Abstract
Objective: Stress, fatigue, depression, and anxiety negatively impact quality of life in patients with relapsing-remitting multiple sclerosis (RRMS). Conventional treatments often offer limited relief and may increase patients’ distress. In response to interest in complementary approaches, we explored the safety and potential benefits of Tension Releasing Exercises (T.R.E.), a mind-body technique aimed at reducing deep muscular tension linked to chronic stress or trauma.
Methods: Twenty RRMS patients participated in a two-month intervention involving 24 T.R.E. sessions (three per week). Demographic, neurological, and clinical data were collected before and after the intervention. Outcome measures included MusiQoL, SF-36, fatigue severity, anxiety, depression, and treatment burden. Statistical analyses were conducted using IBM SPSS v23, with Mann-Whitney U tests and Benjamini-Hochberg correction. Significance was set at p<0.05.
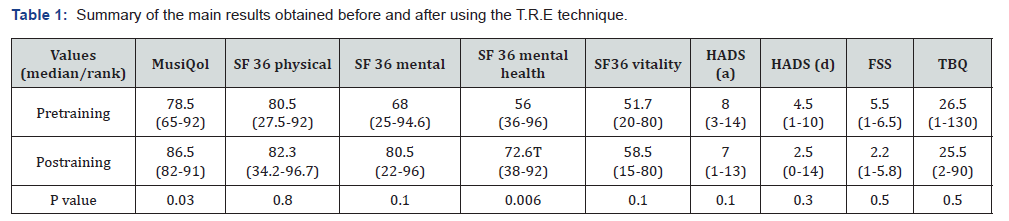
Results: Eighteen participants were women (mean age 43 ± 10 years), with a median disease duration of 7 years and EDSS of 1 (range 0–4). Only one participant had mild spasticity. No adverse effects were reported. MusiQoL scores improved from 78.5 to 86.5 (p=0.03), and symptom scores from 75.75 to 82.75 (p=0.025). No significant changes were observed in fatigue, vitality, or mood. EDSS, spasticity, and pharmacologic treatments remained stable. Treatment burden scores did not change, suggesting T.R.E. did not increase burden.
Conclusions: T.R.E. appears safe and may improve quality of life in RRMS patients without adding treatment burden. This low-cost, easily implemented technique warrants further investigation in larger trials and across other neurological and chronic conditions.
Keywords: Multiple Sclerosis; Quality of Life; Body-Mind Therapy; Fatigue
List of abbreviations: MS: Multiple Sclerosis; NCCIH: National Center for Complementary and Integrative Health; T.R.E: Tension-releasing exercises; MSp: Multiple Sclerosis patients; RRMS: Relapsing-remitting multiple sclerosis; TBQ: Treatment of Burden Disease Questionnaire; SF 36: Short Form 36; MusiQol: Multiple Sclerosis Quality of life; FSS: Fatigue Severity Scale; HADS: Hospital Anxiety and Depression Scale; ADL: Activities of Daily Living; PWB: Psychological Well-Being: RFr, RFa, RHCs: Relationship With Friends, Family And Healthcare System; PT: Symptoms; SSL: Sentimental and sexual life; COP: Coping; REJ: Rejection
Introduction
Multiple sclerosis (MS) is characterized as an inflammatory and degenerative disease, presenting a spectrum of symptoms that exert temporary or permanent impacts on the quality of life for affected individuals. Currently, 3.000.000 people worldwide grapple with this incurable condition, for which available symptomatic treatments exhibit limited efficacy. Like individuals with other chronic illnesses, those dealing with MS have increasingly turned to diverse medications and complementary techniques to improve their quality of life [1,2]. However, this practice raises two significant concerns: the unknown safety and efficacy of these interventions, and an insufficient consideration of the treatment burden. Mind-body therapies stand out as complementary techniques, acknowledged by the National Center for Complementary and Integrative Health (NCCIH) as methods grounded in the understanding of mind-body interactions [3,4]. These therapies aim to alleviate tension, mitigate the impact of stress, and bolster an individual’s physiological and psychological well-being.
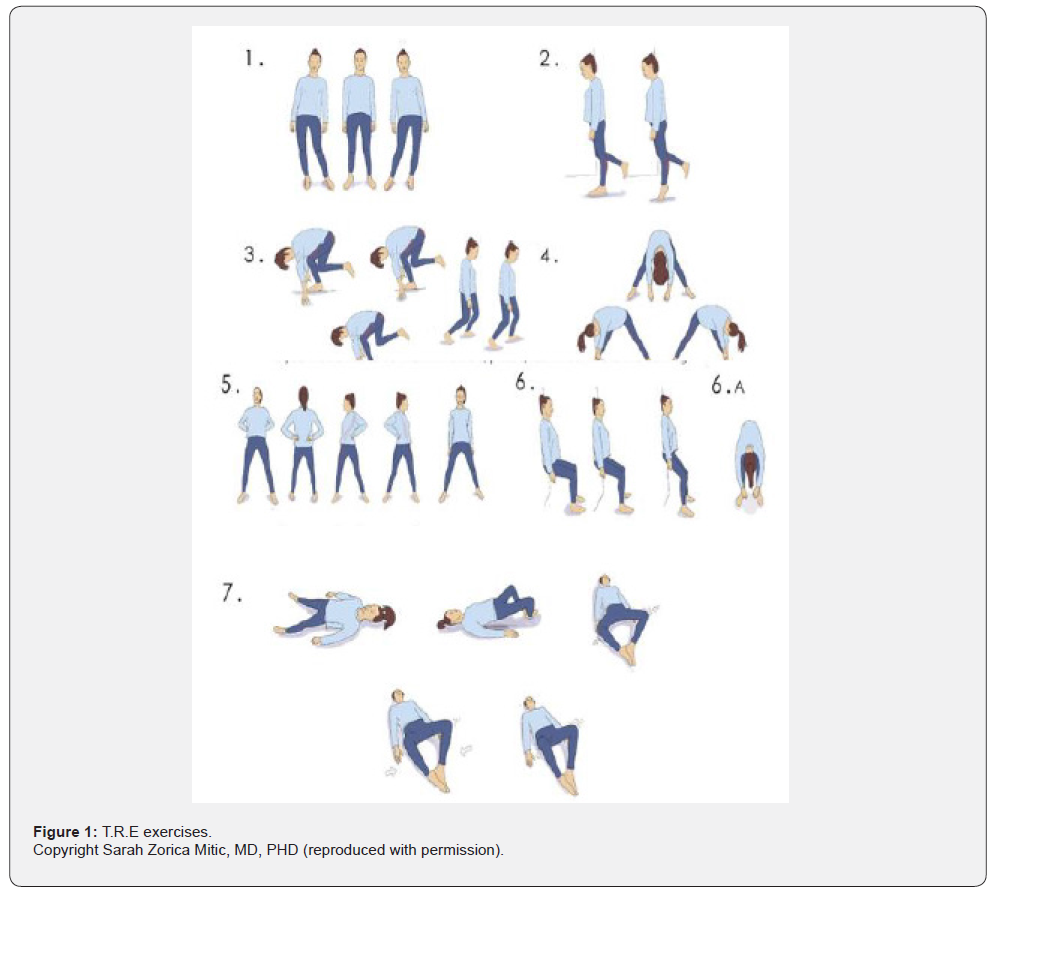
Tension and Trauma-releasing exercises (T.R.E ®) comprises seven different exercises, six performed in a standing position and one lying flat. The sequence primarily activates standing and breathing muscles in an ascending manner, ultimately inducing the appearance of a tremor with neurogenic characteristics. Positioned as a body-mind intervention, T.R.E operates on the premise that neuromuscular tremors release deep-seated muscle tension, contributing to the regulation of the autonomic nervous system and fostering a state of relaxation and calm. The precise mechanism of action, however, remains to be elucidated [5,6]. Simultaneously, the practitioners are instructed in concepts of self-regulation of experience, training the moderation of personal self-demand. Currently there are few publications evaluating the impact of T.R.E on health and none considering burden of treatment and quality of life [7]. Additionally, only one trial on Multiple Sclerosis patients (MSp) has been published, providing limited data [8]. Our pilot study aims to fill this crucial gap by rigorously assessing the safety (with a focus on physical injury, emotional distress, fatigue, and treatment burden) and potential benefits (including improvements in quality of life, symptomatic relief, and vitality) of T.R.E in individuals diagnosed with relapsingremitting multiple sclerosis (RRMS).
Materials and Methods
Study Design
This clinical interventional pilot study aimed to assess the impact of T.R.E on individuals with RRMS. The training occurred during the transition from spring to summer in the southern hemisphere, spanning 25 sessions held three times a week, adopting a hybrid approach (two in-person and one remote). The extension of the trial was set considering previous communications with an avoidance of the summer season to minimize the potential confounding factor of ambient heat The T.R.E session lasted 60-minutes, including 10 minutes at the beginning and end dedicated to sharing experiences, fostering a supportive environment. Certified T.R.E ® instructors, a body-mind therapist, and a neurologist led the exercises, and participants were expected to attend at least 75% of the sessions. Longitudinal assessments were conducted during each session, with patients acting as their own controls. Two main questions were addressed in this trial: Is it safe for RRMS individuals to practice T.R.E? Is it beneficial for RRMS individuals to practice this technique?
Participants
Given the absence of solid precedents on T.R.E interventions on MSp, a sample size based on power calculations couldn’t be established. We consider including 20 patients as a reasonable number. Randomly invited 25 fully ambulatory patients from our service, 21 of them agreed to participate. Inclusion criteria were
1) 18 to 65 years of age
2) Have a diagnosis of RRMS
3) Maintain the use of disease-modifying therapy
throughout the study
4) Having received at least one dose of COVID-19 vaccine
5) Capable of performing standing exercises
Exclusion criteria included presence of relapses, use of steroids in the past 90 days or not giving informed consent. The study was approved by our Local Ethical Committee. All patients signed an informed consent.
T.R.E Training
The T.R.E training involved a fixed sequence of 7 exercises designed to stimulate large joints and muscle groups, inducing autonomic stress responses (Figure 1). The purpose was to elicit a tremor mimicking physiological self-regulation during stress without re-experiencing trauma. Sessions also focused on teaching self-regulation of physical symptoms (e.g., tiredness, fatigue, cramps) and emotional experiences (e.g., fear, anguish, irritability).
Clinical and Demographic Evaluation
Neurological evaluation was conducted at beginning and ending of the training by a physician experienced on MSp. It included measuring of: EDSS, Ashworth Scale, and 25-step walk test. Demographic data were recorded, as along with any changes in MS-specific treatment, the need of symptom-related medication, the presence of relapses, and modifications in physical activity routines.
Safety Evaluation Test
The treatment of Burden Disease Questionnaire (TBQ), was administered at the beginning and the end of the training period. TBQ is a self-reported validated measure for MS patient assessing the effects of treatment burden on patient wellbeing. The validated Spanish version consists of 13 questions addressing tasks MS patients face in daily life. The scale ranges from 0, i.e.no issues about self-care, to 130, highest level of complaint over managing MS-related medical indications and dealing with the health care system [9].
Benefits Evaluation
Four scales were utilized for benefits evaluation, including, Musiqol and SF 35 for quality of life, FSS for fatigue, and the Hospital Anxiety and Depression Scale (HADS) for emotional testing.
We chose to include MusiQol due to is the best specific tool approved and Spanish validated for evaluating individuals with MS. MusiQol is a self-administered questionnaire encompassing 9 domains (activities of daily living (ADL); psychological wellbeing (PWB); relationship with friends, family and healthcare system (RFr, RFa, RHCs); symptoms (SPT); sentimental and sexual life (SSL); coping (COP); and rejection (REJ). MusiQol has also an index score which is calculated as the mean of the individual domains. The point rank from 0 (no QoL) to 120 (representing the best QoL) [10]. Related with previous publication, we were aware about the importance of vitality on MSp [11]. We decided to add SF36 because its subitems would allow us to quantify markers such as vitality and discriminate quality of life in the physical and emotional axis. SF 36 is a well-known self-administered scale comprising 36 items grouped in 8 separate scores, namely: physical functioning, social functioning, role-physical, role-emotional, mental health, vitality, bodily pain, and general health. Two final measures are calculated, the physical component summary (PCS) and mental component summary MCS) [12]. MusiQol as well SF 36 feature scores from 0 to100, where 0 represents the lowest and 100 the highest quality of life (QOL) level.
To assess fatigue severity, we employed the Fatigue Severity Scale (FSS), a self-administered nine-item questionnaire. The FSS measures the severity of fatigue and its impact on a person’s activities and lifestyle in the previous week. FSS scores range from 1 to 7, with higher scores indicating more severe fatigue. Values above 4 are considered indicative of significant fatigue [13]. The Hospital Anxiety and Depression Scale (HADS) was utilized to evaluate anxiety and depression. This scale comprises two variables, one measuring anxiety, with seven items, and a separate set measuring depression. Scores between 0 and 7 are considered normal, scores between 8 and 10 indicated mild symptoms. Scores exceeding 10 suggest the presence of significant anxiety or depression are present [14].
Statistical Analysis
IBM SPSS Statistics v23 software (Armonk, NY: IBM Corp) was used for statistical analyses. Unless otherwise indicated, continuous variables were reported as median and interquartile range (IQR), while categorical variables were presented as percentages (%) of total number of patients. To assess differences between groups the Mann-Whitney’s U test was employed considering the non-parametric nature of the data. Multiple test correction was performed using the Benjamini-Hochberg procedure to decrease rates of false discovery. Significance was established at p-values below 0.05.
Results
Demographic and Clinical Parameters
A total of 21 patients were initially enrolled and 20 successfully completed the trial. One participant withdrew from the study prematurely due to unrelated T.R.E health issues, and their data was excluded from the analysis. The average attendance was 18.5 sessions representing 75% completion rate. The distribution of attendance was as follows: ≥ 75%: 13 out of 20 patients; 51%- 74%: 6 out of 20 patients; and 50% 1for 1 out of 20 patients. Of the 20 patients studied, 18 were women and 2 men. The mean age was 43 years (SD ±10). The median disease duration was 7 years (range 1-25). The median EDSS was 1 (range 0-4). Only one patient had mild spasticity (Ashworth 1) meanwhile the rest of the group didn’t have spasticity.
Test Results
Clinical And Safety Results
No patient required additional pharmacological symptomatic medication or reported major or minor injuries. Actually, some MSp reported some dose reduction of symptomatic treatment for sleep disorders, anxiety, and restless leg syndrome although its value was not statistically significant. EDSS, Ashworth, 25-step walk test scales remain unchanged. One participant discontinued the training due to health issue not related with the protocol. Regarding TBQ Median score was 26.5, a value that did not change significantly by the end of the study (median 25.5) (p= 0.5).
Benefit Test Results
• MSQ
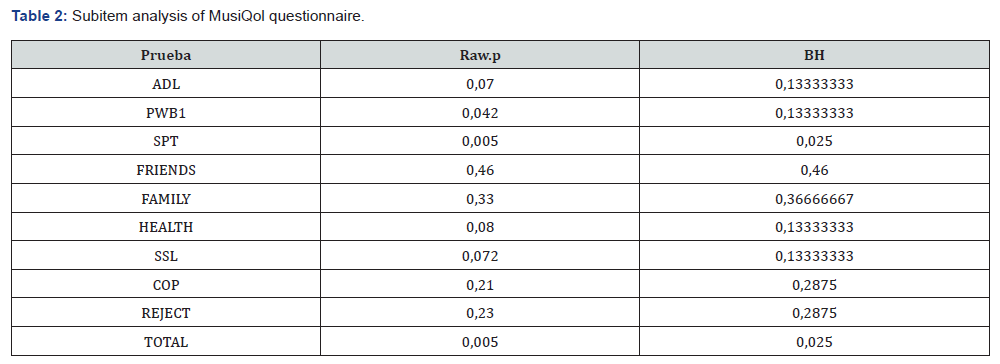
The median pre-training score was 78.5 (rank 65-92). Posttraining score was 86.5 (rank 82-91) (p= 0.03). Although fatigue and emotional load had not changed, quality of life improved. A second analysis of individual MusiQol domains was conducted to identify any single item that could explain these results. Symptom assessment significantly improved after training (p= 0.025).
• SF 36
Median differences in physical or mental components before and after training did not reach statistical significance. However, individualized item analysis revealed a significant improvement in “mental health” at the end of the study (p= 0.006).
• HADs Anxiety, Depression, and Fatigue
Only 4 patients reported significant symptoms of anxiety. Post-training scores showed a trend, although not statistically significant, towards improvement. Regarding the depression subscale, 3 patients reported mild symptoms, at the beginning, and none reported severe depression. Post-training values did not show significant modifications.
• FSS
Nine patients met the criteria for significant fatigue at the beginning of the study, seven of whom maintained similar values at the end of the study. Although the analysis of individual cases indicated some had improved significantly, the group analysis showed no impact on fatigue.
These data are summarized in (Table 1).
Discussion
Multiple sclerosis is a chronic, degenerative, inflammatory disease that predominantly affects young, socially, and economically active people. The symptoms often persist through life, negatively impacting the QoL [2,11]. Patients seek alternative or complementary therapeutic methods when allopathic medical approach fails to improve symptoms [15]. Although there is growing evidence on the safety and efficacy of certain alternatives medical approaches, more work still needed to establish solid indications based on evidence medicine [16]. In this context, our objective was to evaluate the benefits and risks of a new bodymind technique call T.R.E. Only one study has been published testing a T.R.E. program on nine MSp [8]. The program taught once a week, spanning a total of nine sessions, demonstrating some improvements in spasticity, fatigue, and day-to-day symptoms, including stress, and sleep quality. Although QoL and the treatment burden of disease were not measured, they have laid the groundwork for future lines of research in MS trials (Table 2).
FSS: Fatigue Severity Scale
HADS (a): Hospital Anxiety and Depression scale (anxiety score)
HADS (d): Hospital Anxiety and Depression scale (depression score)
MSQ: MusiQol. Multiple Sclerosis Quality of life questionnaire.
SF36 Short Form 36
TBQ: Treatment of Burden questionnaire
In this exploratory study, we evaluated the safety and benefits of 20 MS patients before and after completing a T.R.E program three times a week for two months (24 sessions). The results of the safety testing showed no side effects. Indeed, a few patients reported a reduction in their use of symptomatic medications, although this did not reach statistical significance. The benefits of developing coping skills were evident in MusiQol scores, with significant improvements observed, particularly for the symptoms subitem. The scale scores showed a notable range narrowing at the end of training, shifting from 65-92 to 82-91. Quality of life is a unique combination of physical characteristics, emotional resources, and mental abilities at a specific moment in a person’s life. In this sense, we confirmed the impact of T.R.E on QoL, the most encompassing variable.
While our initial working hypothesis anticipated significant improvements in fatigue, vitality, and emotions, no such improvements were observed. The lack of improvement in fatigue could be attributed to the initially low values on the FFS scale for most patients included in the study’s commencement. Future studies incorporating patients with higher fatigue scores may unveil potential benefits. Additionally, fatigue in MS tends to fluctuate and is notably influenced by changes in body temperature. Despite efforts to control this variable, the study was conducted in late spring and early summer, potentially impacting the results. Concerning vitality, only a specific subitem on the SF36 scale could serve as an indicator, but unfortunately, we could not demonstrate significant differences in TRE for this symptom. Given its complexity, the precise measurement of vitality may surpass the capabilities of current assessment scales.
Regarding emotional impact, the overall evaluation of the SF36 scale revealed significant data, primarily associated with the mental health subitem, although not reflected in the mental component of the SF36 evaluation. No changes were observed in the physical component of the SF36, aligning with the stable results of the EDSS, the walking test, and the Ashworth scale. All the tasks a person must undertake to manage their health after an MS diagnosis are defined as the burden of disease [17], quantifiable through the TBQ questionnaire [9]. In this sense, we demonstrated that T.R.E training, either during sessions or home exercises three times a week for at least two months, did not increase the burden of treatment, and the schedule did not adversely affect adherence.
While the mechanism of action of T.R.E is not yet reliably known, the underlying theory suggests that neuromuscular tremors release deep muscle tension, contributing to the regulation of the autonomic nervous system and generating a state of relaxation and calm [5-7] Meanwhile, different organs inform the central nervous system about events that can balance or unbalance physical or mental health. The maintenance of this complex system of responses relies on the correct functioning of neuroendocrine, autonomic, metabolic, cardiovascular, and immune pathways [18]. These is also described as “Top-Down/ Bottom -Up” regulation mechanism model [19]. At molecular level, it has been published that regular practice of yoga together with meditation and breathing techniques (considered a body -mind approach) improved the adrenal response to stress evidenced by a decrease in basal cortisol.
Simultaneously, some researches on physical activity, mindfulness and cognitive therapies had shown reduction of biochemical molecules that modify neuronal plasticity (e.g., BDNF, VEGF, IGF-1), reduce inflammation, or metabolic and stress-related mediators and changes in gray matter. Although the intrinsic mechanism of T.R.E intervention is still unknow it could be possible that some of the previous physical changes may be involved [20-26]. We acknowledge the limitations of this study, with the most significant one being the small sample size of our study population. However, it’s crucial to note that this is an exploratory study. Additionally, the inclusion of MS patients with low levels of disability may have influenced the results. Including MS patients with a higher EDSS or Ashworth scale could potentially yield more significant results. Despite these limitations, we interpret the greatest strength of our study to be the potential improvement in quality of life without increasing the burden of treatment, thanks to a low-cost and easily implementable intervention.
Conclusion
TRE proved to be a safe body-mind technique that enhanced the quality of life without increasing the treatment burden or causing undesirable effects in relapsing-remitting MS patients. Additionally, we observed that the program was easy to follow and had a meager economic cost. Based on our findings, we encourage the scientific community to incorporate new complementary treatment strategies for MS and a wide range of neurological chronic conditions that limit the quality of life without increasing the burden of treatment. This should be the ultimate therapeutic goal for both patients and physicians.
Acknowledgments
To Fundación Columbia de Concienciay Energía. Buenos Aires. Argentina without whose unconditional support, this study could not have been completed.
To T.R.E Argentina, for their generous, free labor.
To Dr Ismael Calandri, MD, Buenos Aires, Argentina, for the statistical assistance and review.
To all the people with Multiple Sclerosis who contribute to the permanent search for a better life. Especially to those who participated with great commitment in this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Peter Rieckmann, Diego Centonze, Irina Elovaara behalf MS in the 21st Century Steering Group (2018) Unmet needs, burden of treatment, and patient engagement in multiple sclerosis: A combined perspective from the MS in the 21st Century Steering Group. Multiple Sclerosis and Related Disorders 19: 53-160.
- Berrigan L, Fisk J, Patten S, Tremlett H, Wolfson C, et al. (2016) Health-related quality of life in multiple sclerosis. Neurology 86(15): 1417-1424.
- Kliger B, Lee R, Shiflett S (2004) Integrative medicine: Basic Principles. In Integrative Medicine. Principles for practice. Mc Graw Hill 3-23.
- Wahbeh H, Elsas S, Oken B (2008) Body mind intervention. Neurology 70(24): 2321-2328.
- Berceli D (2015) Shake it off naturally: reduce stress, anxiety and tension with (TRE). CreateSpace: IX-XII.
- Porges S (2009) The polyvagal theory: New insights into adaptive reactions of the autonomic nervous system. Cleve Clin J Med 76(Suppl 2): S86-S90.
- Berceli D, Salmon M, Bonifas R, Ndelfo N (2014) Effects of self-induced unclassified therapeutic tremors on quality of life among non-professional caregivers: a pilot study. Glob. Adv. Health Med 3(5): 45-48.
- Lynning M, Svane C, Westergaard K, Bergien S, Gunnersen S, et al. (2021) Tension and trauma releasing exercises for people with multiple sclerosis-An exploratory pilot study. J Tradit Complement Med 11(5): 383-389.
- Ysrraelit MC, Fiol MP, Peña FV, Vanotti S, Terrasa SA, et al. (2019) Adaptation and validation of a Spanish version of the treatment burden questionnaire in patients with multiple sclerosis. BMC Neurol 19(1): 209.
- Fernández O, Fernández V, Baumstarck-Barrau K, Muñoz L, Gonzalez Alvarez M, et al. (2011) Validation of the spanish version of the Multiple Sclerosis International Quality of Life (Musiqol) questionnaire.BMC Neurol 11: 127.
- Ysrraelit MC, Fiol M, Gaitán MI, Correale J (2018) Quality of Life Assessment in Multiple Sclerosis: Different Perception between Patients and Neurologists. Front Neurol 8: 729.
- Augustovski F, Lewin G, García-Elorrio E, Rubinstein A (2008) The Argentine-Spanish SF-36 Health Survey was successfully validated for local outcome research.J Clin Epidemiol 61(12): 1279-1284.
- Krupp L, LaRocca N, Muir-Nash J, A D Steinberg (1989) The Fatigue Severity Scale. Application to Patients with Multiple Sclerosis and Systemic Lupus Erythematosus. Arch Neurol 46(10): 1121-1123.
- Herrero M, Blanch J, Peri JM, De Pablo J, Pintor L, et al. (2003) A validation study of the hospital anxiety and depression scale (HADS) in a Spanish population.Gen Hosp Psychiatry 25(4): 277-283.
- Sastre-Garriga J, Munteis E, Rio J, Pericot I, Tintoré M, et al. (2003) Unconventional therapy in multiple sclerosis. Mult Scler 9(3): 320-322.
- Yadav V, Bever Ch, Bowen J, Bowling A, Weinstock-Guttman B, et al. (2014) Summary of Evidence-Based Guideline: Complementary and Alternative Medicine in Multiple Sclerosis, Neurology 82(12) :1083-1092.
- Sav A, King M, Whitty J, Kendall E, McMillan S, et al. (2015) Burden of treatment for chronic illness: a concept analysis and review of the literature. Health Expect 18(3): 312-324.
- Kern S, Ziemssen T (2008) Brain-immune communication psychoneuroimmunology of multiple sclerosis. MSJ 14: 6-21.
- Gill Taylor A, Goehler L, Galper D, Innes K, Bourguignon Ch (2010) Top-Down and Bottom-Up mechanisms in Mind Body Medicine: Development of integrative framework for psychophysiological research. Explore 6: 29-41.
- Cahn B, Goodman M, Peterson Ch, Maturi R, Mills P (2017) Yoga, Meditation and Mind-Body Health: Increased BDNF, Cortisol Awakening Response, and Altered Inflammatory Marker Expression after a 3-Month Yoga and Meditation Retreat. Front. Hum. Neurosci 11: 315.
- Van Aalst J, Ceccarini J, Demyttenaere K, Sunaert S, Van Laere K (2020) What Has Neuroimaging Taught Us on the Neurobiology of Yoga? A Review. Front. Integr. Neurosci 14: 34.
- Singleton O, Hozel B, Vangel M, Brach N, Carmody H, et al. (2014) Changes in brainstem gay matter concentration following an indulness-based intervention is correlated with imporvement in psychological well-being. Frontiers in Human Neuroscience 8: 33.
- Müller P, Duderstadt Y, Lessmann V, Notger G, Müller N (2020) Lactate and BDNF: Key Mediators of Exercise Induced Neuroplasticity?. Clin. Med 9: 1136.
- Sauder T, Keune P, Müller R, Schenk T, Oschmann P, et al. (2021) Trait mindfulness is primarily associated with depression and not with fatigue in multiple sclerosis (MS): implications for mindfulness-based interventions. BMC Neurol 21(1): 115.
- Cavalera C, Rovaris M, Mendozzi L, Pugnetti L, Garegnani M, et al. (2019) Online meditation training for people with multiple sclerosis: A randomized controlled trial.Multiple Sclerosis Journal 25(4): 610-617.
- Simpson R, Sharon Simpson S, Marina Wasilewski M, Mercer S, Lawrence M (2021) Mindfulness-based interventions for people with multiple sclerosis: a systematic review and meta-aggregation of qualitative research studies. Disabil Rehabil 9: 1-15.






























