Can Yoga and Physiotherapy Benefit Patients in Weight Loss Programs and with ALS?
Bodh I Jugdutt*
Division of Cardiology, Department of Medicine, University of Alberta, Edmonton, Canada
Submission: February 19, 2018; Published: April 10, 2018
*Corresponding author: Bodh I Jugdutt, Division of Cardiology, Department of Medicine, Faculty of Medicine, University of Alberta, 2C2 Walter MacKenzie Health Sciences Centre, Edmonton, Alberta, T6G 2R7, Canada, Tel: ; Fax: (780) 437-3546; Email: bjugdutt@ualberta.ca
How to cite this article: Bodh I J.Can Yoga and Physiotherapy Benefit Patients in Weight Loss Programs and with ALS?. J Yoga & Physio. 2018; 4(4):555643. DOI: 004 10.19080/JYP.2018.04.555643
Abstract
Patients with a wide range of musculoskeletal injuries causing pain, imbalance and physical limitations are referred by their physicians for physiotherapy, and often for yoga when more advanced exercises for balance, stretching, strength and posture as well as mindful-meditation for stress reduction and healing of body, mind and spirit are needed. Recently, yoga and physiotherapy have evolved into a joint, targeted active holistic approach for optimal rehabilitative exercises and physical therapy, with added emphasis on global healing of body, mind and soul to ensure achievement and maintenance of optimal health. The benefits of yoga-physiotherapy have been documented in several studies, both as adjuncts to medical management or as primary therapy for various common conditions including hypertension, exercise intolerance due to coronary artery disease and adult-onset type 2 diabetes. These benefits are highly pertinent for the large group of overweight and obese patients who are challenged by these and other co-morbidities as well as sagging skin with weight loss. Yoga-physiotherapy is also a powerful adjunctive modality that is highly beneficial in a smaller but special group of patients afflicted with the rapidly progressing neurodegenerative motor neuron disease (MND), amyotrophic lateral sclerosis, ALS. An effective algorithm applicable to ALS is proposed. In conclusion, the practice of yoga-physiotherapy can potentially be very beneficial for managing patients in weight loss programs and with ALS. However, there is a need for more collaborative controlled randomized clinical trials (RCTs).
Keywords: ALS; Amyotrophic lateral sclerosis; MND; Motor neuron disease; RCT; Randomized clinical trials
A Physicians Perspective
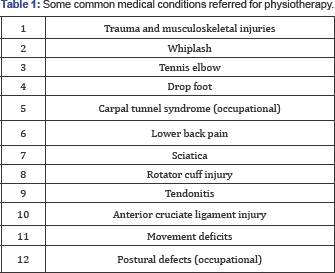
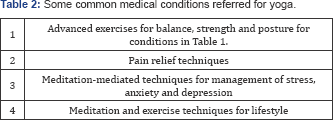
As physicians, we often see patients with a wide range of musculoskeletal injuries that require the professional services of physiotherapists, occupational therapists, rehabilitation specialists, chiropractors, yoga or yoga-physiotherapy practitioners, and others at specific stages of their acute care and subsequent recovery. We tend to prescribe physiotherapy or yoga, or both separately or combined as yoga-physiotherapy for treatment of the condition without outlining what is specifically needed. This referral approach is quite appropriate since many advances have been made in these disciplines of medicine and the formulation of the optimal treatment plan is best delegated to the experts in these disciplines. Traditionally, medical referrals for physiotherapy are made for a wide range of musculoskeletal injuries causing pain, imbalance and physical limitations (Table 1). Yoga is prescribed for those musculoskeletal ailments that can benefit from more advanced exercises for balance, stretching, strength and posture and additional mindful-meditation for stress reduction and healing of body, mind and spirit (Table 2).
Over nearly five decades of exposure to sick patients and translational research in intensive care settings of teaching hospitals, I gained an appreciation of the value of physiotherapy in accelerating recovery and healing in both medical and surgical wards. During an early phase of my career, I also witnessed the benefits of yoga and meditation in controlling blood pressure, relieving stress, and in some cases hastening healing via physiological bio-feedback mechanisms.
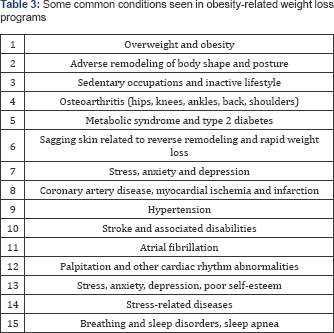

In more recent years, I have been challenged by two types of patients with problems that can be addressed by carefully designed yoga and physiotherapy protocols. The first type concerns overweight and obese patients who belong to a larger population that has grown steadily world-wide over the last five decades in developed and developing countries. They suffer from common ailments related to excessive weight, fat and poor lifestyle (Table 3) and participate in effective supervised weight loss programs and share a common frustration. While they are generally satisfied with their improved mobility, increased range of movements, diminished musculoskeletal pain, reverse remodeling of body shape and improved sense of wellbeing, many express dissatisfaction and concern with sagging skin despite trainer-supervised exercise with weights and treadmill for "toning" in gyms, and a reluctance to have to resort to bariatric surgery as a quick-fix. The second type concerns those with neurodegenerative disease and more specifically those few with a rare form of neurodegenerative motor neuron disease (MND), amyotrophic lateral sclerosis (ALS). I helplessly witnessed the frustration of three associates who were suddenly struck by ALS in their mid-twenties, mid-forties and mid-sixties, respectively, who experienced various motor deficits during progression of the disease (Table 4). After two years of research and scrutiny of the scientific and other literature including ALS websites, consultation with research colleagues worldwide working on MND and ALS , yoga and physiotherapy practitioners and patient users, I realized the potential power of carefully designed programs of combined yoga-physiotherapy as adjuncts to medical therapy for both categories of patients.
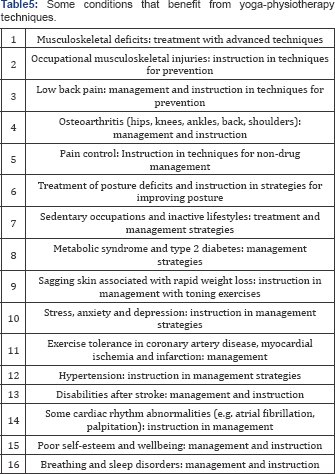
Yoga and physiotherapy have evolved into a joint targeted active holistic approach towards optimal rehabilitation in a wide range of patients, with emphasis on global healing of body, mind and soul so as to ensure both achievement and maintenance of optimal health. The applications of yoga for different types of patients have been reviewed [1]. In a randomized trial of yoga versus physical therapy for chronic low back pain, yoga was found to be non-inferior to physical therapy for function and pain [2]. The benefits of yoga-physiotherapy have been documented in various studies, either as adjuncts to medical management or as primary therapy for conditions listed in Table 5 and include hypertension, exercise intolerance due to coronary artery disease, adult-onset type 2 diabetes, tachycardia and palpitation, and insomnia (Table 5). These benefits are highly pertinent for the overweight and obese patients in weight loss programs. Benefits of comprehensive physiotherapy in obesity have been reviewed [3] although yoga may augment the benefits. Other conditions that are reported to benefit from yoga-physiotherapy include ALS [4], as well as attention-deficit- hyperactivity disorders, irritable bowel syndrome, fibromyalgia, rheumatoid arthritis, urinary-urgency and incontinence and migraine headaches [1,3].
Historically, yoga dates from the India of about 5000 years ago, with evidence in 3000 BC cave drawings of Harappa and Mohenjo-daro in the Indus valley and the teaching of Krishna in the Bhagavad-Gita of about 3102 BC during the war described in Mahabharata. Physiotherapy also originated in yoga as seen in the starting positions and postures, supine position, and hyperextensions, although it was Hippocrates who is credited as the first to teach manual manipulation in 460 BC. The combined yoga-physiotherapy approach is therefore not surprising. Whereas physiotherapy focuses on body function and dysfunction and treatment of musculoskeletal disabilities to hasten healing and restore function, yoga focuses on global wellbeing and healing of the whole person. Joint yoga- physiotherapy is applicable to both overweight patients in weight loss programs and those with ALS. In ALS patients, the therapeutic benefits of yoga incorporating relaxation, breathing technique, physical exercise and mindful-meditation have been documented [4]. In both conditions however, early intervention is required for primary prevention. Since the patients often present at fairly advanced stages, only secondary and tertiary prevention strategies can be applied to control progression and to prevent and treat complications.
The two disciplines in yoga-physiotherapy complement each other nicely; alone, each discipline has its merits, demerits and limitations; when combined in a multi-disciplinary setting, they result in synergy, enhancing benefits of each approach alone. They lead to additional benefits with respect to alleviation of pain and promotion of healing and health in their broadest sense, at mental, physical and spiritual levels. They both advocate alignment and balance between stretching and strengthening to improve posture as well as exercise for expanding range of movement without causing or aggravating injury. They both emphasize the importance of movement, mobility, locomotion and posture. In the initial one-on-one consultation, trained and licensed instructors carefully assess every patient for the degree, extent and severity of musculoskeletal deficit, defects in posture, ranges of motion at pertinent joints, degree of muscle spasm and pain with specific motions. Armed with the objective data, the yoga-physiotherapy instructors can jointly develop a careful treatment plan for correcting posture, improving physical performance, relieving pain and alleviating stress tailored to the needs of each individual patient. They also provide instruction to the patients, on an individual basis or in groups. The group approach has its merits for shared protocols.
Many centers now provide joint yoga-physiotherapy facilities. The process involving one-on-one consultation, examination, formulation of a tailored treatment plan followed by instruction is crucial for ensuring success in individual patients. Physicians need to be fully informed of the merits and offerings of the separate or joint yoga-physiotherapy facilities, the advantages, potential and limitations of each modality and the combination for their individual patients and request formal consultation by the yoga-physiotherapy practitioners. Yoga-physiotherapy can provide multiple modalities used in physiotherapy, such as manual therapy, thermal therapy, electrical therapy, prescription exercise (for core, resistance, cardio and yoga), acupuncture and trigger point needling. Electrical based therapies include electromagnetic field (EMF), electrical muscle stimulation (EMS), transcutaneous electrical nerve stimulation (TENS), neuromuscular electrical stimulation (NMES), ultrasound (US) and cold or low level laser therapy (LLLT). For optimal results, it is crucial that all players, including the instructors, physicians, caregivers and the patient, are kept in the loop. From the patient perspective, health care providers need to ensure that Medicare coverage is made available as the majority of the patients are still in the work force and a growing number are retired seniors. In fact, a significant proportion of obese patients enrolled in weight loss programs are older adults and seniors who are being treated for the medical conditions listed in Table 3 and belong to the aging population with multiple co-morbidities [5].
ALS, also known as Lou Gehrig's disease or MND, is a life- threatening disease [4,6]. While there is no cure as yet, there is hope with several experimental treatments and trials in progress. The only FDA-approved and currently available drug for ALS therapy is the glutamate blocker riluzole. Adjunctive therapy with anti-oxidants and aggressive palliative care with yoga-physio involving prescribed exercises and meditation plus rehabilitation techniques, with psychological support and counselling, offers hope for delaying or even halting progression until more definitive therapy can be found. Progressive paralysis develops from degeneration of upper and lower motor neurons in the brain and spinal cord, respectively. Depending on the stage of progression and the range of deficits (Table 4), the yoga-physiotherapy protocols need to not only be customized for the individual patient but also continuously adjusted during progression for optimal benefit. The "one-size-fits- all" approach using fixed standard protocols may not be as effective. A positive attitude, with an "expect-the-worst" but "prepare" and "hope-for-the-best" philosophy, is important for boosting patient morale during the management of progressive neurodegenerative diseases. There are different versions of ALS with different rates of progression; while some progress rapidly with 80�x0025; over 2 to 5 years mortality as with Lou Gehrig, about 10�x0025; over 10 years or more, and some progress at a much slower pace as with Stephen Hawking who has survived several decades with a strong positive attitude and aggressive supportive care [6,7]. It has been suggested that gene silencing with antisense oligonucleotide may potentially benefit some ALS patients [6]. Recently other genes that cause protein clumping in motor neurons and toxic factors produced in glial cells have also been implicated in ALS [6]. On the horizon, mesenchymal stem cells secreting neutrophic factors being studied in phase 3 trial hold promise for rapidly progressing ALS [8]. Respiratory failure is usually terminal [9].
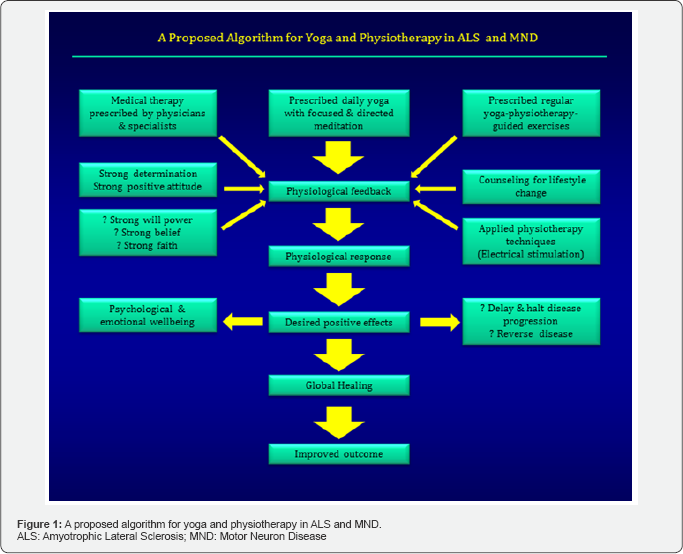
A proposed generic algorithm for a collaborative, multidisciplinary approach for ALS and MND, and also applicable to other neurodegenerative diseases is depicted in Figure 1. This requires a multidisciplinary approach with collaboration of medical and yoga-physiotherapy teams as well as other support teams for continued counseling and life-style changes and family support for morale and preserved dignity. The algorithm with minor adjustments is applicable to both ALS and MND. It should be emphasized that the integrated team approach should involve the family, especially in ALS [4].
Different types of yoga are advocated for different conditions. Hatha-yoga is especially useful for toning in weight loss programs. Shiv-yoga is useful for meditation for mass healing. It teaches healing and meditation techniques involving physical and breathing exercises for harnessing the individual's dormant divine healing energies. For optimal and prolonged lifestyle benefit with yoga-physiotherapy protocols, continued adherence is critical; protocols should be applied not just on a few minutes a day for a few days per week in the acute phase, but on a "24 /7/365" basis. However, being only human, our patients need continued support for continued adherence to the protocols in achieving ideal goals.
The practices of physiotherapy, yoga and yoga-physiotherapy have all boomed over the last decade, with new studios popping up everywhere and extensive advertisements and promotions placed on websites. While the websites are teeming with reports, anecdotes and vignettes of success, the results of the studies are often inconclusive and conflicting. There is therefore an urgent need for properly controlled RCTs with adequate sample size and multicenter participation. Besides multicenter networking and multidisciplinary collaboration, there is a need for standardization of the teaching, training and treatment protocols to be used and establishment of uniform metrics for assessing progress and improvement in yoga, physiotherapy and the combined approaches. What are the metrics for mental, spiritual and physical health and healing? Besides objective measurements of parameters for muscle strength, range of movement, muscle tone, posture and shape, loose skin fold thickness, balance, pain threshold and physical performance, physiological and hemodynamic measurements can be made. Healing of the pathological process can be assessed with biochemical markers such as those for inflammation. Psychological assessments of mood and wellbeing can be achieved using questionnaires and patient interviews. Predefined uniform criteria for assessment and improvement of quality-of-life need to be used. For RCTs, there is also need for standardization of the diagnostic criteria for the medical condition under study, and the entry and exclusion criteria to be used for recruitment of patients. The procedures for objective data collection and analysis also need to be predefined.
In conclusion, the practice of combined yoga-physiotherapy has emerged as a powerful adjunctive approach for the treatment of many disorders and can potentially be very beneficial for managing patients in effective weight loss programs and with ALS. However, there is a need for more collaborative research and controlled RCTs.
Acknowledgement
Thanks to Bernadine Jugdutt for assistance with tables and figures, and to Vijay Menon for computer assistance.
Addendum
In memoriam: Sadly, the physicist Stephen Hawking died on March 14, 2018 at age 76; he survived ALS for 55 years with a positive attitude and physiotherapy coupled with medical and supportive therapies.
References
- 1. Sovik R, Bhavanani AB (2016) History, Philosophy, and Practice of Yoga. In: Khalsa SB (Ed.), The principles and Practice of Yoga in Health Care. Handspring, East Lothian, UK, pp. 17-29.
- 2. Saper RB, Lemaster C, Delitto A, Sherman KJ, Herman PM, et al. (2017) Yoga, physical therapy, or Education for Chronic low back pain: a randomized Noninferiority trial. Ann Intern Med 167(2): 85-94.
- 3. Cieslinska Swider J (2015) Physiotherapy in the comprehensive treatment of obesity. Physiotherapy and Health activity. 23: 34-43.
- 4. Stevens J (2010) Yoga and ALS (amyotrophic lateral sclerosis). 21: 50.
- 5. Jugdutt BI (2014) Biology of aging and implications for heart failure therapy and prevention. In: Jugdutt BI (Ed.), Aging and Heart Failure. Mechanisms and Management. Springer, New York, USA, pp. 15-33.
- 6. Petrucelli L, GitlerAD (2017) New Drugs for Lou Gehrig's disease head for clinical trial. Scientific American 1: 34-42.
- 7. Harmon K (2012) How has Stephen Hawking lived past 70 with ALS? Scientific American. Scientific American 7: 1-6.
- 8. Gothelf Y, Kaspi H, Abramov N, Aricha R (2017) miRNA profiling of NurOwn: mesenchymal stem cells secreting neurotrophic factors. Stem Cell Res Ther 8(1): 249.
- 9. Lyall RA, Donaldson N, Fleming T, Wood C, Newsom Davis I, et al. (2001) A prospective study of quality of life in ALS patients treated with noninvasive ventilation. Neurology 57(1): 153-156.






























