Immediate Effects of a Brief 10-Minute Mindfulness-Based Stress Reduction Body Scan for Central Sensitization: A Case Series
Jessica McConahay1, Debra Rico2,5, Jessica Podolak3,5, Hailey Louw4 and Adriaan Louw5*
1 Whole Body Health Physical Therapy, USA
2 Rockhurst University, USA
3 Phileo Health, LLC, USA
4 University of Wisconsin, USA
5 Evidence in Motion, USA
Submission: April 21, 2023; Published: May 10, 2023
*Corresponding author: Adriaan Louw, Evidence in Motion, USA
How to cite this article: Jessica M, Debra R, Jessica P, Hailey L, Adriaan L. Immediate Effects of a Brief 10-Minute Mindfulness-Based Stress Reduction Body Scan for Central Sensitization: A Case Series. J Yoga & Physio. 2023; 10(3): 555789. DOI:10.19080/JYP.2023.10.555789
Abstract
Introduction: Chronic pain is often challenging to treat due to changes associated with central sensitization. Mindfulness practices have been shown to impact pain through a non-judgmental appraisal of physical sensations. This case series aimed to determine if a 10-minute body scan meditation would positively impact a person who suffers from central sensitization.
Materials and Methods: Sixteen participants were guided through a 10-minute body scan meditation. Pre- and post-treatment measures included self-reported pain rating, pain pressure threshold, and a body pain diagram. The global rate of change was also assessed following treatment.
Results: Overall, self-reported pain was reduced by 0.9 points (p=0.001). Body pain diagrams reduced 46.9% after mindfulness-based stress reduction. Changes in pain pressure threshold and the global rate of change improved but were not statistically significant. Overall, patients with low back pain responded far more favorably than patients with neck pain. Positive correlations were found with improvements in self-reported pain rating, pain pressure threshold, and the global rate of change related to the extent of pain on the body pain diagram.
Conclusion: A brief body scan meditation is able to positively influence body pain diagrams, which are correlated to a pain experience. The brief body scan meditation had a larger influence on patients with low back pain than neck pain. More research is needed to explore how a non-tactile, non-threatening treatment can alter pain experiences including sensitivity of the nervous system.
Keywords: Meditation; Chronic Pain; Central Sensitization; Physical Therapy
Abbreviations: CS: Central Sensitization; CSI: Central Sensitization Inventory; GROC: Global Ratings of Change (scale); HICP: High-Impact Chronic Pain; LS: Lumbar Paraspinals; MBSR: Mindfulness-Based Stress Reduction; MCID: Minimal Clinical Important Difference; MDC: Minimal Detectable Change; NDI: Neck Disability Index; ODI: Oswestry Disability Index; PPT: Pressure Pain Thresholds; TA: Tibialis Anterior; US: United States; UT: Upper Trapezius
Introduction
Chronic pain is experienced by nearly 30% of the United States (US) population, with a prevalence higher than any other chronic medical condition [1]. High-impact chronic pain (HICP) is a subset of chronic pain defined as daily or near-daily pain that interferes with work or life. Estimates of HICP have nearly doubled since 2011, from 4.8% of the US adult population to 8% in 2016 [1,2]. As efforts have been made to better understand chronic pain in the US amidst the current opioid crisis, the need for better and safer treatments of pain continues to be researched. Central sensitization (CS) is a physiological process contributing to HICP that is defined as “an amplification of neural signaling within the central nervous system that elicits hypersensitivity” [3].
The symptom cluster of CS is proposed to include disproportionate pain, disproportionate aggravating and easing factors, diffuse palpation tenderness, psychosocial issues (i.e., high fear avoidance, pain catastrophization, etc.) [4,5]. CS additionally includes hypersensitivity to touch which often hinders traditional rehabilitation treatments such as manual therapy and exercise [6]. Recent studies related to chronic spinal pain and CS has also shown a correlation between altered body schema and chronic pain [7,8]. Clinically, these alterations show up as abnormal measurements of 2-point discrimination, left right judgement tasks, patient drawn pain maps and more [9-11].
Treating patients presenting with signs and symptoms of CS should have a multimodal approach [8] focusing on three key areas- altering faulty pain cognitions (i.e., pain neuroscience education, cognitive behavioral therapy, etc.), movement (i.e., aerobic exercise, resistance training, graded exposure, etc.), and therapeutic strategies to calm the nervous system (i.e., relaxation, mindfulness, sleep hygiene, etc.) [12-14]. In physical therapy, many treatment strategies have focused on the first two elements of the aforementioned multimodal approach to chronic pain. The third element, calming the nervous system, is slowly emerging within the scope of physical therapy. Mindfulness-based interventions have also been shown to impact the central mechanisms of pain, including pain perception and response to pain, with evidence supporting the efficacy of mindfulness in the treatment of chronic pain [15,16].
One specific mindfulness-based intervention is the Mindfulness-Based Stress Reduction (MBSR) program, which was developed and used to treat chronic pain and stress-related health issues [16]. The MBSR program includes body scan meditation, sitting meditation, walking meditation, yoga, and education about stress [17]. This program shows good efficacy for the treatment of chronic pain and stress-related health disorders [18,19]. Participation in a structured MBSR program, however, requires a considerable time commitment and access to a program, both of which can be barriers to access for therapist and patient. Body scan meditation is a practice within the MBSR program.
During the body scan meditation, attention is guided throughout the body with instructions to attend to and appraise sensations without judgment [17]. Body scan meditations have been studied as a treatment for chronic pain but not in people who suffer specifically from CS [20]. In the study by Ussher et al, a brief 10-minute body scan treatment for chronic pain showed positive changes in pain severity, pain related distress, perceived ability for daily activities, perceived likelihood of pain interfering with social relations. This study however did not specifically assess changes to signs and symptoms associated with CS. Exploring the treatment effects of a body scan meditation in someone who suffers from CS may be a valuable and practical addition to evidence-based treatments options. This case series aimed at determining if the clinical application of a single, brief 10-minute body scan meditation would positively impact a patient who presents with signs and symptoms associated with CS.
Methods
Study Design
Institutional review board approval was obtained for this study at Rockhurst University and this study was registered at clincaltrials.gov. In line with the objectives of the study a simple pre-post case series design was chosen for the study design.
Participants
This case series comprises data from a convenience sample of 16 patients seeking or already receiving physical therapy care via referral and direct access at an independently owned physical therapy clinic. Inclusion was based on criteria for recognizing CS [21], including patient report of pain of at least 3 months duration; patient report of diffuse pain that spreads outside the segmental area of primary nociception; patient’s pain is considered disproportionate to what one would expect based on the available tissue damage or presumed source of nociception; and Central Sensitivity Inventory (CSI) score of 40 or greater. Patients were excluded if they were under 18 years old or less, had neuropathic or nociceptive pain as the dominant pain mechanism, were unable to read or understand the English language, medical history and presentation were deemed not appropriate for physical therapy treatment, or patient was pregnant at the time of the study. When patients met the inclusion and exclusion criteria, they were verbally offered the option to participate in the study and given written informed consent.
Intervention
The patient was allowed to choose a comfortable position during the meditation, including the option of supine, hook lying, or sitting. The physical therapist (JM) guided the participant through a 10-minute scripted body scan meditation, which was written by the physical therapist (JM) for use in this study and in line with a previous, brief body-scan study [20]. The physical therapist counseled the participant to stop the treatment at any point during the meditation for any reason, including an increase in discomfort. Briefly, the intervention entailed a guided, step-by-step body awareness scan. Starting with the breath, the focus of attention began at the feet, progressing in a cephalad direction to the legs, trunk, and head. Throughout the meditation, awareness focused on sensations and movements of the body associated with the breath ending with a broad expansive body awareness.
Outcomes
Prior to the intervention, demographic information was collected to describe the cohort including gender, duration of pain, work status, previous meditation experience, and duration of meditation experience. Additionally, before the treatment, each patient completed a functional outcome measure to help describe the level of disability they were experiencing at the time of the study:
1) Low back pain - Oswestry Disability Index (ODI): The ODI is a 10-question self-report outcome measure that is reliable for individuals with low back pain, with higher scores indicating higher disability [22].
2) Neck pain - Neck Disability Index (NDI): The NDI is also a 10-question self-report outcome measure for people with neck pain; this outcome is reliable, valid, and responsive for acute and chronic conditions with a higher score indicating higher disability [23].
To ensure the sample of this case series represents patients with clinical signs and symptoms associated with CS, patients completed a CSI upon intake. A score of > 40 has been proposed as a higher likelihood of presenting with CS. The CSI is a 25-item questionnaire relating to CS. Subjects answer questions with a Likert scale response of 0 (never) to 4 (always). A score equal to or greater than 40 indicates the potential presence of CS and was a qualifier for the patient to be part of this study. The CSI has been shown to have good sensitivity and specificity for identifying those with CS and is considered a valid and clinically relevant indicator of patients that have centrally sensitized pain state [24,25]. The CSI was issued before the body scan meditation. No post-intervention follow-up was done on the CSI.
In line with the objectives of the study, a series of measurements were performed prior to and following treatment to assess the efficacy of the intervention:
3) Numeric pain rating scale (NPRS): Self-reported general pain was measured using the NPRS. The NPRS has been shown to have a minimally clinical important difference (MCID) of 1.0 point for chronic pain [26].
4) Body pain diagram: Participants were asked to fill in a body chart to illustrate the spatial distribution of their symptoms. Using a body pain diagram for a patient to indicate the location and extent of pain is a valid tool for identifying pain sensitization. Diffuse, spreading pain is a criterion for CS. An overlay was created as described by Margolis et al dividing the body diagram into 45 anatomical regions. The overlay was placed over the body pain diagram and each area that was colored was given a point [27,28]. A body pain diagram was issued pre-intervention and post-intervention.
5) Pain pressure threshold (PPT): A digital pressure algometer was used to assess palpation sensitivity was measured in kilograms per square centimeter (kg/cm2). Three locations were measured on the patient’s hand-dominant side using a Wagner FPX 50 algometer. These locations were as follows: (1) tibialis anterior (TA), (2) lumbar paraspinals (LS), and (3) upper trapezius (UT). To measure, the tip of the algometer was placed on the skin and before applying pressure, the examiner stated: “I am going to begin applying pressure. Tell me the moment the sensation changes from comfortable pressure to slightly unpleasant pain.” The pressure was then applied at a rate of 5 N/s. The examiner stopped applying pressure and recorded the measurement when the participants said “now.” One measurement was taken at each location. Two studies report a 15% reduction in PPT as clinically significant [29,30].
6) Global Rating of Change (GROC): The GROC is a 15-point Likert-type scale measuring perception of improvement or deterioration, ranging from -7 (“a very great deal worse”) to +7 (“a very great deal better”). The MCID for the GROC for chronic musculoskeletal pain has been reported as a positive change of 2.0 [31]. This measurement was taken after the body scan meditation.
Statistical Analysis
Microsoft Excel TM was used to enter data into spreadsheets. All observations were kept from the sample, with no modifications to the original data. Excel was used to explore descriptive statistics of the sample such as mean and standard deviation of demographics variables, as well as calculate the correlations between body map drawings, PPT in kg/cm2, NPRS, and GROC. Rstudio Cloud version 1.4 of Rstudio IDE was used in the analysis of the research questions as to whether the body scan meditation affects pressure pain thresholds and the extent of pain on a body diagram. Two-sided, paired sample t-tests in R were used to evaluate any differences between survey responses before and after meditation in NPRS, PPT in kg/cm2, and extent of pain on a body diagram.
Results
Patients
This study included 16 patients presenting with low back or neck pain (Table 1).

Self-Reported Pain
Immediately after meditation self-reported pain was reduced in a statistically significant manner (p=0.001) with a mean change of 0.97 points. The overall change in pain did not meet or exceed the MCID for chronic pain, but in 10 subjects (63%) the immediate post-change met or exceeded the MCID for pain reduction. Specific to region, low back pain rating (p=0.001) was significantly improved and exceeding the MCID, whereas neck pain rating (p=0.077) failed to do so.
Pressure Pain Thresholds
In all three regions where PPT was measured, PPT improved slightly. None of the immediate post-PPT measures were statistically significant (UT p=0.057; TA p=0.79 and LS p= 0.094). PPT for the UT (15.9%) did exceed MCID, however, the PPT did not meet or exceed the MCID for TA (1.4%) or LS (9.1%) [29,30]. Specific to region, there were no significant differences between lower back and neck pain.
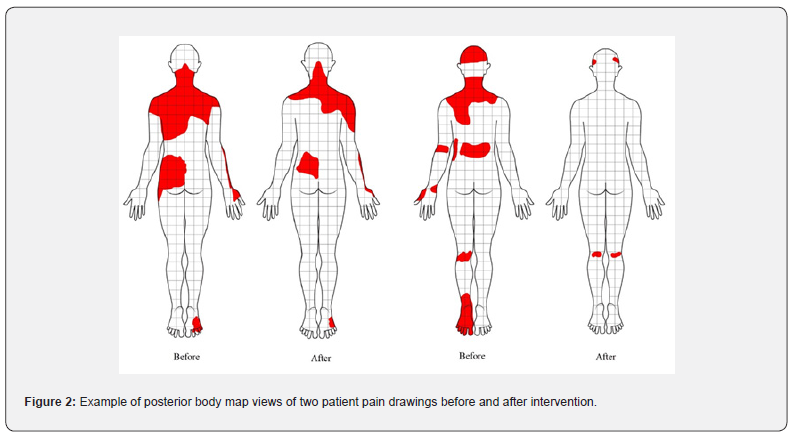
Body Maps
Pain drawings after meditation reduced significantly (p < 0.001) (Figure 1). Overall patient pain drawings after meditation reduced by 46.9%. No data is available on MCID for body map drawings. Specific to region, low back pain maps reduced by 67% (p = 0.002), whereas neck pain maps reduced by 39% (p=0.009). Figure 2 illustrates an example of two patient pain drawings before and after intervention. Global Rate of Change Scale Following the intervention, patients scored a mean score of 1.69 on the GROC, which overall did not meet or exceed the MCID of +2. On an individual level, 10 patients (62.5%) met/exceeded the MCID for the GROC after the intervention. Specific to region, patients with low back pain scored an average GROC of 2.833 meeting the MCID, whereas patients with neck pain scored an average GROC of 1.0, not meeting the MCID.

Context of OH in EAC
7.5. Correlations
Changes in self-reported pain, PPT, and GROC were analyzed in relation to spread of pain on the body diagrams. Five post-meditation measurements yielded a moderate positive correlation with reduction in body map size, including decreased pain (r = 0.51), GROC (r = 0.63), and all three PPT locations (LS (r = 0.52), UT (r = 0.35), TA (r = 0.46)).
Discussion
This is the first study to demonstrate the effects of a brief body scan meditation having a positive effect on body pain drawings and self-perception of improvement with patients who present with signs and symptoms consistent with CS. The results failed to show significant changes in PPT and overall self-reported pain ratings.
A growing body of evidence points to altered brain maps the correlation to pain especially to chronic pain [7,8]. These altered cortical maps have become a target to various physical therapy treatments to help ease pain and disability [10].
Graded motor imagery is a sequential series of techniques used in physical therapy aimed at directly influencing altered cortical maps and have shown growing efficacy in complex pain states such as complex regional pain syndrome and chronic low back pain [32]. Recent research started exploring if common therapeutic treatments (manual therapy, dry needling, exercise, and more) can also influence these altered body maps [33,34]. One shortcoming is the fact that many of these treatments including graded motor imagery often require tactile input (touch), which may be a barrier for patients presenting with allodynia and hyperalgesia [35].
Although this study failed to show any significant changes in PPT, a brief 10-minute, non-tactile treatment was able to reduce body pain drawings significantly and these reductions had a moderate correlation to reductions in self-reported pain. This is the first study to show a direct correlation between a body scan mindfulness treatment and body map drawings. Interestingly, the results showed a larger effect on low back pain versus neck pain. This finding concurs with a growing body of evidence tying chronic low back pain to altered body schema including the search for safer non-pharmacological therapeutic treatments [8,10].
In this study, overall self-reported pain did not meet or exceed MCID. This contrasts with the study by Ussher who showed a significant change in self-reported pain [20]. Our study however was conducted on a sample of patients with a mean pain duration double that of the patients in the Ussher study and specifically presenting with signs and symptoms associated with CS. Additionally, in this study, the intervention was only performed once whereas the Ussher study contained 2 interventions. It is also important to note that the immediate post-intervention pain score changes were in line with a recent meta-analysis on MBSR showing relatively small self-reported pain after MBSR interventions [16].
As with body maps, patients with low back pain did experience a reduction in self-reported pain that exceeded the MCID. This finding is important since the intervention was brief, non-tactile, and has the potential of being a part of a home exercise program which may foster greater independence and self-efficacy. As with self -reported pain the overall GROC scores failed to meet the MCID, however patients with low back pain mean GROC scores did exceed MCID. Overall, the results would imply this 10-minute body scan treatment may have more promise for patients with chronic low back pain than with chronic neck pain. This is interesting since the low back is not in a person’s visual field daily versus the neck and it has been proposed that this lack of visual input may be a contributing factor to the maintenance of chronic low back pain [36,37].
A surprising result is the lack of significant changes in PPT, be it local or remote from the effected body region. In this study there was a clinically meaningful change in upper trapezius PPT, albeit slight. Theoretically, patients with CS present with a sensitized nervous system which contributes to the clinical presentation of allodynia and hyperalgesia and is likely ideal for MBSR [6]. In this study, patients presented with PPT scores for low back and upper trapezius indicating significant sensitivity to pressure pain thresholds, which would be ideal for this intervention [38]. The PPT results, however, are consistent with previous studies showing minimal changes in PPT after MBSR [39].
Most pain-related outcomes for MBSR treatments via systematic reviews and meta-analyses, however, have explored self-reported pain and various psychosocial factors associated with pain, versus PPT [16]. These results, in conjunction with other studies, question the exact mechanism of the positive changes seen following MBSR training. Future studies will need to explore the various mechanisms underlying potential benefits of MBSR training. This study contains various limitations. First, by its design (case series) there is no control group to compare the treatment intervention. Future studies will need to further explore these results in a randomized control trial. Second, the results only report on immediate post-treatment effects and no long-term effects.
Given the powerful connection between fear avoidance and pain catastrophization this study would have benefited by adding these psychosocial variables as outcomes measure to further explore its interaction related to self-reported pain and body maps. Third, these results question the optimal dosage of a brief body-scan meditation intervention. Another shortcoming was the omission of additional validated sensory testing measures such as 2-point discrimination and localization to further connect pain drawings, self-reported pain and altered body schema in patients receiving MBSR for CS. A major oversight of the study was not to do a repeat CSI after the treatment to assess and see if the brief body scan meditation was able to shift patients below the CSI threshold for CS of 40 point.
Conclusion
A brief body scan meditation is able to positively influence body pain diagrams, which are correlated to a pain experience. The brief body scan meditation had a larger influence on patients with low back pain than neck pain. More research is needed to explore how a non-tactile, non-threatening treatment can alter pain experiences including sensitivity of the nervous system.
References
- James Dahlhamer, Jacqueline Lucas, Carla Zelaya, Richard Nahin, Sean Mackey, et al. (2018) Prevalence of Chronic Pain and High-Impact Chronic Pain Among Adults- United States, 2016. MMWR. Morbidity and Mortality Weekly Report 67(36): 1001-1006.
- Mark H Pitcher, Michael Von Korff, M Catherine Bushnell, Linda Porter (2019) Prevalence and Profile of High-Impact Chronic Pain in the United States. Journal of Pain 20(2): 146-160.
- Woolf CJ (2011) Central sensitization: Implications for the diagnosis and treatment of pain. Pain 152(3): S2-S15.
- Shraim MA, H Masse-Alarie, PW Hodges (2021) Methods to discriminate between mechanism-based categories of pain experienced in the musculoskeletal system: a systematic review. Pain 162(4): 1007-1037.
- Muath A Shraim, Hugo Massé-Alarie, Leanne M Hall, Paul W Hodges (2020) Systematic Review and Synthesis of Mechanism-based Classification Systems for Pain Experienced in the Musculoskeletal System. Clin J Pain 36(10): 793-812.
- Nijs J, B Van Houdenhove, RaB Oostendorp (2010) Recognition of central sensitization in patients with musculoskeletal pain: Application of pain neurophysiology in manual therapy practice. Manual Therapy 15(2): 135-141.
- Moseley GL (2008) I can't find it! Distorted body image and tactile dysfunction in patients with chronic back pain. Pain 140(1): 239-243.
- Benedict Martin Wand, Luke Parkitny, Neil Edward O'Connell, Hannu Luomajoki, James Henry McAuley (2011) Cortical changes in chronic low back pain: current state of the art and implications for clinical practice. Man Ther 16(1): 15-20.
- Mark J Catley, Abby Tabor, Benedict M Wand, G Lorimer Moseley (2013) Assessing tactile acuity in rheumatology and musculoskeletal medicine-How reliable are two-point discrimination tests at the neck, hand, back and foot? Rheumatology (United Kingdom) 52(8): 1454-1461.
- Bray H, GL Moseley (2011) Disrupted working body schema of the trunk in people with back pain. Br J Sports Med 45(3): 168-173.
- Dan-Mikael Ellingsen, Florian Beissner, Tawfik Moher Alsady, Asimina Lazaridou, Myrella Paschali, et al. (2021) A picture is worth a thousand words: linking fibromyalgia pain widespreadness from digital pain drawings with pain catastrophizing and brain cross-network connectivity. Pain 162(5): 1352-1363.
- Jo Nijs, Eva D'Hondt, Peter Clarys, Tom Deliens, Andrea Polli, et al. (2020) Lifestyle and Chronic Pain across the Lifespan: An Inconvenient Truth? PM R 12(4): 410-419.
- Larun L, et al. (2015) Exercise therapy for chronic fatigue syndrome. Cochrane Database Syst Rev 2(2): CD003200.
- Jo Nijs, Amarins J Wijma, Ward Willaert, Eva Huysmans, Paul Mintken, et al. (2020) Integrating Motivational Interviewing in Pain Neuroscience Education for People with Chronic Pain: A Practical Guide for Clinicians. Physical Therapy 100(5): 846-859.
- Fadel Zeidan, Nichole M Emerson, Suzan R Farris, Jenna N Ray, Youngkyoo Jung, et al. (2015) Mindfulness Meditation-Based Pain Relief Employs Different Neural Mechanisms Than Placebo and Sham Mindfulness Meditation-Induced Analgesia. The Journal of neuroscience: the official journal of the Society for Neuroscience 35(46): 15307-15325.
- Lara Hilton, Susanne Hempel, Brett A Ewing, Eric Apaydin, Lea Xenakis, et al. (2017) Mindfulness Meditation for Chronic Pain: Systematic Review and Meta-analysis. Annals of Behavioral Medicine 51(2): 199-213.
- Dreeben SJ, MH Mamberg, P Salmon (2013) The MBSR body scan in clinical practice. Mindfulness 4(4): 394-401.
- Dennis Anheyer, Heidemarie Haller, Jürgen Barth, Romy Lauche, Gustav Dobos, et al. (2017) Mindfullness-based stress reduction for treating low back pain: A systematic review and meta-analysis. Annals of Internal Medicine 166(11): 799-807.
- Daniel C Cherkin, Karen J Sherman, Benjamin H Balderson, Andrea J Cook, Melissa L Anderson, et al. (2016) Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: A randomized clinical trial. JAMA - Journal of the American Medical Association 315(12): 1240-1249.
- Michael Ussher, Amy Spatz, Claire Copland, Andrew Nicolaou, Abbey Cargill, et al. (2014) Immediate effects of a brief mindfulness-based body scan on patients with chronic pain. Journal of Behavioral Medicine 37(1): 127-134.
- Jo Nijs, Rafael Torres-Cueco, C Paul Van Wilgen, Enrique Lluh Girbes, Filip Struyf, et al. (2014) Applying Modern Pain Neuroscience in Clinical Practice: Criteria for the Classification of Central Sensitization Pain. Pain Physician 17(12): 447-457.
- Fairbank JC, PB Pynsent (2000) The Oswestry Disability Index. Spine (Phila Pa 1976) 25(22): 2940-2953.
- Joshua A Cleland, Julie M Fritz, Julie M Whitman, Jessica A Palmer (2006) The Reliability and Construct Validity of the Neck Disability Index and Patient Specific Functional Scale in Patients with Cervical Radiculopathy. Spine (Phila Pa 1976) 31(5): 598-602.
- Randy Neblett, Howard Cohen, YunHee Choi, Meredith M Hartzell, Mark Williams, et al. (2013) The Central Sensitization Inventory (Csi): Establishing Clinically Significant Values for Identifying Central Sensitivity Syndromes in an Outpatient Chronic Pain Sample. J Pain 14(5): 438-445.
- Tom G Mayer, Randy Neblett, Howard Cohen, Krista J Howard, Yun H Choi, et al. (2012) CSI central sensitivity inventory. Pain Practice 12(4): 276-285.
- Fausto Salaffi, Andrea Stancati, Carlo Alberto Silvestri, Alessandro Ciapetti, Walter Grassi (2004) Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain 8(4): 283-291.
- Margolis RB, RC Tait, SJ Krause (1986) A rating system for use with patient pain drawings. Pain 24(1): 57-65.
- Danielle Southerst, Maja Stupar, Pierre Côté, Silvano Mior, Paula Stern (2013) The reliability of measuring pain distribution and location using body pain diagrams in patients with acute whiplash-associated disorders. Journal of Manipulative and Physiological Therapeutics 36(7): 395-402.
- Moss P, K Sluka, A Wright (2007) The initial effects of knee joint mobilization on osteoarthritic hyperalgesia. Man Ther 12(2): 109-118.
- Sterling M, G Jull, A Wright (2001) Cervical mobilisation: concurrent effects on pain, sympathetic nervous system activity and motor activity. Man Ther 6(2): 72-81.
- Kamper S (2009) Global Rating of Change scales. Australian Journal of Physiotherapy 55(4): 289-289.
- PJ Daffada, N Walsh, C S McCabe, S Palmer (2015) The impact of cortical remapping interventions on pain and disability in chronic low back pain: a systematic review 101(1): 25-33.
- Louw A, Kevin Farrell, Merrill R Landers, Martin Barclay, Elise Goodman, et al. (2016) The effect of manual therapy and neuroplasticity education on chronic low back pain: a randomized clinical trial. Journal of Manual & Manipulative Therapy 25(5): 1-8.
- Matt O'Neill, Adriaan Louw, Jessie Podalak, Nicholas Maiers, Terry Cox, et al. (2022) A Case-Series of Dry Needling as an Immediate Sensory Integration Intervention. J Man Manip Ther 30(3): 165-171.
- Louw A, J Nijs, EJ Puentedura (2017) A clinical perspective on a pain neuroscience education approach to manual therapy. J Man Manip Ther 25(3): 160-168.
- M Diers, A Löffler, W Zieglgänsberger, J Trojan (2016) Watching your pain site reduces pain intensity in chronic back pain patients. Eur J Pain 20(4): 581-585.
- Martin Diers, Walter Zieglgänsberger, Jörg Trojan, Annika Mira Drevensek, Gertrud Erhardt-Raum, et al. (2013) Site-specific visual feedback reduces pain perception. Pain 154(6): 890-896.
- Linda S Chesterton, Panos Barlas, Nadine E Foster, David G Baxter, Christine C Wright (2003) Gender differences in pressure pain threshold in healthy humans. Pain 101(3): 259-266.
- Cathcart S, Maarten A Immink, Michael Proeve (2013) Mindfulness training does not reduce generalized hyperalgesia in chronic tension-type headache. Journal of Pain Management 6(3): 217-221.






























