Adding Virtual Reality Pain Neuroscience Education to Usual Care for Chronic Low Back Pain: An Exploratory Study
David Boyce1, Daniel Stopher2,3 and Adriaan Louw3*
1Hanover College, Doctor of Physical Therapy Program, USA
2ProRehab Physical Therapy, USA
3Evidence in Motion, Pain Science, USA
Submission:June 18, 2024;Published: July 02, 2024
*Corresponding author: Adriaan Louw, PT, PhD, Evidence in Motion, 605 Pennsylvania Ave, Story City, IA, USA
How to cite this article: Boyce D, Stopher D, Louw A. Adding Virtual Reality Pain Neuroscience Education to Usual Care for Chronic Low Back Pain: An Exploratory Study. J Yoga & Physio. 2024; 11(4): 555817 DOI:10.19080/JYP.2024.11.555817
Abstract
Introduction: Evidence supports adding cognitive and behavioral treatments such as pain neuroscience education (PNE) for chronic low back pain (CLBP). Advances in digital therapeutics, adding technology is being explored to determine its ability to add clinical benefit and foster greater independence for patients. This exploratory study tested if adding PNE virtual reality (PNE-VR) to usual care (UC) physical therapy (PT) for CLBP added benefits.
Materials and Methods: Thirty patients presenting to PT with CLBP were randomly allocated to receive UC PT or PNE-VR plus UC for CLBP. UC was based on the most recent practice guidelines for CLBP, focusing on manual therapy, trunk coordination, directional preference exercises, progressive endurance exercises, and fitness activities. PNE-VR consisted of a virtual reality experience of pain metaphors (5-7 minutes) explaining persistent pain, spreading pain, pain with stress/temperature changes, fatigue, sleep disturbance, and focus and concentration deficits. PNE-VR additionally added breathing exercises and mindfulness exercises following PNE. Patients attended PT twice a week for three weeks and initial measurements included Oswestry Disability Index (ODI), pain catastrophization scale (PCS), and self-reported pain – numeric pain rating scale (NPRS). At each visit, NPRS was measured, and after visits three and six, a global rating of change (GROC) scale was administered. After six visits, the ODI, PCS, NPRS. and GROC was repeated.
Results: PNE-VR added to UC yielded superior results to UC for CLBP for self-reported pain (p = 0.04), exceeding minimal clinical important difference (MCID) for the PNE-VR group. Patient satisfaction did not reach statistical significance (p = 0.10) between the two groups, but the PNE-VR group’s difference exceeded MCID for the GROC, and the UC group did not. No differences between groups were found for ODI (p = 0.27) or PCS (p = 0.14). Prior to treatment, three UC patients and seven PNE-VR patients exceeded the cut-off score of a high PCS (>30). Following treatment, only one UC patient moved below the high PCS cut-off score, whereas five PNE-VR group patients moved below the cut-off score.
Conclusion: Adding PNE-VR to UC yielded potential benefits over UC for CLBP, including self-reported pain and patient satisfaction. No added benefit was found regarding disability and pain catastrophizing. Future and larger-scale studies should explore the addition of digital therapeutics to UC to add additional patient benefits from PT.
Keywords: Pain Neuroscience Education; Virtual Reality; Chronic Low Back Pain; Physical Therapy; Digital Therapeutics
Abbreviations: CLBP: Chronic Low Back Pain; GROC: Global Rating of Change; MCID: Minimal Clinical Important Difference; MDC: Minimal Detectable Change; NPRS: Numeric Pain Rating Scale; ODI: Oswestry Disability Index; PCS: Pain Catastrophization Scale; PNE: Pain Neuroscience Education; PNE-VR: Pain Neuroscience Education Virtual Reality; PT: Physical Therapy; UC: Usual Care; US: United States
Introduction
It is well reported that low back pain is the most common musculoskeletal disorder in the world, leading to high rates of pain and disability, especially chronic low back pain (CLBP) [1]. It is reported that approximately one in three patients with low back pain develop CLBP, with symptoms present one year later [2]. CLBP is a major global issue as it has been shown to be the leading cause of disability and healthcare costs [3]. On a clinical level, CLBP is a challenge for healthcare providers, with data showing that 80-90% of patients with low back often being diagnosed with “non-specific” low back pain, adding little to no additional clinical guidance for diagnosis, treatment, clinical pathways, risk factors, etc. [4].
With the enormous burden of CLBP, clinicians often find themselves in a precarious position trying to seek the optimal treatment plan to ease the patient’s pain and disability and additionally lessen the impact of CLBP on society [5]. Given the complexities of diagnosis, the individual nature of each person’s pain experience, co-morbid psycho-social factors, it remains a clinical challenge to treat CLBP [1,6,7]. One way to help clinicians is the use of high-level evidence (i.e., systematic reviews and metaanalyses), as well as the development of practice guidelines using the current best evidence. The most recent practice guideline in physical therapy (PT) was published in 2021 [8]. Specific to CLBP, it was recommended (A-level evidence, supported by systematic reviews, meta-analyses, and high-quality randomized clinical trials) that a multi-modal treatment approach consisting of different forms of exercise, manual therapy, and education be used [8]. Regarding exercise, therapists were advised to use general exercise training, muscle strengthening, endurance training, specific trunk muscle activation, aerobic exercise, and aquatic exercises [9]. Active, self-help treatments such as yoga, stretching, Pilates, and strength training were recommended to encourage movement and foster independence. The heavy focus on exercise and movement aligns with one of the pillars of the current best-evidence approach for treating chronic pain. Another recommendation was manual therapy, be it thrust or non-thrust joint mobilization, underpinning the need for care by a skilled clinician [10]. The final recommendation was the use of pain neuroscience education (PNE). PNE teaches patients more about the underlying biology and physiology of their nervous system during a pain experience, allowing for a greater understanding of the sensitization of the nervous system, which impacts their pain perception, movement, and outlook on recovery [11]. Current evidence shows that PNE, specifically in chronic pain, decreases self-reported pain levels, disability, fear avoidance, and pain catastrophizing, allowing patients to move more, which is tied to the aforementioned key pillar of treating CLBP [12,13]. Furthermore, the guidelines and evidence support the use of PNE as a multi-modal intervention alongside exercise and manual therapy versus stand-alone treatment [8, 12, 14].
Even though the current evidence provides clinicians with guidelines, various clinical barriers remain. Chronic pain is complex, and patients often present with various levels of complexity, including higher levels of fear, catastrophizing, and depression [6,15]. The sensitization of the nervous system fluctuates which impacts clinicians’ ability to progress exercises as planned. Clinicians need a variety of skill sets to help patients with CLBP, including the ability to instruct them in various forms of exercise, perform manual therapy, deliver PNE, etc. [8]. Added to this are the ever-increasing demands of productivity, often resulting in more patient visits, shorter treatment sessions, and protracted plans of care. In 2009, Deutscher and colleagues reported that the mean duration of a PT visit for low back pain was around 30 minutes, highlighting the significant challenge CLBP poses for clinicians [16]. An emerging trend in PT, driven by advances in technology and the recent shift in telehealth during the coronavirus pandemic, is the use of digital therapeutics [17,18].
Digital Therapeutics are evidence-based therapeutic interventions driven by software to prevent, manage, or treat a medical disorder or disease [17]. With the advent of virtual reality (VR), augmented reality, wearable technology, fitness trackers, pain applications, and more, clinics and clinicians are looking to see if these may help with complex conditions such as CLBP [18]. This model proposes using these digital therapeutics as PT extenders versus PT replacements [19]. Embracing the technological advances, a clinician can focus their available time on physical treatments (i.e., exercises and manual therapy), whereas digital platforms can be used to deliver other complementary treatments to calm the nervous system, including PNE, breathing, relaxation, mindfulness-based stress reduction, and more [19,20]. This allows for a more robust clinical session combining these treatments in one session and possibly allows for home use, fostering independence. To date, very little is known or published in this realm. The purpose of this study was to determine if the addition of PNE, delivered via VR, added any additional benefits to patients seeking PT care for CLBP.
Methods
Design
The study was designed as a randomized clinical trial. Before the study, institutional review board approval was obtained from Bellarmine University. All procedures followed were in accordance with the ethical standards according to the Helsinki Declaration of 1975, as revised in 1983. Participation in the study was entirely voluntary, and patients had to sign a written consent.
Patients
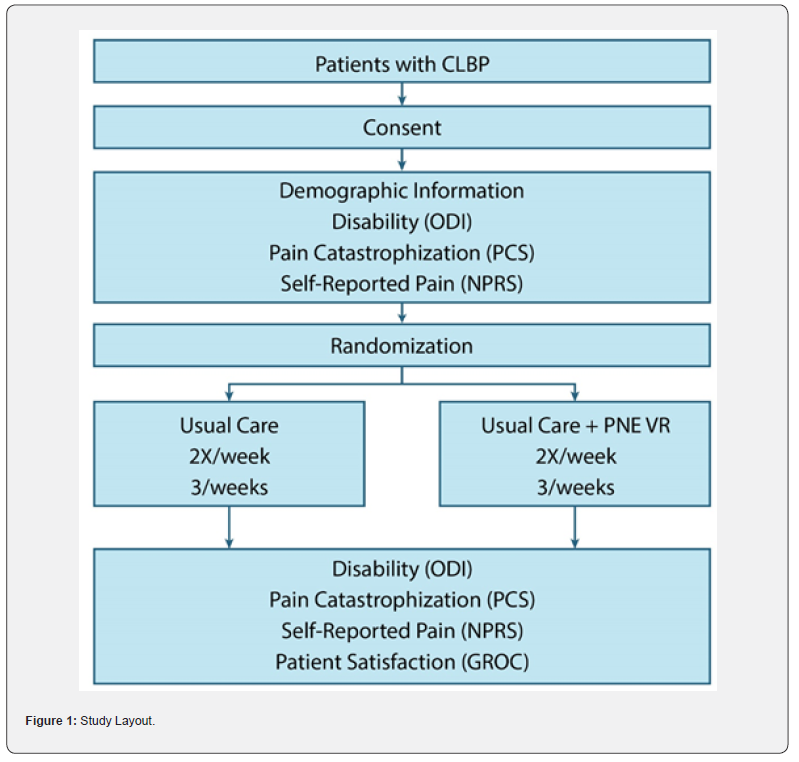
Patients attending PT for CLBP were invited to participate in the study. Data collection occurred at nine clinics specializing in the assessment and treatment of CLBP and the delivery of usual care (UC) per current practice guidelines, as well as PNE via VR (PNE-VR) (Figure 1) [20]. Inclusion criteria were adults (18 and older), present with CLBP (> 3 months) to PT for assessment and treatment, proficient in the English language, no precautions or contraindications specific for VR (i.e., pre-existing binocular vision abnormalities or seizures), no red flags for PT in general and consenting to the study.
Instruments
Upon consent, patient demographics were gathered to
describe the cohort, including age and gender. Before treatment
(visit 1), a series of outcome measures were obtained:
Self-Reported LBP (Numeric Pain Rating Scale - NPRS):
The NPRS is a standard self-reported pain rating scale for
numerous musculoskeletal conditions [21-23]. The minimal
clinical important difference (MCID) for the NPRS for CLBP is
reported as a reduction of 1.7 points [24].
Disability (Oswestry Disability Index - ODI): The ODI is a
validated, extensively utilized questionnaire for people who suffer
from low back pain. It consists of 10 items representing different
health constructs (i.e., pain intensity, physical functioning, sleep
functioning, and social functioning). Each section is scored on
a 0 to 5 rating scale, where zero means ‘No pain’ and 5 means
‘Worst imaginable pain.’ The total score of the ODI is calculated by
adding all scores of applicable items, dividing the obtained score
by the maximal total score, and multiplying the result by 100 to
get a percentage score [25]. The higher the score, the higher the
patient-determined disability [25,26].
Pain Catastrophizing (Pain Catastrophization Scale - PCS):
The PCS is a self-report questionnaire that assesses inappropriate
coping strategies and catastrophic thinking about pain and injury.
The PCS has been used in previous musculoskeletal studies [27,28] and demonstrated strong construct validity, reliability, and stability [29]. The PCS utilizes a 13-item, 5-point Likert scale with higher scores indicating elevated levels of catastrophizing. Previous studies using the PCS have shown a median score of 18 in healthy individuals, and a score over 30 is reported as a high level of pain catastrophization [29]. In patients with musculoskeletal pain, the PCS’s minimal detectable change (MDC) is reported to be 9.1 [30], and the MCID has not been established.
Patient self-reported experience following the UC and UC plus PNE-VR was measured after the 3rd visit and final visit, using the Global Rate of Change (GROC) scale. The GROC is a scale that measures self-perceived change in health status. The primary purpose was to quantify the extent to which a patient has improved or deteriorated over time. The GROC scale involves a single question for the patient to rate their change concerning a particular condition over a specified period. The scale used is -7 (a very great deal worse) to 7 (A very great deal better). The MCID for the GROC for chronic musculoskeletal pain has been reported as a change of 2.0 [31].
Intervention
The PNE-VR session was designed to be delivered after a patient’s planned PT session, thus not interfering with their current treatment plan [19]. UC focused on the current practice guidelines with a focus on manual therapy, trunk coordination, directional preference exercises, progressive endurance exercise and fitness activities [8]. At the completion of their normal oneon- one session with the attending PT, patients were placed in a private treatment room for the PNE-VR session. The PNE-VR was delivered using a headset and earphones while a patient was seated in a comfortable chair [19, 20]. Patients were familiarized with the VR headset, navigating the VR dashboard the subject sees in the headset, and how to access each of the sessions utilizing a hand-held activator. The PNE-VR sessions were uploaded via a wireless signal to the headset and the subject used a hand-held activator to start, navigate and end their PNE session. The PT was not in the room during the PNE-VR. The software tracked the subject throughout the sessions, ensuring they fully complete each session. The VR system provides a total 360-degree immersion, including sound, to provide a true sensory virtual environment. The total of the PNE-VR treatment session was 12 minutes to limit prolonged VR exposure and mimic typical in-person therapist-led PNE [32,33]. The content of the PNE-VR is in line with current oneon- one, clinician-led PNE research [12,32]. The PNE-VR session included an introduction to PNE (1 minute), an introduction to the nervous system (3 minutes), a metaphor of the sensitive alarm system to educate patients on hyperalgesia and allodynia (2 minutes) [32], a metaphor of the “nosy” neighbor to educate patients about spreading pain as a consequence of a sensitized nervous system (2 minutes), and strategies used to calm down a sensitized nervous system non-pharmacologically (4 minutes) (Figure 1).
Analysis
Upon completion of the study, participant intake forms from pre- and post-intervention were collected for analysis. There was no attrition during the study and all participants were accounted for in post-treatment analysis. Demographic data was calculated to be reported in means, standard deviations, percentages and total numbers. Paired, two-sample t-tests were used to calculate if there were significant differences between the groups for CLBP, disability and PCS scores. A predefined significance level of a = 0.05 was used in this study for all analyses. Additionally, count data was generated to examine the proportion of the study sample who achieved either MDC or MCID.
Results
Patients
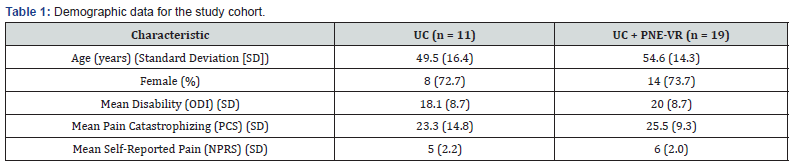
Thirty patients completed the trial with eleven assigned to UC, and 19 to UC plus PNE-VR (Table 1). At the start of the study, no significant differences between the groups were present in regard to age (p = 0.41), disability (p = 0.51), pain catastrophization (p = 0.66) and self-reported pain (p = 0.16).
Back Pain
Following treatment, UC plus PNE-VR yielded a significant (p = 0.04) greater improvement in pain than UC. As a whole, the UC plus PNE-VR group’s improvement over 6 sessions met the MCID for CLBP, while the UC group did not (Figure 2). In the UC group, 18% of the patients met or exceeded the MCID for CLBP, while 47% of the patients in the UC plus PNE-VR group met or exceeded the MCID.
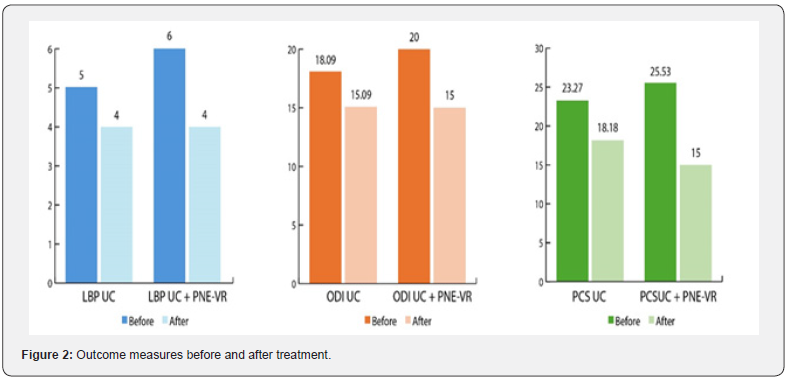
Disability
There was no significant difference in improvement of ODI between the two groups at the end of the 6 therapy sessions (p = 0.27) (Figure 2). In the UC group, 36% of the patients improved their ODI beyond minimal detectable change (MDC), while 47% of the UC plus PNE-VR group improved their ODI beyond MDC.
Pain Catastrophizing
There was no significant difference in improvement of PCS between the two groups at the end of the 6 therapy sessions (p = 0.14) (Figure 2). In the UC group, 27% of the patients improved their PCS beyond MDC, while 58% of the UC plus PNE-VR group improved their PCS beyond MDC. Prior to treatment, 3 patients in the UC group exceeded the cut-off score of a high PCS (>30) and following treatment, 2 remained above the cut-off score. For the UC plus PNE-VR group, there were 7 patients above the cut-off prior to treatment and only 2 at the end of the treatment.
Patient Satisfaction
After 3 visits, the mean GROC score for both groups did not meet or exceed the MCID and was not different between the two groups (p = 0.35). After 6 visits, the mean GROC score for the UC group once again did not meet/exceed the MCID, but the UC plus PNE-VR group did. There was no significant difference between the 2 groups at 6 visits (p = 0.10). After 6 visits, 27% of the UC group met or exceeded the MCID for the GROC, while 63% of the UC plus PNE-VR group met or exceeded the MCID.
Discussion
To our knowledge, this is the first study to report on the difference between UC PT for CLBP, and the addition of PNE-VR to UC for CLBP. The addition of PNE-VR to UC yielded potential added benefits over UC for CLBP, including self-reported pain and patient satisfaction. No added benefit was found regarding disability and pain catastrophizing.
The addition of PNE-VR to UC yielded meaningful shifts to self-reported CLBP. The combination of PNE with UC, consisting mainly of various forms of exercise and movement, aligns with current practice guidelines [8]. Additionally, the results concur with the evidence that shows PNE as a stand-alone treatment is not effective, but the combination of PNE and exercise/movement (PNE+) is very beneficial for patients experiencing chronic pain, including CLBP [14,34]. Conversely, the results show that UC alone, focusing only on exercise/movement, without a cognitive intervention, is limited in its ability to create a meaningful shift, underscoring the importance of a multi-modal approach. This decrease in self-reported pain with the use of PNE-VR concurs with a previous PNE-VR case study of chronic whiplash associated disorder and case series of back, neck, knee and shoulder pain, showing a reduction on self-reported pain [19,20].
The fact that the PNE-VR session was an “add-on” treatment, after UC, fuels the belief that digital therapeutic strategies such as this may indeed allow for a more robust therapeutic experience. In this study, if the Deutscher, et. al study is used as an example, patients with UC received approximately 30 minutes of PT, whereas the addition of the PNE-VR, allowed for a more robust, extended session (approximately 45 minutes), which not only yielded superior results regarding self-reported pain, but also achieved higher patient satisfaction [19]. This is an important finding, since it’s well documented that patients with chronic pain feel mistreated and misunderstood by the medical system [35]. The PNE-VR addition to UC yielded a larger positive patient experience, compared to UC, which is a positive step for people struggling with chronic pain. Even though the study did not explore which part - content, added time, advanced technology, etc., yielded the positive change, the results show the addition of PNE, use of VR and extending a normal PT session is welcomed by the patients. By adding more beneficial treatments, without adding more burden to the healthcare provider, digital therapeutics could bridge the gap between patient needs, provider capacity and the time-constraints of clinical practice [19].
In this study, the addition of PNE-VR did not alter pain catastrophizing over the UC group. This result was surprising since current best-evidence for PNE shows robust shifts in PCS scores, and it’s been postulated that high PCS scores are often predictive of success with the use of PNE [12,13]. Even though there was no significant difference in PCS scores between the groups, it is important to note that the PNE-VR shifted more patients below the cut-off score for a high PCS, indicative of reduced ability to return to work [29]. Similarly, the results show no meaningful difference between the UC group and PNE-VR group for disability. This result once again is contrary to current evidence showing PNE’s ability to positively influence disability [12,13]. These differences related to pain catastrophizing and disability may be attributed to the delivery methods, using VR. PNE delivery entails the use of metaphors, examples and pictures, often done by a clinical as a one-on-one intervention, or in group settings [12,32]. These have been explored extensively, whereas the use of digital therapeutics has not, including the use of VR. To date, most VR treatments for pain have centered on distraction techniques, addition of techniques to calm the nervous system (i.e., breathing and relaxation), or more recently as part of graded motor imagery to influence structural changes in the brain [36- 38]. The delivery of a cognitive intervention via VR for pain is new and these results imply researchers should further study if VR is the most appropriate modality for use in the delivery of PNE in the digital therapeutic space. Additionally, the VR delivery of PNE does not allow for the typical ability of patients to ask questions, or clarify information, which is a cornerstone of the delivery of PNE by a clinician, be it one-on-one or in groups [32,35]. Given the fact that PNE-VR did shift self-reported pain and yielded a positive patient experience, the results may also indicate a potential subgroup of patients with CLBP that may do well with PNE delivered via VR. Future studies should explore what patients do well with VR.
Conclusion
The addition of PNE-VR to UC yielded potential added benefits over UC for CLBP, including self-reported pain and patient satisfaction. No added benefit was found regarding disability and pain catastrophizing. Future and larger scale studies should explore the addition of digital therapeutics to UC to add additional patient benefits from PT.
Acknowledgements
The authors would like to acknowledge the clinicians at Pro Rehab Louisville, KY, and the Bellarmine University DPT students involved in the development, data collection, and treatment: Jason Walsh PT, DPT, COMT; Riley Sturzebecher PT, DPT; Adam Campbell PT, DPT; Jessica Hetzer PT, DPT, OCS; Dale Boren Jr. PT, MPT, OCS, ASTYM cert.; Adam Fatkin PT, DPT; Brittany Thompson PT, DPT, TPS, LSMC, and Jill Stump PT, DPT, OCS, Kam Meehan SPT, Raaj Patel SPT, Jared Simpson SPT, Alexis Walsh SPT.
References
- Nijs J, Eva K, Alessandro C, Chad C, Lieven AD, et al. (2024) Nociceptive, neuropathic, or nociplastic low back pain? The low back pain phenotyping (BACPAP) consortium's international and multidisciplinary consensus recommendations. Lancet Rheumatol 6(3): e178-e188.
- Luciola da CMC, Christopher GM, Mark JH, James HM, Robert DH, et al. (2012) The prognosis of acute and persistent low-back pain: a meta-analysis. CMAJ 184(11): E613-624.
- Collaborators GBDLB (2023) Global, regional, and national burden of low back pain, 1990-2020, its attributable risk factors, and projections to 2050: a systematic analysis of the Global Burden of Disease Study. Lancet Rheumatol 5(6): e316-e329.
- Chiarotto A, Koes BW (2022) Nonspecific Low Back Pain. N Engl J Med 386(18): 1732-1740.
- Latimer J, Maher C, Refshauge K (2004) The attitudes and beliefs of physiotherapy students to chronic back pain. Clin J Pain 20(1): 45-50.
- Zimney K, Van Bogaert W, Louw A (2023) The Biology of Chronic Pain and Its Implications for Pain Neuroscience Education: State of the Art. J Clin Med 12(13): 4199.
- Cook CE, Rhon DI, Bialosky J, Donaldson M, George SZ (2023) Developing Manual Therapy Frameworks for Dedicated Pain Mechanisms. JOSPT Open 1(1): 1-16.
- George SZ, Julie MF, Sheri PS, Michael JS, Jason MB, et al. (2021) Interventions for the Management of Acute and Chronic Low Back Pain: Revision 2021. J Orthop Sports Phys Ther 51(11): CPG1-CPG60.
- Naugle KM, Fillingim RB, Riley JL (2012) A meta-analytic review of the hypoalgesic effects of exercise. The journal of pain : official journal of the American Pain Society 13(12): 1139-1150.
- Bond BM, Chris DK, Adam WY, Wen L (2020) Effect of spinal manipulative therapy on mechanical pain sensitivity in patients with chronic nonspecific low back pain: a pilot randomized, controlled trial. J Man Manip Ther 28(1): 15-27.
- Moseley GL, Hodges PW, Nicholas MK (2004) A randomized controlled trial of intensive neurophysiology education in chronic low back pain. Clin J Pain 20(5): 324-330.
- Louw A, Kory Z, Emilio JP, Ina D (2016) The Efficacy of Therapeutic Neuroscience Education on Musculoskeletal Pain – A Systematic Review of the Literature. Physiotherapy Theory and Practice 32(5): 332-355.
- Siddall B, Adrian R, Matthew DJ, John B, Diana P, et al. (2021) Short-term impact of combining pain neuroscience education with exercise for chronic musculoskeletal pain: a systematic review and meta-analysis. Pain 163(1): e20-e30.
- Louw A, Kathleen AS, Jo N, Carol AC, Kory Z (2021) Revisiting the Provision of Pain Neuroscience Education: An Adjunct Intervention for Patients but a Primary Focus of Clinician Education. J Orthop Sports Phys Ther 51(2): 57-59.
- Louw AKF, Brennan J, Rulis A, Mendoza G, Louw H, et al. (2021) Depression and patients attending outpatient physical therapy with musculoskeletal pain and disability. MOJ Orthop Rheumatol 13(6): 126-129.
- Deutscher D, Susan DH, Ruth D, Dennis LH, Randall JS, et al. (2009) Associations between treatment processes, patient characteristics, and outcomes in outpatient physical therapy practice. Arch Phys Med Rehabil 90(8): 1349-1363.
- Phan P, Mitragotri S, Zhao Z (2023) Digital therapeutics in the clinic. Bioeng Transl Med 8(4): e10536.
- Rohaj A, Bulaj G (2023) Digital Therapeutics (DTx) Expand Multimodal Treatment Options for Chronic Low Back Pain: The Nexus of Precision Medicine, Patient Education, and Public Health. Healthcare (Basel) 11(10): 1469.
- Louw A, Zimney K, Stopher D, Saldanha KG, Shockley J, et al. (2022) Pain Neuroscience Education Delivered Through Virtual Reality for Common Musculoskeletal Conditions Seen in Physical Therapy: An Exploratory Study. Rep Global Health Res 6(2): 1-12.
- Louw A, Louw C, Flynn T (2019) Case report: Pain Neuroscience Education using Virtual Reality. Pain and Rehabil 46: 4-7.
- Moseley GL (2003) Joining forces - combining cognition-targeted motor control training with group or individual pain physiology education: a successful treatment for chronic low back pain. J Man Manip Therap 11(2): 88-94.
- Moseley L (2002) Combined physiotherapy and education is efficacious for chronic low back pain. Aust J Physiother 48(4): 297-302.
- Moseley GL (2005) Widespread brain activity during an abdominal task markedly reduced after pain physiology education: fMRI evaluation of a single patient with chronic low back pain. Aust J Physiother 51(1): 49-52.
- Farrar JT, James PY, Linda L, John LW, Michael RP (2001) Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 94(2): 149-158.
- Fairbank JC, Pynsent PB (2000) The Oswestry disability index. Spine 25(22): 2940-2953.
- Sheahan PJ, Nelson-Wong EJ, Fischer SL (2015) A review of culturally adapted versions of the Oswestry Disability Index: the adaptation process, construct validity, test-retest reliability and internal consistency. Disabil Rehabil 37(25): 2367-2374.
- Moseley GL, Nicholas MK, Hodges PW (2004) A randomized controlled trial of intensive neurophysiology education in chronic low back pain. Clin J Pain 20(5): 324-30.
- Moseley GL (2004) Evidence for a direct relationship between cognitive and physical change during an education intervention in people with chronic low back pain. Eur J Pain 8(1): 39-45.
- Sullivan MJL, Bishop SR, Pivik J (1995) The Pain Catastrophizing Scale: Development and validation. Psychological Assessment 7(4): 524-532.
- George SZ, Valencia C, Beneciuk JM (2010) A psychometric investigation of fear-avoidance model measures in patients with chronic low back pain. J Orthop Sports Phys Ther 40(4): 197-205.
- Kamper SJ, Maher CJ, Mackay G (2009) Global rating of change scales: a review of strengths and weaknesses and considerations for design. J Manual Manipulative Ther 17(3): 163-170.
- Louw A, Kory Z, Christine O, Sandra H (2016) The clinical application of teaching people about pain. Physiotherapy Theory and Practice 32(5): 385-395.
- Louw A, Kevin F, Breanna C, Brooke F, Grace L, et al. (2019) Immediate effect of pain neuroscience education for recent onset low back pain: an exploratory single arm trial. J Man Manip Ther 27(5): 267-276.
- Wood L, Hendrick PA (2019) A systematic review and meta-analysis of pain neuroscience education for chronic low back pain: Short-and long-term outcomes of pain and disability. Eur J Pain 23(2): 234-249.
- Zimney KJ, Emilio P, Morey JK, Adriaan L, et al. (2022) The relationship between trust and outcomes during physical therapy care for chronic low back pain. Physiother Theory Pract 40(6): 1164-1171.
- Patterson DR, Hunter GH, Gloria C, Devon B, Harley HH, et al. (2021) Hypnotic Enhancement of Virtual Reality Distraction Analgesia during Thermal Pain: A Randomized Trial. Int J Clin Exp Hypn 69(2): 225-245.
- Hoffman HG, David RP, Robert AR, Raquel P, Wanda B, et al. (2020) Virtual Reality Analgesia for Children With Large Severe Burn Wounds During Burn Wound Debridement. Front Virtual Real 1: 602299.
- Hoffman HG, David AB, Eric R, Christelle K, Sylvie L, et al. (2020) Virtual reality hand therapy: A new tool for nonopioid analgesia for acute procedural pain, hand rehabilitation, and VR embodiment therapy for phantom limb pain. J Hand Ther 33(2): 254-262.






























