) Having significant physical symptoms, such as but
not limited to bone metastasis, spinal cord compression, brain
metastasis, cardiovascular failure, renal failure, and late-stage
cancer. Nineteen participants meeting the inclusion and exclusion
criteria (IEC) were contacted by the research team for enrollment
via phone call/ text messages.
Procedure
Eligible participants were invited to attend a briefing session
in which the main objectives and procedure of the study were
explained to them, and informed consent was collected. Detailed
instructions concerning the collection of saliva samples using the
Salivettes (Sarstedt, Nümbrecht) in a self-administered way were
provided. Participants were also given a link to a Google Form for
recording the saliva sampling times which were scheduled at
• immediately upon waking,
• 30 mins. after waking,
• 3 hours after waking, and
• before bedtime, on two consecutive days before and
after the 8-week mindful yoga program.
They were also instructed to refrain from exercise, smoking, brushing teeth, eating, and drinking beverages that contain alcohol or caffeine before collection of the first two saliva samples and for 1 hour before collecting the remaining two samples during a day. Participants were given sufficient time to make a decision to take part in the study or not, and encouraged to ask any questions about, and raise any concerns with, the study before the briefing session concluded.
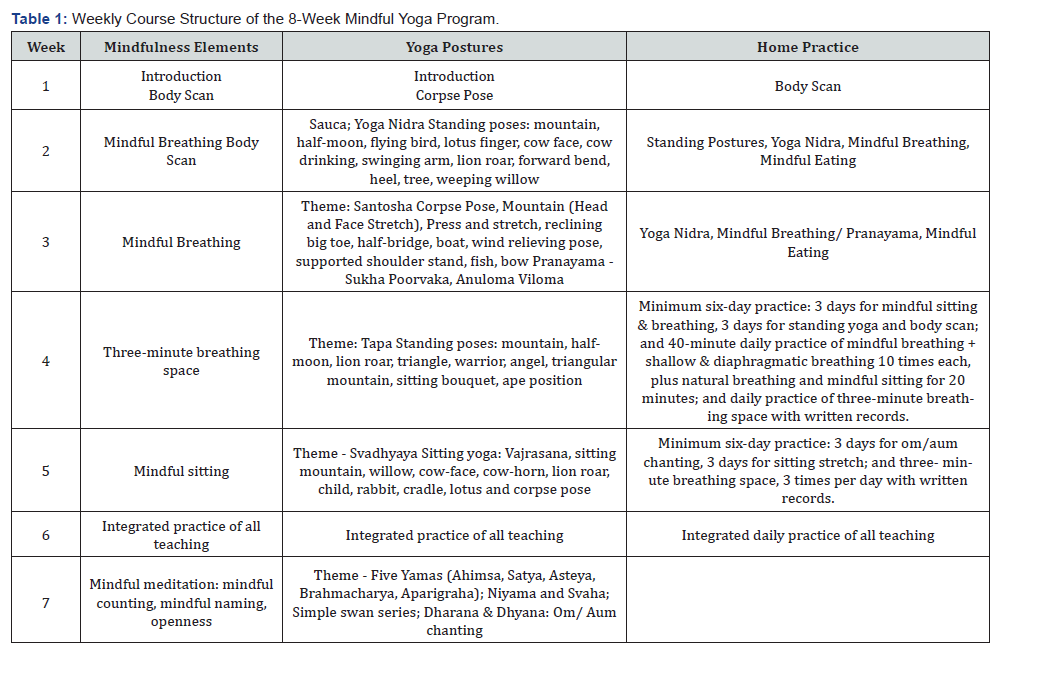
Mindful Yoga
Participants met in the same yoga studio 2.5 hours per week over 8 weeks between March and April in 2024 for their yoga lessons. All sessions were led by a certified yoga teacher with experience in teaching yoga to cancer patients. The focus of the program was on the integration of mindfulness elements of MBSR with yoga postures, breathing and meditation. Participants were encouraged to practice at home daily following the home practice videos provided by the researchers. Details of the weekly course structure of the mindful yoga program can be found in (Table 1).
Measures
Participants were required to complete an online survey within 3 days before the commencement, and within one week after the end, of the mindful yoga program. The survey was designed to measure psychological outcomes including health-related quality of life, perceived stress, mindfulness, and depressive symptomatology. Health-related Quality of Life (HRQoL) was measured by the Chinese version of the Health Survey Short Form-12 (SF-12 v2) [18]. This brief scale measures 8 health domains subsumed under the Physical (physical functioning, role-physical, bodily pain, and general health) and Mental (vitality, social functioning, role-emotional, mental health) component, respectively. This measure has been used to assess the benefits of mindfulness training on cortisol response in breast cancer survivors [19]. The scale exhibited acceptable internal consistency at pre- and post-intervention, with Cronbach alphas equal to 0.86 and 0.87, respectively.
Perceived Stress was measured by the Chinese version of the 10-item Perceived Stress Scale (PSS-10) validated in Hong Kong Chinese [20]. The scale has been widely adopted by previous studies as a reliable tool to assess the influence of mindfulnessbased interventions (MBIs) on perceived stress in patients with various cancer, including breast cancer survivors, gastrointestinal and lung cancer patients [21-24]. The scale exhibited acceptable internal consistency in the present sample with Cronbach alphas equal to 0.89 and 0.83 in pre- and post-intervention, respectively.
Mindfulness was measured by the Chinese version of Five Facet Mindfulness Questionnaire. Chinese Five Facet Mindfulness Questionnaire (FFMQ-C) assesses five major aspects of mindfulness, namely observation, description, aware action, nonjudgmental experience to inner experience, and non-reactivity to inner experience. The scale consists of 39 items anchoring to a 5-point scale. The scale demonstrated acceptable internal consistency with Cronbach alphas equal to 0.84 and 0.89 in preand post-intervention, respectively. The FFMQ-C has been shown to be a reliable and valid measure of mindfulness in a recent study with Chinese colorectal cancer survivors on quality of life and sleep patterns [25]. Depression was measured with the Chinese version of the 9-item Patient Health Questionnaire (PHQ-9), which has been validated in studies with Hong Kong [26] and mainland Chinese [27]. Respondents were asked to indicate the frequency of experiencing each of the 9 items in the last two weeks using a 4-point scale (0 = not at all; 3 = almost every day). Acceptable levels of internal consistency of the scale were observed in the present sample, with Cronbach alphas equal to 0.90 and 0.78 in pre- and post-intervention, respectively.
Collection of Saliva Samples
Participants were asked to collect 4 saliva samples at immediately after waking, and 30 mins. and 3 hours thereafter, and before bedtime each day over two consecutive days. Saliva samples were collected within 3 days prior to the commencement of the intervention, and within 7 days after the end of the intervention. Participants were required to store the saliva samples in the freezer compartment of their home refrigerators until they returned the samples to the researcher within one week. In addition, they also filled out an online diary to indicate the time at which each saliva sample was collected. The saliva samples were stored in the laboratory at -20o Celsius until they were thawed for cortisol assays.
Statistical Analyses
The focus of analyses was on the changes in salivary cortisol and the four psychological outcomes. This was examined with paired t-tests. As cortisol data were skewed to the right with a number of outliers, the cortisol data were winsorized at 2 SDs and then log10 transformed, which significantly reduced skewness of the data.
Results
Sample Characteristics
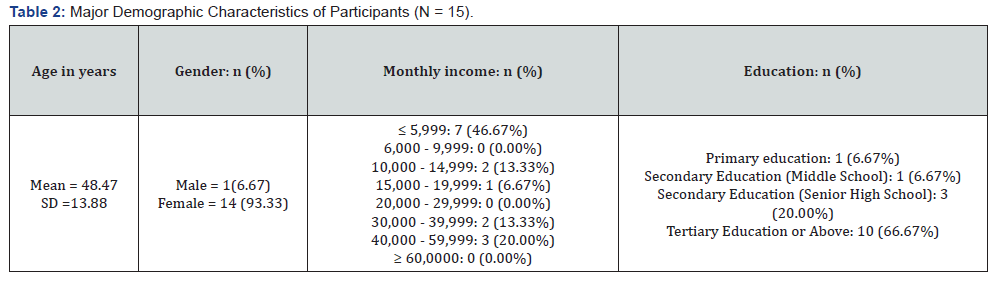
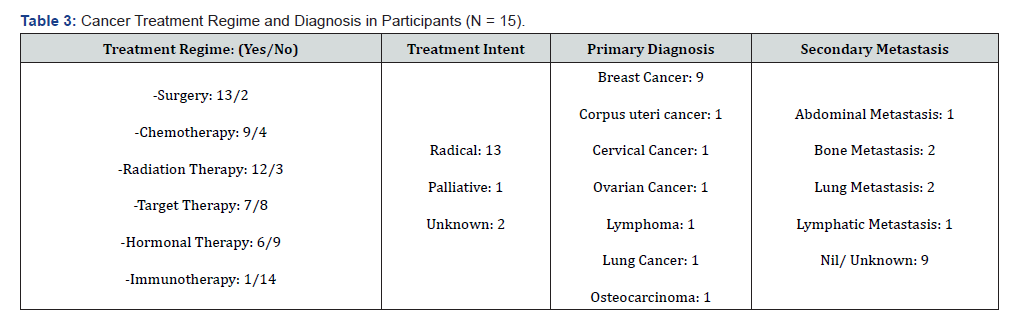
Major demographic characteristics and clinical profiles of the participants are summarized in (Table 2 & 3). The majority of the participants (N = 15) was women (n = 14), with only one male participant (n = 1), having a mean age of 48.47 yrs. (SD = 13.88). They were in general highly educated with the majority having received tertiary or higher education (n = 10). In terms of clinical profiles, most participants exhibited a radical treatment intent (n = 13), and have gone through chemotherapy (n = 9) and/or radiation therapy (n = 12).
Changes in Psychological Outcomes and Salivary Cortisol
Saliva samples were thawed and centrifuged at 3500 rpm for 2 min at room temperature; clear supernatants were used for analysis. Cortisol was assayed using the Abcam (ab154996) cortisol in vitro competitive ELISA kit, with sensitivity of 0.12 ng/ ml (0.33nmol/L). The means and standard deviations of healthrelated quality of life (HRQoL, SF-12), perceived stress (CPSS-10), depression (PHQ-9), mindfulness (FFMQ-C), and mean diurnal cortisol levels (average of the concentrations of cortisol in the 4 saliva samples over the day), are summarized in (Table 4). Results of paired-sample t-tests show that mindful yoga significantly increased HRQoL or SF-12 scores, with significant effect in the mental component, t (14) = 4.54, p < .001. Perceived stress was also significantly reduced, t (14) = - 3.85, p < .001. In addition, a trend in enhanced mindfulness, t (14) = 1.88, p = .08, and reduced depression, t (14) = -1.84, p = .09 was also observed.
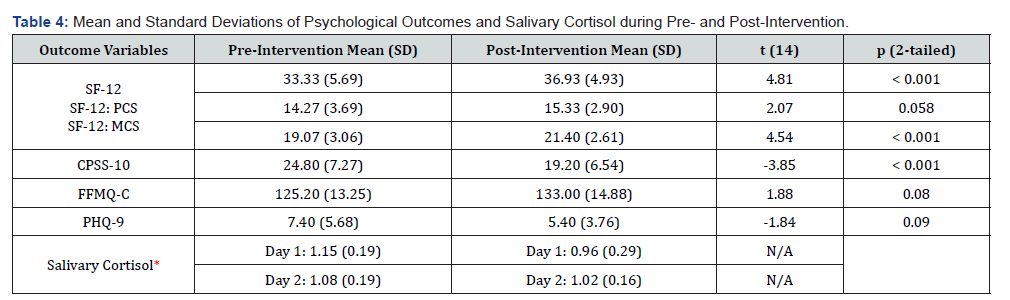
*, log10 nmol/L (mean diurnal level); SF-12 = Health Survey Short Form-12; SF-12: PCS = Physical Component Summary; SF-12: MCS = SF-12 Mental Component Summary; CPSS-10 = 10-item Chinese Perceived Stress Scale; FFMQ-C = Chinese Five-Facet Mindfulness Questionnaire; PHQ-9 = 9-item Patient Health Questionnaire.
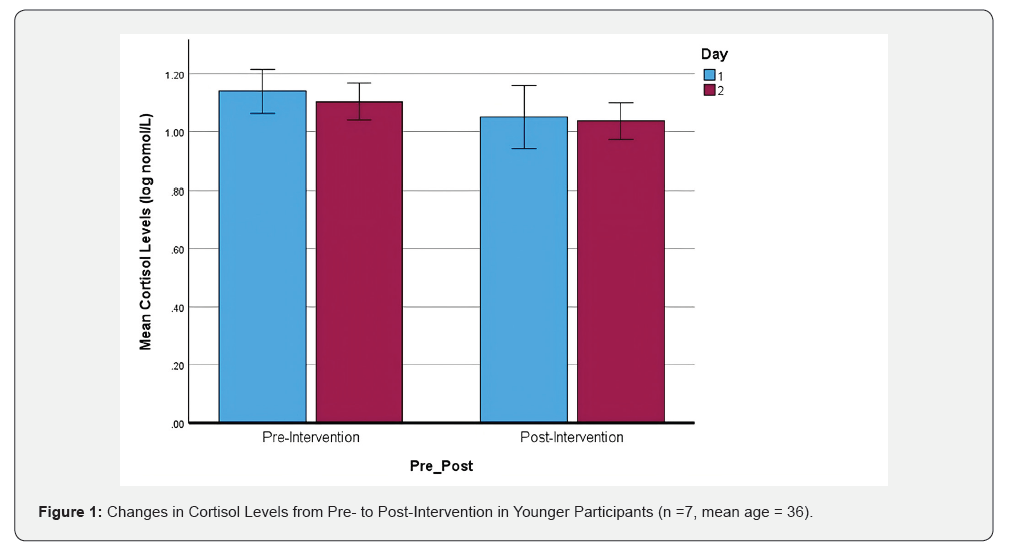
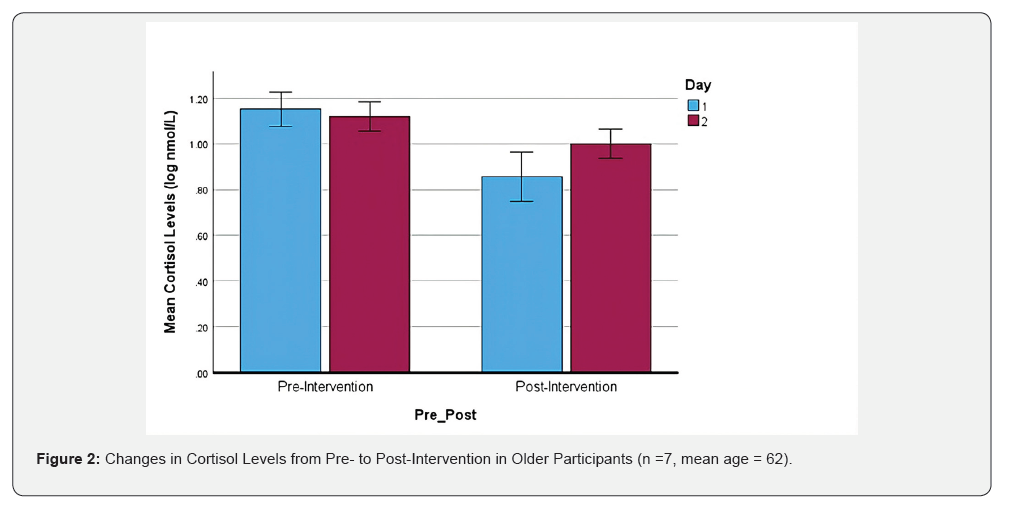
With regard to changes in diurnal cortisol levels, initial inspection of the correlations between mean levels of cortisol were correlated with age of participants in pre- and post-intervention in an opposite way. Age was correlated positively with mean cortisol in pre-intervention (r = .183), but negatively in post-intervention (r = -.250). Although the two correlations are not significant, this pattern suggests possible interaction between age and change in cortisol levels from pre- to post-intervention. A 3-way mixed ANOVA with repeated measures (day and pre- post intervention) and age (a between-subject factor creating by a split at the median age of 44 yrs.). This created a younger group (n = 7) with mean age = 36.00 yrs., SD = 5.23, and an older group with mean age = 61.57 yrs., SD = 6.08. Results of ANOVA show that diurnal cortisol levels were lowered significantly by mindful yoga, F (1,12) = 23.96, p < .001. There was also a significant interaction between age and pre- post intervention, F (1,12) = 4.93, p = .046, such that the cortisol-lowering effect of mindful yoga was stronger in older participants. This pattern of interaction is illustrated graphically in (Figure 1 & 2).
Conclusion and Discussion
Present findings show that an eight-week mindful yoga program significantly improved health-related quality of life (HRQoL) and reduced perceived stress in cancer patients in Hong Kong. The effect of mindful yoga on HRQoL and perceived stress in cancer patients is in line with prior research [15,16]. The effect of mindful yoga on diurnal cortisol levels is also consistent with prior findings [12] and theories on the relevance of cortisol to progression and prognosis of cancer [17]. Even Bonferroni correction was applied to the p value of paired- sample t-tests, the significant effect on HRQoL and perceived stress remained significant. On the other hand, the nonsignificant change in depression scores from pre- to post-intervention seems to be consistent with the results of a recent meta-analysis [28]. The finding that older participants were more benefited by mindful yoga in reduction of diurnal level of cortisol has not been reported in prior research. The reason for this is not immediately apparent but as the program was designed to be mild in physical intensity, it may be more appealing to or suitable for older participants. However, as normal aging is associated with an increase in cortisol level, [29] which is relevant to progression and prognosis of cancer, this finding may have implications to public health in aging societies.
In sum, the significance of present findings is twofold. First, to our best knowledge, this is the first study examining the effect of mindful yoga in cancer patients in Hong Kong. Although the health benefits of yoga have been studied in Parkinson’s disease [30] and patients with metabolic syndrome [31], data concerning the effects on cancer patients in Hong Kong are extremely scanty. Second, despite obvious limitations such as sample size and the absence of a control group, present findings may still play an important role in stimulating further research with vigorous designs to examine the potential of yoga as a complementary therapy for cancer patients, especially for older patients. Despite the significance of these preliminary findings, their implications should be interpreted cautiously because the small and homogenous sample limits generalization and replicability of findings. Without a control group, it is challenging to isolate the effect of yoga from that of well-established confounding variables such as maturation, history, and regression toward the mean.
Acknowledgement
This research was supported by the following grants (1) City University of Hong Kong SRG-Fd (7006068), (2) Science and Technology Innovation Committee of Shenzhen Municipality (JCYJ20210324133813036), and (3) Hong Kong Research Grants Council (C7008-22G and 11103523). Thanks, are also due to Mr. Ken Wong for leading the mindful yoga sessions, and Dr. Meijun WANG and Mr. Ho Yin TSANG for their technical help in cortisol assays.
References
- Kabat-Zinn J (2003) Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology: Science and Practice 10(2): 144-156.
- Baer RA (2003) Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical psychology: Science and practice 10(2): 125.
- Kabat-Zinn J (1982) An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General hospital psychiatry 4(1): 33-47.
- Teasdale JD, Segal Z, Williams JMG (1995) How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness) training help? Behaviour Research and Therapy 33(1): 25-39.
- Grossman P, Niemann L, Schmidt S, Walach H (2004) Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of psychosomatic research 57(1): 35- 43.
- Querstret D, Morison L, Dickinson S, Cropley M, John M (2020) Mindfulness- based stress reduction and mindfulness-based cognitive therapy for psychological health and well-being in nonclinical samples: A systematic review and meta-analysis. International Journal of Stress Management 27(4): 394.
- Fishbein D, Miller S, Herman-Stahl M, Williams J, Lavery B, et al. (2016) Behavioral and psychophysiological effects of a yoga intervention on high-risk adolescents: A randomized control trial. Journal of Child and Family Studies 25: 518-529.
- Schuver KJ, Lewis BA (2016) Mindfulness-based yoga intervention for women with depression. Complementary therapies in medicine 26: 85-91.
- Fischer JM, Kandil FI, Kessler CS, Nayeri L, Zager LS, et al. (2022) Stress reduction by yoga versus mindfulness training in adults suffering from distress: A three-armed randomized controlled trial including qualitative interviews (RELAX study). Journal of Clinical Medicine 11(19): 5680.
- Grensman A, Acharya BD, Wändell P, Nilsson GH, Falkenberg T, et al. (2018) Effect of traditional yoga, mindfulness-based cognitive therapy, and cognitive behavioral therapy, on health-related quality of life: a randomized controlled trial on patients on sick leave because of burnout. BMC complementary and alternative medicine 18: 1-16.
- Pascoe MC, Thompson DR, Ski CF (2017) Yoga, mindfulness-based stress reduction and stress-related physiological measures: A meta-analysis. Psychoneuroendocrinology 86: 152-168.
- Gard T, Brach N, Hölzel BK, Noggle JJ, Conboy LA, Lazar SW (2012) Effects of a yoga-based intervention for young adults on quality of life and perceived stress: the potential mediating roles of mindfulness and self-compassion. The Journal of Positive Psychology, 7(3): 165-175.
- Gonzalez M, Pascoe MC, Yang G, de Manincor M, Grant S, et al. (2021) Yoga for depression and anxiety symptoms in people with cancer: a systematic review and meta‐analysis. Psycho‐Oncology 30(8): 1196-1208.
- Hsueh EJ, Loh EW, Lin JJ A, Tam KW (2021) Effects of yoga on improving quality of life in patients with breast cancer: a meta-analysis of randomized controlled trials. Breast Cancer 28: 264-276.
- Chang YC, Yeh TL, Chang YM, Hu WY (2021) Short-term effects of randomized mindfulness-based intervention in female breast cancer survivors: a systematic review and meta-analysis. Cancer nursing 44(6): E703-E714.
- Bratborska AW, Piotrowski I (2024) The impact of yoga practice on cortisol levels in breast cancer patients-a comprehensive review. Oncology in Clinical Practice 20(6): 420-427.
- Miller S, Mendelson T, Lee-Winn A, Dyer NL, Khalsa SBS (2020) Systematic review of randomized controlled trials testing the effects of yoga with youth. Mindfulness 11: 1336-1353.
- Lam CLK, Wong CKH, Lam ETP, Lo YYC, Huang WW (2010) Population norm of Chinese (HK) SF-12 health survey-version 2 of Chinese adults in Hong Kong. Hong Kong Practitioner 32(2): 77-86.
- Hsiao FH, Jow GM, Kuo WH, Yang PS, Lam HB, et al. (2016) The long-term effects of mindfulness added to family resilience-oriented couples support group on psychological well-being and cortisol responses in breast cancer survivors and their partners. Mindfulness 7: 1365-1376.
- Ng SM (2013) Validation of the 10-item Chinese perceived stress scale in elderly service workers: one-factor versus two-factor structure. BMC psychology 1(1): 1-8.
- Zhang Y, Cui C, Wang L, Yu X, Wang Y, et al. (2021) The mediating role of hope in the relationship between perceived stress and post-traumatic stress disorder among Chinese patients with oral cancer: A cross-sectional study. Cancer Management and Research 393-401.
- Xu W, Zhou Y, Fu Z, Rodriguez M (2017) Relationships between dispositional mindfulness, self‐acceptance, perceived stress, and psychological symptoms in advanced gastrointestinal cancer patients. Psycho‐Oncology 26(12): 2157-2161.
- Zhong M, Goh PH, Li D, Bao J, Xu W (2020) Dispositional mindfulness as a moderator between perceived stress and psychological symptoms in Chinese digestive tract cancer patients. Journal of Health Psychology 25(6): 810-818.
- Tian X, Jin Y, Chen H, Tang L, Jiménez-Herrera MF (2021) Relationships among social support, coping style, perceived stress, and psychological distress in Chinese lung cancer patients. Asia-Pacific Journal of Oncology Nursing, 8(2): 172-179.
- Fong TC, Ho RT (2020) Mindfulness facets predict quality of life and sleep disturbance via physical and emotional distresses in Chinese cancer patients: A moderated mediation analysis. Psycho‐oncology 29(5): 894-901.
- Chin WY, Wan EYF, Choi EPH, Chan KTY, Lam CL K (2016) The 12-month incidence and predictors of PHQ-9-screened depressive symptoms in Chinese primary care patients. The Annals of Family Medicine 14(1): 47-53.
- Wang W, Bian Q, Zhao Y, Li X, Wang W, et al. (2014) Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. General hospital psychiatry 36(5): 539-544.
- Ma X, Li SN, Chan DNS (2025) Effects of yoga on cancer-related fatigue, psychological distress, and quality of life among patients with cancer undergoing chemotherapy and/or radiotherapy: a systematic review and meta-analysis. Cancer Nursing 48(3): 200-212.
- Stamou MI, Colling C, Dichtel LE (2023) Adrenal aging and its effects on the stress response and immunosenescence. Maturitas 168: 13-19.
- Kwok JYY, Chan LML, Lai CA, Ho PWL, Choi ZYK, et al. (2025) Effects of Meditation and Yoga on Anxiety, Depression and Chronic Inflammation in Patients with Parkinson’s Disease: A Randomized Clinical Trial. Psychotherapy and psychosomatics 94(2): 101-118.
- Lau C, Yu R, Woo J (2015) Effects of a 12-week hatha yoga intervention on metabolic risk and quality of life in Hong Kong Chinese adults with and without metabolic syndrome. PLoS One 10(6): e013073.






























