Cognitive Impairment in Elderly - A Post Covid 19 Sequelae
Madhuri Rajbhar*1 and Rasika Kaluskar2
1Intern, College of Physiotherapy, Tilak Maharashtra Vidyapeeth, India
2Associate professor, College of Physiotherapy, Tilak Maharashtra Vidyapeeth, India
Submission: August 03, 2022; Published: August 16, 2022
*Corresponding author: Madhuri Rajbhar, Intern, College of Physiotherapy, Tilak Maharashtra Vidyapeeth, India
How to cite this article: Madhuri R, Rasika K. Cognitive Impairment in Elderly - A Post Covid 19 Sequelae. J Yoga & Physio. 2022; 10(1): 555780. DOI:10.19080/JYP.2021.10.555780
Abstract
Background: Coronavirus disease (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) also affects the nervous system. This eventually leads to cognitive impairment in about 29.9% individuals, Mild cognitive impairment in 8.9% and Dementia in about 6.8% individuals in research done previously. Thus, this study was undertaken to investigate the Cognitive impairment in elderly post COVID 19.
Material and Methods: In this study we assessed 30 elderly individuals who survived from COVID 19 with an age group of more than 60 years of age. We used TICS (Telephonic Interview for Cognitive Status) scale to find the level of cognitive impairment in elderly individuals.
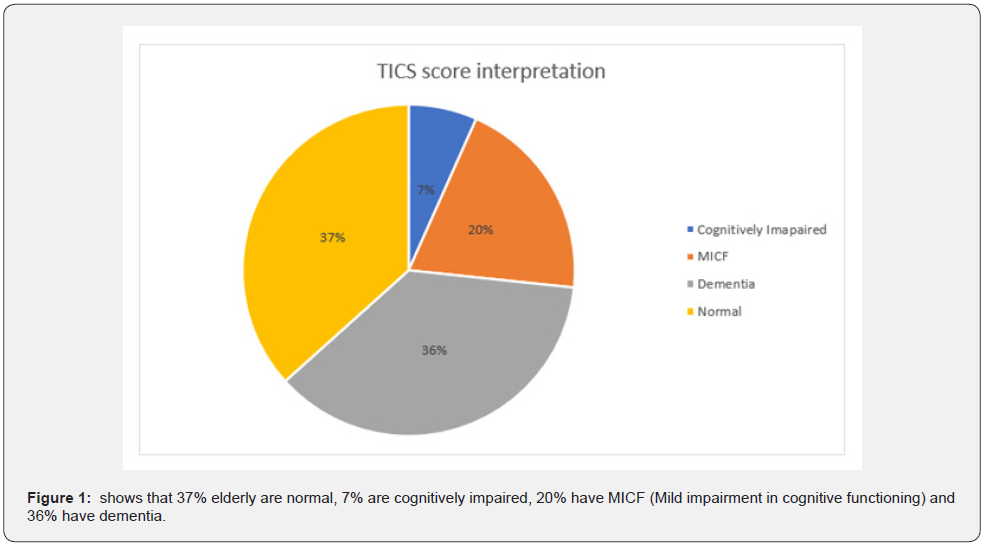
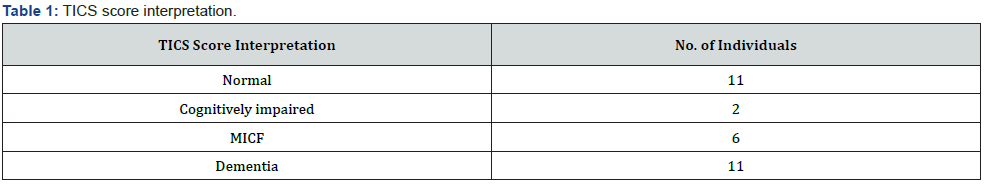
Results: According to the TICS scale, 37% elderly are normal, 7% are cognitively impaired, 20% have MICF (Mild impairment in cognitive functioning) and 36% have dementia.
Conclusion: Hence, the study concluded that there is evidence of cognitive impairment in elderly post COVID 19.
Keywords: Post COVID 19; Cognitive impairment; Elderly; Physiotherapy
Abbreviations: SARS-CoV-2: Severe Acute Respiratory Syndrome Coronavirus 2; MERS-CoV: Middle East Respiratory Syndrome Coronavirus; ACE-2: Angiotensin-Converting Enzyme-2; CNS: Central Nervous System; PNS: Peripheral Nervous System; SIRS: Severe Inflammatory Response Syndrome; TICS: Telephone Interview for Cognitive Status
Introduction
Coronavirus disease (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The first case of COVID-19 appeared in Wuhan, Hubei, China and later spread to rest of the world making it a pandemic [1]. The coronavirus is a non-segmented positive-sense RNA viruses belonging to the family Coronaviridae. Most of the human coronavirus infections are mild, but the epidemics of the two beta coronaviruses which are the severe acute respiratory syndrome coronavirus (SARS-CoV) 2,3,4 and Middle East respiratory syndrome coronavirus (MERS-CoV) 5,6 have caused more than 10,000 cumulative cases in the past two decades, with mortality rates of 10% with SARS-CoV and 37% with MERS-CoV 7,8 [2].
COVID-19 was earlier reported as a lower respiratory tract disease, with symptoms including fever, cough and shortness of breath. But at the same time, the severity of the disease varies from asymptomatic or very mild symptoms such as a cold, pneumonia, to very severe symptoms and acute respiratory failure. Reports suggested few more symptoms including anosmia (loss of sense of smell) and ageusia (loss of taste) in patients with COVID-19 infection. These symptoms helped in concluding that there is affection of the central nervous system (CNS) in a patient with COVID-19 infection [1].
The most frequent symptoms in patients affected with COVID-19 infection are broadly classified into the Central Nervous System (CNS), Peripheral Nervous System (PNS), and skeletal muscular symptoms. The CNS symptoms of these include meningitis, encephalitis, cerebrovascular complications. The peripheral nervous system symptoms include anosmia, ageusia and skeletal muscular [2] symptoms include myalgias. It is postulated that the cause of CNS involvement is either the direct injury to CNS through blood and neuronal pathways or indirectly because of an immune mediated response, hypoxia caused by decreased oxygen saturation, or by binding of subacute respiratory syndrome-coronavirus-2 to the host angiotensin-converting enzyme-2 receptor (ACE-2). The striking of the radiological findings in COVID-19 patients with neurological symptoms have also emerged [3].
The mechanism of injury for CNS damage includes direct and indirect injury. The direct mechanism of injury involves the introduction of the virus into the brain either through the hematogenous or the neuronal pathways. The neuronal route is further divided into olfactory, respiratory, and gut-brain axis routes [3].
a) Hematogenous pathway: the studies done on the mechanism of injury through the hematogenous pathway show little evidence of SARS-CoV-2 affecting the brain tissues through this pathway, however the postulated mechanism can be explained by the angiotensin-converting enzyme-2 (ACE-2) receptor acting on the endothelial cells of the capillaries. When there is presence of COVID-19 in the systemic circulation it slows down the movement of blood in the capillaries, and there is binding of SARS-CoV-2 with ACE-2 receptor. This binding with receptors results in subsequent damage and increased permeability of the blood brain barrier because of increased cytokines that can give away for nervous access [3].
b) Neuronal pathway: the movement of the COVID-19 virus either retrograde or anterograde through different peripheral nerves is one possibility by which the virus can gain access to the neuronal pathway. The most vulnerable pathway is that of the olfactory bulb pathway, which is through the cribriform plate. Some studies suggested that the removal of olfactory bulbs in mice models subsequently halted the infection from reaching the central nervous system (CNS). There is presence of viral antigens which are found in the brainstem, following connections to the respiratory tract. Viral entry in the brainstem, with alterations in neuronal groups could trigger death [3].
Many studies have also showed that the gut-brain axis entry is a potent route since there is an abundance of ACE-2 receptors on the gut epithelial cells. The enteric glial cells also express many immune cells that cause inflammatory mediators including interleukin-6 (IL-6). Therefore, the elevated IL-6 levels are observed in COVID-19 infection can lead to late CNS symptoms [3].
The indirect pathway can be broadly classified into hypoxia, immune mediated and ACE-2 receptor pathways.
a) Hypoxia pathway: the hypoxia pathway mainly attributes to less oxygen saturation which is caused by acute respiratory distress syndrome in critical patients with COVID-19. Loss of oxygen in this case causes mitochondria of the brain cells to carry out anaerobic metabolism. An increase in acid after this leads to cerebral oedema, cerebral vasodilation, and swelling of the brain cells which further exacerbate CNS complication.
b) Immune mediated pathway: the effect of other viruses had also caused significant mortality because of severe inflammatory response syndrome (SIRS)- induced multiorgan failure just like SARS-CoV-2. The activation of immune response due to such incidence can result in chronic injuries to the brain.
c) ACE-2 receptor pathway: many investigations and studies have shown that the glial cells and neuronal cells show presence of ACE-2 receptors and are likely targeted by SARSCoV- 2 once the individual is infected by COVID-19. After the infection, inside the neuronal cells, a cycle of budding is initiated causing neuronal damage without further inflammation just like SARS-CoV-1 and this subsequently damage the nervous tissue [3]. Thus, the COVID-19 infection has a wide effect on the central nervous system (CNS) and the peripheral nervous system (PNS).
The risk factors for COVID-19 involves older age, diabetes mellitus, chronic lung diseases, cardiovascular problems, obesity, immunocompromised states, chronic kidney diseases and liver diseases. All ages and both sexes are affected with COVID-19 [4]. Thus, this study aims to assess the current cognitive status and the cognitive decline in elderly patients recovered from COVID-19.
Subjects and Methods
Ethical clearance was obtained from concerned college committee, College of Physiotherapy, TMV, Pune. Virtual consent was taken from the patient before initiating the study. After getting the consent form and the demographic data, aim of the study was explained to the patient. The participants were then screened for inclusion and exclusion criteria. The participants were explained about the basic rules of the scale which is to be used during the interview. A telephonic interview was arranged for the participants. It was assured that the participants reply to each question of the questionnaire with best response. After the interview the scoring of the scale was done. Depending on the score the participants were then categorized into different groups. The obtained data was analysed using descriptive statistics.
Result
Table 1, Figure 1.
Discussion
Coronavirus disease (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. The coronavirus is a non-segmented positive-sense RNA viruses belonging to the family Coronaviridae [2]. The most frequent symptoms in patients affected with COVID-19 infection are broadly classified into the Central Nervous System (CNS), Peripheral Nervous System (PNS), and skeletal muscular symptoms. The CNS symptoms of these include meningitis, encephalitis, cerebrovascular complications. The peripheral nervous system symptoms include anosmia, ageusia and skeletal muscular symptoms include myalgias. It is postulated that the cause of CNS involvement is either the direct injury to CNS through blood and neuronal pathways or indirectly because of an immune mediated response, hypoxia caused by decreased oxygen saturation, or by binding of subacute respiratory syndrome-coronavirus-2 to the host angiotensin-converting enzyme-2 receptors. The striking of the radiological findings in COVID-19 patients with neurological symptoms have also emerged [3].
The risk factors for COVID-19 involves older age, diabetes mellitus, chronic lung diseases, cardiovascular problems, obesity, immunocompromised states, chronic kidney diseases and liver diseases. All ages and both sexes are affected with COVID-19 [4]. The need of this study is that cognitive impairment is a crucial health problem due to its adverse effect on both elderly individuals independent living and the heavy economic burden to homes and social care, thus a study was required to find the impact of COVID-19 on the cognition of the elderly people. COVID-19 not only affects the respiratory system but also the nervous system thereby affecting the cognitive ability of the patient. So, the study would help to understand the current cognitive status and the cognitive decline in elderly patients. Hence, it’s important to conduct a study on the elderly population affected by COVID-19, so the required measures can be taken to improve their cognitive status.
The aim of this study is to find the cognitive impairment in elderly post COVID-19 infection, by using the Telephone Interview for Cognitive Status (TICS). This scale will help to find the current cognitive status of the elderly population and the level of cognitive decline in those individuals. The score of the TICS scale will help to categorize the elderly individuals into normal, cognitively impaired, mild cognitive impairment and dementia, which will state the cognitive status or the neurological status of the elderly.
The interpretation of the TICS score is formulated in the Figure 1. In this study, conducted with the TICS scale 36% participants have dementia, 20% with MICF (Mild impairment in cognitive functioning), 7% are cognitively impaired and 37% participants are normal. Referring to the above data, the study conducted to find the cognitive impairment in elderly population post COVID-19 concludes that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is associated with an increased risk of long-term cognitive decline in elderly population [5].
Conclusion
Severe acute respiratory syndrome coronavirus (SARS-CoV-2) infection causes long term cognitive decline in more than half of the elderly population that is 63.33% as compared to that of the normal elderly population.
References
- Daroische R, Hemminghyth MS, Eilertsen TH, Breitve MH, Chwiszczuk LJ (2021) Cognitive Impairment After COVID-19-A Review on Objective Test Data. Front Neurol 12: 699582.
- Wu W, Wang A, Liu M, Ren L, Zhao J, et al. (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395(10223): 497-506.
- Khan AR, Farooqui MO, Jatoi NN, Jawaid S, Mahdi D, et al. (2021) Neurological Manifestations of SARS-CoV-2: A Narrative Review. Neurologist 26(1): 15-19.
- Prasad N, Gopalakrishnan N, Sahay M, Gupta A, Agarwal SK (2020) COVID-19 Working Group of Indian Society of Nephrology (2020) Epidemiology, genomic structure, the molecular mechanism of injury, diagnosis, and clinical manifestations of coronavirus infection: An overview. Indian J Nephrol 30(3): 143-154.
- Liu YH, Wang YR, Wang QH, Chen Y, Chen X, et al. (2021) Post-infection cognitive impairments in a cohort of elderly patients with COVID-19. Molecular Neurodegeneration 16(1): 48.






























