Abstract
Asthma is a chronic respiratory condition characterized by airway inflammation and bronchial hyper-responsiveness, leading to recurrent episodes of wheezing, breathlessness, and coughing. Yogic practices, including breathing exercises (pranayama) and physical postures (asanas), have been increasingly recognized as complementary therapies for respiratory diseases. This study evaluates the effect of a structured yogic regimen on Forced Vital Capacity (FVC), Maximum Voluntary Ventilation (MVV), and Peak Expiratory Flow Rate (PEFR) in asthmatic patients. Eighty participants with moderate asthma underwent a 12-week yoga intervention. Pre- and post-intervention respiratory parameters were assessed. Significant improvements were observed, indicating that yogic practices may enhance lung function and overall respiratory health.
Keywords: Asthma; Yoga; Pulmonary Function; FVC; MVV; PEFR; Pranayama
Abbreviations: FVC: Forced Vital Capacity; MVV: Maximum Voluntary Ventilation; PEFR: Peak Expiratory Flow Rate
Introduction
Asthma affects millions of individuals globally, posing substantial health and economic burdens. Standard treatments typically include inhaled corticosteroids and bronchodilators, but non-pharmacological interventions such as yoga have gained attention for their holistic benefits. Yogic techniques emphasize controlled breathing, relaxation, and posture alignment, which may improve respiratory muscle strength, lung elasticity, and stress management, contributing to better asthma control.
This study aims to investigate the impact of yogic practices on key pulmonary function tests:
1.Forced Vital Capacity (FVC) - a measure of the maximum amount of air exhaled after a deep inhalation.
2.Maximum Voluntary Ventilation (MVV) - the greatest volume of air that can be inhaled and exhaled within a minute.
3.Peak Expiratory Flow Rate (PEFR) - the highest speed of exhalation.
Previous studies have explored the potential benefits of yoga in managing respiratory disorders, particularly asthma. Vedanthan et al. [1] conducted a randomized controlled trial demonstrating significant improvements in pulmonary function tests and reduced medication dependency among asthma patients practicing yoga. Similarly, Singh et al. [2] found that regular pranayama exercises enhanced peak expiratory flow rates and reduced asthma symptoms in adolescents. Nagendra HR et.al [3] states that the practice of Pranayama improves the lung capacity. Study done by [4] shows that effect of Yogic practices improves the flexibility and respiratory measure of vital capacity and breath holding time.
Mestan J [5] found no significant difference between inspiratory volume and Kumbhaka period/duration of Pranayama. [6] found that slight increase in pick flow rate due to practice of Anulom-Vilom Pranayama. Joshi AR et.al. [7] observation during their study reflects that the practice of Yoga influence the Pulmonary function. During another study Usha G et.al [8] observed an influence of breathing exercise on pulmonary function tests. Joshi LN et.al [9] observed the effect of short-term Pranayama practice on breathing and ventilation function of lungs was significant. Desai BP et.al. [10] states that the effect of one attempt and five attempt of Kapalbhati on plasma fibrinogen level in normal subjects was significantly increased after single and five consecutive attempts of Kapalbhati of one minute duration each in normal subjects. In another study Gore MM et.al [11] the effect of ten minutes Kapalbhati on some physiological functions has been observed and it has been found that the heart rate and eye movements increase and the finger pulse volume decreases significantly as well as the respiration rate decreased immediately after Kapalbhati.
Another study by Cooper et al. [12] highlighted the psychological benefits of yoga, showing reduced anxiety and better asthma-related quality of life scores. Pranayama techniques like Bhastrika and Kapalbhati are thought to improve airway patency and lung compliance [13]. The combination of controlled breathing, muscle relaxation, and improved posture alignment in yoga helps enhance respiratory efficiency and resilience to triggers. The findings from these studies provide a foundation for further exploration into how structured yogic interventions can optimize respiratory health outcomes, including FVC, MVV, and PEFR, in asthmatic populations.
Methodology Eighty asthmatic patients, aged 20-50 years, were selected from hospitals of Haridwar. Participants were divided into a yoga intervention group (n=40) and a control group (n=40). Inclusion criteria included a diagnosis of moderate persistent asthma and stable medication use. Exclusion criteria included other respiratory or cardiovascular conditions.
Intervention Protocol
The yoga intervention consisted of:
• Pre asana practices: Joints loosening with slow breathing
and Kapalbhati Kriya.
• Asanas: Tadasana, Tiryak-tadasana, Bhujangasana,
Dhanurasana, Gomukhasana, and Shavasana.
• Pranayama: Anulom Vilom, Bhastrika and Suyabhedi
Pranayama
• Meditation and Relaxation: 10 minutes of So-Ham
Sadahana meditation.
Sessions were conducted six days in week for three months, each lasting 60 minutes. The control group continued their standard medical treatment without yoga.
Data Collection
Pulmonary function tests (FVC, MVV, and PEFR) were measured using a spirometer at baseline and after 12 weeks.
Results:
(Table 1)
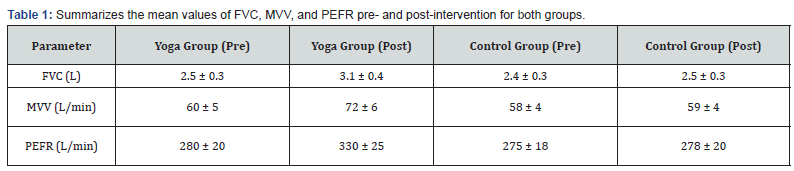
Statistical analysis using paired t-tests showed significant improvements in the yoga group (p < 0.05) for all parameters, whereas the control group exhibited minimal changes.
Discussion
The findings indicate that a 12-week yoga regimen substantially improves pulmonary function in asthmatic patients. Enhanced FVC and MVV suggest better lung capacity and respiratory muscle strength, while increased PEFR indicates improved expiratory flow and airway clearance. Yogic practices produce consistent physiological changes and have sound scientific basis. Kumar K [14] observed a significance of Nadi Sodhan and Kapalbhati practice on forced ventilation capacity (FVC), maximum voluntary ventilation (MVV) and picks expiratory flow rate (PEFR). Madanmohan Rai et.al [15] found a cardio respiratory change during Savitri Pranayama and Shavasana. Telles S et.al [16] find in another study a better Oxygen consumption in the subjects during pranayamaic type of very slow-rate breathing Kulkarni V A et.al [17].
Effect of short-term Yoga training program on peak expiratory flow rate is significant. Oak J P et.al [18]. Practice of Yoga, including Nadi Shodhan having a positive impact in the treatment of a case of coxalgia. The benefits of pranayama may be attributed to controlled breathing patterns, which reduce bronchospasm and enhance parasympathetic tone. Postures like Bhujangasana and Dhanurasana stretch thoracic muscles and improve lung expansion. Furthermore, relaxation techniques may lower anxiety and stress, known asthma triggers.
Conclusion
Yogic practices offer a promising complementary approach to managing asthma by improving critical lung function parameters. Incorporating yoga into standard care could enhance quality of life and reduce the frequency of asthma exacerbations. Future studies with larger samples and long-term follow-up are recommended to validate these findings.
dropdown Start here
References
- Vedanthan PK, Kesavalu LN, Murthy KC, Duvall K, Hall MJ, et al. (1998) Clinical study of yoga techniques in university students with asthma: A controlled study. Allergy and Asthma Proceedings 19(1): 3-9.
- Singh V, Wisniewski A, Britton J, Tattersfield A (2009) Effect of yoga breathing exercises (pranayama) on airway reactivity in subjects with mild asthma. Thorax 54(12): 1102-1106.
- Nagendra HR, Nagaratna R (1985) Yoga for bronchial Asthma- A control study, Brit Med Res 291: 1077-1080.
- Robson Moses (1973) Effect of Yoga on flexibility and respiratory measure of vital capacity and breath holding time, completed research in Health Physical Education and Recreation 15: 97.
- Mestan J, Bhole MV (1979) Cardiac out-put in normal, deep and Ujjayi Pranayamic breathing, Yoga Mimansa 19(4): 11-17.
- Gore MM (1981) Effect of Yogic Training on Peak expiratory flow rate, Yoga Mimansa 20(1&2): 100-104.
- Joshi AR & Pansare MS (1985) Effect of Yoga on Pulmonary function test, Indian J Physiol Pharmacol 36(2): 105.
- Usha G, Samosundram KBV (1986) Influence of breathing exercise on pulmonary function tests, Indian J Physiol Pharmacol 30 (5): 50-54.
- Joshi LN Joshi VD, Gokhale LV (1992) Effect of short-term Pranayama practice on breathing and ventilation function of lungs, Indian J Physiol Pharmacol 36(2): 105-108.
- Desai BP, Ghatore ML (1986) The effect of one attempt and five attempt of Kapalbhati on plasma fibrinogen level in normal subjects; Modern Perspectives in Physical Education and Sports, Harnam Publications, India.
- Gore MM, Ghatore ML, Rajpurkar MV (1989) Effect of ten minutes Kapalbhati on some physiological functions, Yoga Mimansa 28 (3): 1-11.
- Cooper S, Oborne J, Newton S, Harrison V, Thompson C, et al. (2003) Effect of two breathing exercises (Buteyko and pranayama) in asthma: A randomised controlled trial. Thorax 58(8): 674-679.
- Goyeche JR (1979) Yoga and anxiety. Medical Psychotherapy 3: 8-13.
- Kumar K (2013) Significance of Nadi Sodhan and Kapalbhati on forced ventilation capacity (FVC), maximum voluntary ventilation (MVV) and picks expiratory flow rate (PEFR); Indian Journal of Traditional Knowledge; N I S C A I R, New Delhi 12(2): 342-345.
- Madanmohan Rai UC, Balavittal V, Thombre DP, Gitananda (1983) Swami Cardiorespiratory changes during Savitri Pranayama and Shavasana, The Yoga review 3: 25-34.
- Telles S, Desiraju T (1991) Oxygen consumption during pranayamaic type of very slow-rate breathing, Indian J Med Res 94: 357-363.
- Kulkarni VA, Datar SV, Katti VA (1997) Effect of short-term Yoga Training program on peak expiratory flow rate, Yoga Mimansa, 32(1&2): 14-20.
- Oak JP, Bhogal RS (1997) Treatment of Coxalgia through Yoga: A client centred therapy approach – A case study; Yoga Mimansa 32(3).






























