Abstract
Guttate psoriasis (GP) is a clinical variant of psoriasis that often follows, but not always, an infection, most commonly streptococcal pharyngitis. In the past, systemic therapy for GP has been proven ineffective [1]. Given that psoriasis vulgaris and guttate psoriasis have similar pathogenesis, monoclonal antibodies targeting interleukin 23 (IL23) [2] and 12-23 (IL12/23) [3] have been shown to be effective in two case series. However, there is only one case series published examining three patients treated with multiple doses of Ixekizumab, a monoclonal antibody targeting IL-17 [4]. We present a case series exhibiting clearance of GP within 4-weeks of initial injection, following four patients who received a single dose of Ixekizumab and one patient who received two doses of Ixekizumab.
Keywords: Guttate psoriasis; One dose; Ixekizumabl; Interleukin-17
Abbreviations:GP: Guttate Psoriasis; IL23: Interleukin 23; IL-17A: Interleukin-17A; NBUVB: Narrowband-UVB; OTC: Over the Counter; ENT: Ear Nose and Throat Physician; Tregs: Regulatory T Cells
Introduction
Guttate psoriasis (GP) is an eruptive clinical variant of psoriasis characterized by multiple and diffuse small erythematous plaques (guttas, or droplets) with a predilection for the trunk and extremities. It often occurs shortly after an acute infection with group B hemolytic streptococcus of the pharynx and tonsils and accounts for 2% of all psoriasis cases. After its onset, 33% can develop chronic plaque disease, while the remainder may resolve spontaneously (within 12-16 weeks). This can cause significant distress to patients due to its pruritic and widespread nature [2]. Current treatment for GP includes treating the underlying infection (for streptococcal-B induced GP), topical corticosteroids, calcipotriene and NBUVB phototherapy [1].
GP shares several immunopathogenic features with plaque psoriasis, such as the overactivation of Th1 and Th17 cells, as well as the association with the HLA-CW6 allele [4]. Psoriasis is caused by a complex interaction between the immune system, patients’ genetic predisposition and environmental factors [1]. GP’s pathogenesis involves dysregulation of the T-helper 17 axis, which activates inflammatory lesions through IL 17, 22, & 23 and TNF-alpha [2].
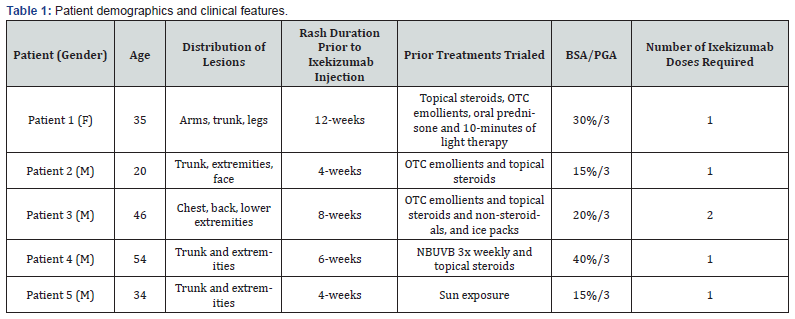
Ixekizumab is a humanized IgG4 monoclonal antibody that targets interleukin-17A (IL-17A), blocking its interaction with the IL-17A receptor, that is FDA approved for the treatment of moderate to severe psoriasis and psoriatic arthritis [4]. We present a case series of 4 patients with GP, who were successfully treated with one dose, and 1 patient with 2 doses of Ixekizumab (Table 1). All patients provided consent for photography and inclusion in this case series.
Case Series
Patient 1
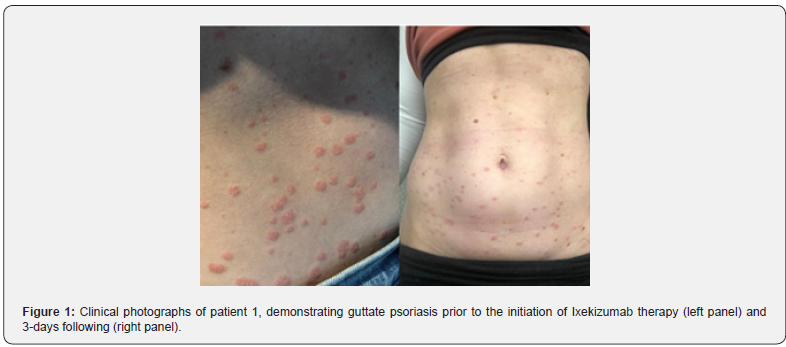
Patient 1 was a 35 year-old woman who presented with a 12-week history of guttate psoriasis, after the onset of an upper respiratory infection 3-weeks prior. She had been previously treated with topical betamethasone, triamcinolone, over the counter (OTC) emollients, 2-rounds of oral prednisone and 10-minutes of light therapy, without improvement. Physical examination showed diffuse guttate lesions, affecting the trunk and bilateral upper and lower extremities. She was treated with the subcutaneous loading dose of Ixekizumab (2 x 80mg dose, total 160mg). She reported improvement of lesions by day three (Figure 1) and almost complete clearance by day seven (Figure 2).

Patient 2
Patient 2 was a 20-year-old male who presented with a 4-week history of guttate psoriasis on the trunk, extremities, and face. Two weeks prior to the onset of the rash, he experienced a sore throat and cough with sputum production. He had tried OTC emollients and topical steroids with no improvement. On examination he had widespread GP, affecting the trunk, bilateral upper and lower extremities and face (Figure 3). He was treated with the loading dose of subcutaneous Ixekizumab (2 x 80mg dose, total 160mg). He reported improvement within 3-days, but was almost completely clear at the two-week follow-up appointment, with evidence of post-inflammatory hypopigmentation.


Patient 3
Patient 3 was a 46-year-old male with a 30-year history of multiple recurrent episodes of guttate psoriasis (biopsy proven), presenting with a persistent flare for the last couple of months. He was diagnosed with streptococcal colonization following a consultation with an Ear Nose and Throat physician (ENT). Skin examination revealed multiple, small, scaly, erythematous plaques on the chest, back, and extremities, with some coalescing into plaques on the lower extremities. He did not respond to treatment with topical OTC creams, steroidal and non-steroidal agents, and ice packs. He was treated with the loading dose of Ixekizumab (2 x 80mg dose, total 160mg) subcutaneous injections at the initial visit. At the two week follow-up visit, he reported improvement in pruritus and a decrease in plaques. During this visit he was given an additional loading dose of Ixekizumab subcutaneously. He was completely clear 1-month following the initial dose and 2-weeks following the second dose. Further doses were deferred. ENT scheduled him for a tonsillectomy.
Patient 4
Patient 4 was a 54-year-old male with a 20-year history of small plaque parapsoriasis managed with topical corticosteroids. Two-weeks following the influenza vaccination, he broke out in generalized guttate psoriasis on his trunk and extremities. NBUVB (3x weekly) and topical triamcinolone BID were attempted for 1 month with minimal improvement. He was treated with the loading dose of subcutaneous Ixekizumab (2 x 80mg dose, total 160mg). One month following injections, the patient had near complete resolution of plaques with residual post-inflammatory hyperpigmentation (Figure 4).
Patient 5
Patient 5 was a 34-year-old male with a history of guttate psoriasis following streptococcal throat infections that resolved with sun exposure. However, he had a streptococcal throat infection 1-month prior with subsequent post-streptococcal glomerulonephritis. He experienced a severe flare of guttate psoriasis that did not resolve with sun exposure and was extremely pruritic and affecting his ability to sleep. Upon physical exam, he had multiple erythematous, scaly round papules, some coalescing into plaques, on the trunk and extremities. He was treated with the loading dose of subcutaneous Ixekizumab (2 x 80mg dose, total 160mg). After 1-month, he was completely clear.
Discussion
Current research indicates that guttate psoriasis’s (GP) pathophysiology overlaps with that of psoriasis vulgaris, with an increased number of Th17 cells and decreased Foxp3þ regulatory T cells (Tregs), resulting in aberrant IL-17 production [4]. An article published in the British Journal of Dermatology [5], analyzing circulating Th1 and Th17 cells in eruptive inflammatory (EI)/GP and chronic stable (CS) psoriasis patients showed that IL-17A levels were more elevated in GP/EI patients compared to the CS group; they were able to exhibit a correlation with IL-17 levels and disease severity demonstrated with Psoriasis Area and Severity Index score. This supports the rapid improvement and resolution of the disease observed with IL–17 inhibitor treatment, Ixekizumab [5].
Conventional treatments for guttate psoriasis (GP) include antistreptococcal and non-antistreptococcal interventions [1,6]. Antistreptococcal interventions include systemic antibiotics or tonsillectomy [6]. Non-antistreptococcal interventions include topical treatments such as corticosteroids and vitamin D3 analogues, systemic treatments such as methotrexate, mycophenolate mofetil, cyclosporine, tacrolimus, or acitretin, biologics such as TNF-alpha inhibitors, or IL-17/IL-23 inhibitors, small molecule inhibitors, such as deucravacitinib, and phototherapy [1,7]. Studies show that a subset of GP patients (30-68%) are refractory to conventional therapy, thus biologic medications are emerging as a more favoured option. Although there is a lack of randomized controlled trials for the treatment of GP, there have been prior case reports and some case series documenting the improvement or resolution of GP with biologics including Guselkumab, Ustekinumab, Risankizumab, and one case series with 3 patients with Ixekizumab [2,3,4,8]. We presented five cases of guttate psoriasis treated with Ixekizumab. Four patients reached near complete resolution after only one loading dose (2 x 80mg subcutaneous injections of Ixekizumab) and one patient required two loading doses of Ixekizumab. Unlike the other case reports and series, this case series is unique in that every patient, except one, only required one loading dose of Ixekizumab in order to achieve complete clearance, suggesting that only one loading dose may be needed to achieve remission in most patients.
This case series presents further research into the potential benefit of early intervention in GP. However, given what we know about GP, it can be argued that the resolution of disease in these cases could be due to the natural history of the disease, rather than due to inhibition of IL-17, although its rapid resolution would argue against this possibility. Further randomized placebocontrolled studies need to be completed in order to determine the therapeutic potential of the inhibition of IL-17 on GP. Further limitations of this study include the lack of follow-up, limited number of patients in this case series, and lack of reimbursement for one-time doses of biologic therapies.
References
- Flora A, Frew JW (2022) A case series of early biologic therapy in guttate psoriasis: Targeting resident memory T cell activity as a potential novel therapeutic modality. JAAD Case Rep 5: 82-87.
- Maruani A, Samimi M, Stembridge N, Abdel Hay R, Tavernier E, et al. (2019) Non-antistreptococcal interventions for acute guttate psoriasis or an acute guttate flare of chronic psoriasis. Cochrane Database Syst Rev 4(4).
- Fogel AL, Strober B (2021) Successful Treatment of Guttate Psoriasis With Ixekizumab: A Case Series. Journal of Psoriasis and Psoriatic Arthritis 6(1): 12-15.
- Choe YB, Hwang YJ, Hahn HJ, Jung JW, Jung HJ, et al. (2012) A comparison of serum inflammatory cytokines according to phenotype in patients with psoriasis. Br J Dermatol 167(4): 762-767.
- Dupire G, Droitcourt C, Hughes C, Le Cleach L (2019) Antistreptococcal interventions for guttate and chronic plaque psoriasis. Cochrane Database Syst Rev 3(3).
- Strober B, Thaçi D, Sofen H, Kircik L, Gordon KB, et al. (2023) Deucravacitinib versus placebo and apremilast in moderate to severe plaque psoriasis: Efficacy and safety results from the 52-week, randomized, double-blinded, phase 3 Program for Evaluation of TYK2 inhibitor psoriasis second trial. J Am Acad Dermatol 88(1): 40-51.
- Hall SL, Haidari W, Feldman SR (2019) Resolution of guttate psoriasis plaques after one-time administration of Guselkumab. J Drugs Dermatol 18(8): 822-823.
- Brummer GC, Hawkes JE, Duffin KC (2017) Ustekinumab-induced remission of recalcitrant guttate psoriasis: a case series. JAAD Case Reports 3(5): 432-435.






























