Combating Loneliness with Yoga: A Psychoneuroimmunological Perspective
Chuk Ling Julian LAI*
Department of Social and Behavioral Sciences City University of Hong Kong
Submission:July 2, 2024;Published: July 18, 2024
*Corresponding author: Chuk Ling Julian LAI, Department of Social and Behavioral Sciences, City University of Hong Kong, Hong Kong SAR, China
How to cite this article: Chuk Ling Julian L. Combating Loneliness with Yoga: A Psychoneuroimmunological Perspective. J Yoga & Physio. 2024; 11(4): 555818 DOI:10.19080/JYP.2024.11.555818
Abstract
Recent research has identified loneliness as one of the most crucial factors contributing to ill health and mortality. The rising prevalence of loneliness has triggered a proliferation of intervention studies aimed at addressing loneliness. However, most of these studies have treated loneliness as a lack of company or social skills without paying due attention to enhanced inflammation, which is one of the key factors explaining ill health in lonely individuals. In this paper, I postulate from a psychoneuroimmunological perspective that yoga can reduce loneliness by improving systemic inflammation. To support this contention, I reviewed evidence from psychobiological research on loneliness and conducted a quantitative summary of findings from recent studies examining the impact of yoga on inflammatory parameters. Results show that the effect size of yoga on inflammatory parameters is g = 0.59 (95% CI [0.26 - 0.92], p < .001), which is almost 4 times larger than that associated with the effect of psychological interventions reported in another recent review. Given the rise of the prevalence of loneliness and mounting evidence showing the connection of this psychological condition with altered inflammatory responses, the present analysis provides support for promoting yoga as an evidence-based solution to reduce loneliness. As yoga is a training suitable for all age groups and compatible with lifestyle interventions, this further illustrates the significant implications of yoga for public health.
Keywords: Loneliness; Inflammation; Yoga; Psychoneuroimmunology; Public Health
Abbreviations: IL-1: interleukin-1; IL-6: Interleukin-6; TNFα: tumor necrosis factor alpha; MBTs: Mind-Body Therapies; TC: Tai Chi; QG: Qigong; YA: Yoga; MED: Meditation; RCTs: Randomized Controlled Trials
Introduction
Loneliness is one of the most crucial factors associated with morbidity and mortality and has been regarded as a major public health challenge [1]. Loneliness is conceptually different from social isolation, which is an objective measure of the lack of social relationships and interactions. Loneliness relates to the quality rather than the quantity of social relationships. Thus, individuals can be socially content when alone or lonely in a crowd [1]. Because of the immense health implications of loneliness, numerous interventions to reduce loneliness have been tested in a growing number of studies. Masi et al. [2] conducted a meta-analysis of 50 studies, of which 20 involved randomized group comparisons, to assess the effectiveness of these interventions. The pooled effect size (Hedge’s g) of the 20 randomized trials was small (-0.198) but significant (95% CI [-0.32 – - 0.08], Z = -3.182), with minimal heterogeneity found between studies (Q = 21.65, p = .30, I2 = 12.25%).
However, the interventions used in these studies all targeted the psychosocial or social-cognitive aspects of loneliness without accounting for the psychoneuroimmunological features associated with the lonely phenotype. Lai et al. [3] pointed out that loneliness is associated with an accentuation of nonspecific immunity, which results in increased inflammation and impaired antiviral response. A recent longitudinal study showed that the upregulation of genes involved in inflammation and downregulation of genes associated with antiviral response is associated with an increase in loneliness [4]. These suggest that loneliness can be decreased by interventions that mitigate or reverse its immunological features. The following review of the psychoneuroimmunological perspective highlights the theoretical support of this hypothesis.
A Psychoneuroimmunological Perspective of Loneliness
According to the seminal review paper by Maier and Watkins [5], cytokines play a central role in bidirectional communication between the brain and the immune system. The immune system components, which include antigen-presenting cells such as macrophages, T-helper cells, and B cells, work together to neutralize the invasion of foreign substances (e.g., bacteria and viruses). The highly coordinated interaction among immunocompetent cells is made possible by the cytokines secreted by these cells. Because a specific immune response takes at least several days or even longer to develop, nonspecific immunity serves as the first line of defense to initiate a response to any invading infectious agent to contain the infectious agent as close to the site of entry as possible. This takes less time because of the large number of cells that can respond to infectious agents in a nonselective manner. The concentration of activated immune cells at the site of entry is a unique feature of inflammation. Activated macrophages secrete cytokines interleukin-1 (IL-1), interleukin-6 (IL-6), and tumor necrosis factor alpha (TNFα), which cause local inflammation. In addition to local inflammation, there is a global response that cannot take place without the participation of the brain. Cytokines secreted by immune cells in the periphery find their way to lymphatic organs, which send signals to the brain via the vagus nerve.
In response to the afferent signals, the brain releases cytokines, primarily IL-1, to activate a global response involving a multitude of physiological and behavioral changes associated with what we call “sickness”. This is an adaptive response that facilitates recovery from illness or injury. The global response also involves the activation of the sympathetic nervous system and the hypothalamic-pituitary-adrenocortical axis to release catecholamines and cortisol, which is also observed in organisms exposed to stressors. Most relevant to my analysis are the following behavioral features of sickness: drowsiness, enhanced responsiveness to pain, loss of appetite, reduced activities and social interactions, reduced sexual behavior, and increased depressive mood [5], which are consistent with the concept of loneliness. Eisenberger et al. [6] have shown a causal connection between experimentally induced inflammation and feelings of social disconnection, supporting the idea of the co-regulation of inflammatory processes and social behavior. Loneliness is related to an adaptive enhancement of inflammation because increased inflammation prepares lonely or disconnected individuals for an increased likelihood of being in a vulnerable state such as predation, injury, or infection. This is supported by findings showing higher basal levels of IL-6 in lonelier adults (Zilioli and Jiang, 2021).
Interventions Altering Inflammatory Processes
Psychological Interventions
It is now widely recognized that dysregulation of inflammatory processes is an important factor contributing to the morbidity associated with a large number of disease conditions [7]. Interventions with psychological dimensions that mitigate inflammatory processes are based on two approaches. The first approach is through mind-body therapies (MBTs) such as Tai Chi (TC), Qigong (QG), yoga (YA), and meditation (MED), which emphasize the use of the mind together with the body to facilitate healing [8]. The second is through psychological interventions. Physical elements can be included in these interventions, but to be classified as psychological interventions, they must be composed of more than 50% elements that have an explicit psychological aim, as in cognitive behavioral therapy, mindfulness-based therapy, or guided imagery. O’Toole et al. [9] reviewed 19 randomized controlled trials (RCTs) of meditation- or mindfulness-based interventions (MBIs). The effect size for combined pro-inflammatory outcomes was small but significant (K = 17, g = 0.15, p = 0.009).
Mind-body Interventions
One meta-analysis [10] and several systematic reviews [8,11,12] have been undertaken to determine the effect of MBTs such as TC, QG, MED, and YA on inflammation. Morgan et al. [10] summarized the results of 34 studies on MBTs and found a moderate effect size for CRP (K = 9, g = 0.58, I2 = 97%) and a small effect size for IL-6 (K = 10, g = 0.35, I2 = 83%). The substantial heterogeneity found between studies was probably due to the diversity of the interventions used. The effects of MBT on other pro-inflammatory markers such as TNF and IL-8 were not significant. Unfortunately, the meta-analysis did not examine or compare the effect sizes of individual MBTs. However, recent meta-analytic reviews have shown limitations in the effectiveness of MBTs such as TC and QG in reducing inflammation [13].
The effectiveness of YA in reducing inflammatory markers was not evaluated separately by Morgan et al. [10], so the question of whether YA is more effective than other MBTs in reducing systemic inflammation remains to be answered. Recent evidence suggests that YA promotes parasympathetic activation reflected by heart rate variability (reviewed by Zou et al., [14]). Parasympathetic activation was shown to have an anti-inflammatory effect by Sloan and Cole (2021). The review of available evidence suggests that YA may be more effective in reducing systemic inflammation than other MBTs. Evidence from a systematic review of 15 RCTs supports previous findings on the efficacy of YA in reducing levels of proinflammatory markers including IL-1, IL-6, and TNFα [12]. Another systematic review of 15 studies reported an attenuating effect of YA on inflammatory markers such as CRP, IL-6, and TNF in eleven of the included studies [11]. It was also found that interventions with a physical activity component such as YA were more effective in reducing CRP than meditation [8].
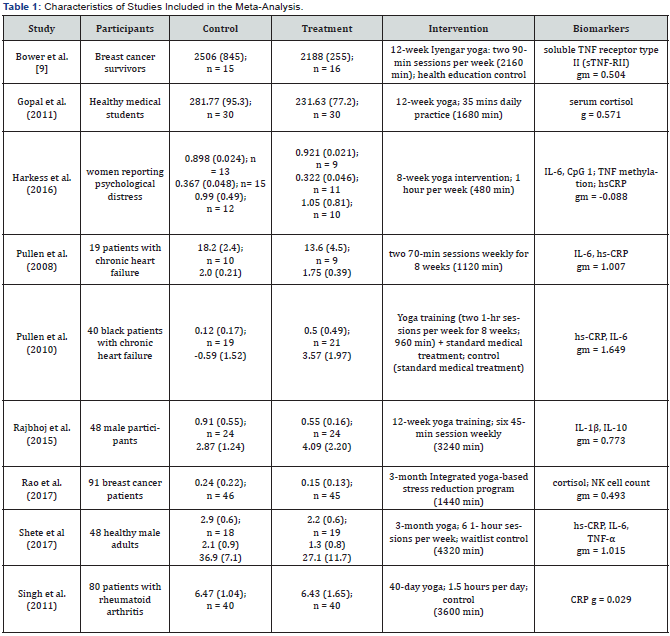
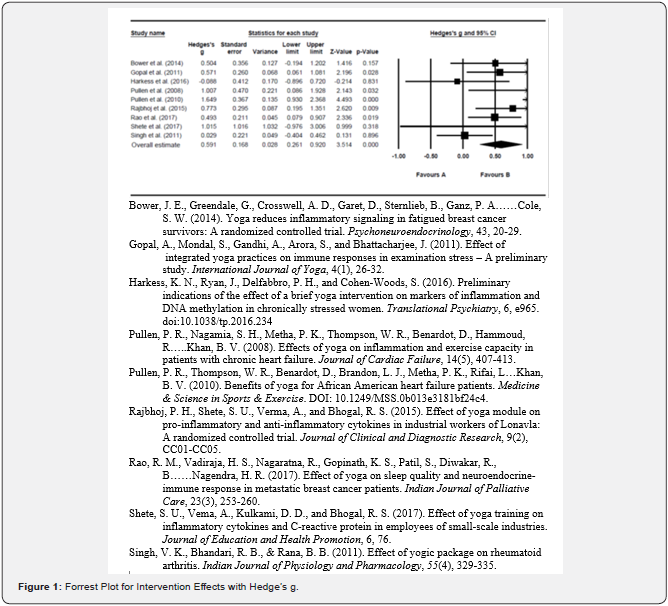
To evaluate the effect of YA on inflammatory markers quantitatively, information from 11 relevant studies examined in recent reviews or meta-analyses on MBTs (e.g. [8,10-12] was extracted to derive a combined effect size. The effect size was determined from the standardized mean difference (Hedge’s g) in biomarker levels post-intervention between the YA and control groups. Nine studies with sufficient information to compute the effect size were included in the meta-analysis (Table 1). All analyses were undertaken using
Comprehensive Meta-Analysis software version 3 (Biostat, Inc.). The effect sizes associated with multiple biomarkers from a single study were combined into a single effect size (Rosenthal, 1991) so that each of the 9 studies has one single effect size for subsequent analyses. As shown in Figure 1, the combined effect size was g = 0.59 (CI [0.26 – 0.92], p < .001) based on random models, implying a moderate and significant reduction in inflammation in the YA group. The heterogeneity was moderate, with statistical parameters showing I2 = 57.17%, Q(8) = 18.68, p = 0.017. No publication bias in the study was found according to Egger’s test, t(7) = 1.07, p = 0.32. The effect size of 0.59 is greater than that associated with MBTs (gs = 0.58 and 0.35, Morgan et al., [10]) and that associated with psychological interventions (g = 0.15, O’Toole et al., [9]). Despite the limitations of this meta-analysis, the findings support earlier evidence suggesting that YA is more effective in decreasing inflammatory processes than other MBTs such as TC and QG. In addition, the demonstrated effects of YA on reducing systemic inflammation seem to compensate for the accentuated nonspecific immunity that characterizes the lonely phenotype.
Conclusion
The preceding analysis has pointed to yoga as an effective form of MBT to improve systemic inflammation, especially when yoga is compared to conventional or mindfulness-based psychotherapies. Due to the close connection between enhanced inflammation and the lonely phenotype, it has also been argued from a psychoneuroimmunological perspective that yoga is particularly effective in reducing loneliness via its anti-inflammatory effect. This has important implications for the literature on loneliness intervention studies which hitherto has been dominated by social-skill training and the unsound idea that a lack of social interactions causes loneliness.
In conclusion, I have provided a theoretical and empirical basis to explain how yoga leads to reduced loneliness and better health via its “anti-inflammatory” effect. This should hopefully stimulate further research leading to a better understanding of the psychobiological mechanisms underpinning the health effects of yoga. Given that loneliness (1) is one of the important upstream factors associated with increased morbidity, and (2) is prevalent in the older population [15], public health policymakers should consider promoting yoga as a crucial component in lifestyle interventions, particularly in aging societies [16].
References
- Hawkley LC (2022) Loneliness and health. Nature Rev Dis Primers 8(1): 22.
- Masi CM, Chen HY, Hawkley LC, Cacioppo JT (2011) A meta-analysis of interventions to reduce loneliness. Personal and Social Psychol Rev 15(3): 219-226.
- Lai JCL, Lee DYH, Leung MOY, Lam YW (2019) Daily hassles, loneliness, and diurnal salivary cortisol in emerging adults. Hormone Behav 115: 104558.
- Cole SW, Capitanio JP, Chun K, Arevalo JMG, Ma J, Cacioppo JT (2015) Myeloid differentiation architecture of leukocyte transcriptome dynamics in perceived social isolation. PNAS 112(49): 15142-15147.
- Maier SF, Watkins LR (1998) Cytokines for psychologists: Implications of bidirectional immune-to-brain communication for understanding behavior, mood, and cognition. Psychol Rev 105(1): 83-107.
- Eisenberger NI, Inagaki TK, Mashal NM, Irwin MR (2010) Inflammation and social experience: An inflammatory challenge induces feelings of social disconnection in addition to depressed mood. Brain Behav Immun 24(4): 558-563.
- Slavich GM (2015) Understanding inflammation, its regulation, and relevance for health: A top scientific and public priority. Brain Behav Immunity 45: 13-14.
- Bower JE, Irwin MR (2016) Mind-body therapies and control of inflammatory biology: A descriptive review. Brain Behav Immun 51: 1-11.
- O’Toole MS, Bovbjerg DH, Renna ME, Lekander M, Mennin DS, et al. (2018) Effects of psychological interventions on systemic levels of inflammatory biomarkers in humans: A systematic review and meta-analysis. Brain, Behav Immun 74: 68-78.
- Morgan N, Irwin MR, Chung M, Wang C (2014) The effects of mind-body therapies on the immune system: Meta-analysis. Plos One 9(7): e100903.
- Djalilova DM, Schulz PS, Berger AM, Case AJ, Kupzky KA, et al. (2019) Impact of yoga on inflammatory biomarkers: A systematic review. Biol Res Nurs 21(2): 198-209.
- Falkenberg RI, Eising C, Peters ML (2018) Yoga and immune system functioning: A systematic review of randomized controlled trials. J Behav Med 41: 467-482.
- Oh B, Bae K, Lamoury G, Eade T, Boyle F, et al. (2020) The effects of Tai Chi and Qigong on immune responses: A systematic review and meta- analysis. Medicines 7: 39.
- Zou L, Sasaki JE, Wei G, Huang T, Yeung AS, et al. (2018) Effects of mind-body exercises (Tai Chi/Yoga) on heart rate variability parameters and perceived stress: A systematic review with meta-analysis of randomized controlled trials. J Clin Med 7(11): 404.
- Chawla K, Kunonga TP, Stow D, Barker R, Craig D, et al. (2021) Prevalence of loneliness amongst older people in high-income countries: A systematic review and meta-analysis. Plos One 16(7): e0255088.
- Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, et al. (2017) An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 152: 157-171.






























