Pathophysiological Impact of Chronic exposure of Cefalexin Antibiotic Residue above the MRL level in Mice
Md. Shafiqul Islam1*, Md. Shakil Islam2 and Sabbya Sachi1
1Department of Pharmacology, Faculty of Veterinary Science, Bangladesh Agricultural University, Mymensingh-2202, Bangladesh
2Department of Pharmacology and Toxicology, Faculty of Animal Science and Veterinary Medicine, Sher-e-Bangla Agricultural University, Dhaka-1207, Bangladesh
Submission: October 07, 2024; Published: October 14, 2024
*Corresponding author: Md. Shafiqul Islam, Department of Pharmacology, Faculty of Veterinary Science, Bangladesh Agricultural University, Mymensingh-2202, Bangladesh, Email id: shafiqpharma@yahoo.co.uk
How to cite this article: Md. Shafiqul Islam*, Md. Shakil Islam and Sabbya Sachi. Pathophysiological Impact of Chronic exposure of Cefalexin Antibiotic Residue above the MRL level in Mice. J of Pharmacol & Clin Res. 2024; 10(4): 555792. DOI: 10.19080/JPCR.2024.10.555792
Abstract
The antibiotic residue in the food chain is a growing public health problem globally because of the development of multidrug-resistant microbial populations and health hazards. In this research, we investigated chronic exposure to cefalexin antibiotic residue (250 ppm) in mice. Mice (n=10) exposed to 250 ppm cefalexin antibiotic in drinking water ad libitum for six months. Control mice (n=10) were supplied drinking water ad libitum without any treatment. Both groups of mice were provided standard mice pellets as feed. LTC analyses revealed that chronic exposure to residual levels of cefalexin antibiotic further deposited in the liver, kidney, spleen, colon, thigh muscle, and breast muscle. Chronic exposure to cefalexin antibiotic residue significantly (P<0.05) increased the body weight, up regulated ALT & AST enzymes, and decreased neutrophils and lymphocytes (P<0.05) respectively in mice. Histology analyses demonstrated an enlarged central vein, infiltration of inflammatory cells in the liver; atrophy, fragmentation of glomeruli, degeneration & necrosis in the kidney; but no visible abnormalities were found in colon architecture. This research suggested that chronic exposure to cefalexin antibiotic residue above the MRL level could affect the liver, kidney, and immune system in mice. Therefore, cefalexin antibiotic residue above the MRL level should be banned for human consumption.
Keywords: Cefalexin Antibiotic; Antibiotic Residue; Liver; ALT & AST
Abbreviations: WHO: World Health Organization; MRL: Maximum Residue Level; DLC: Differential Leucocytes Count; LDH: Lactate Dehydzrogenase; TCA: Trichloroacetic Acid; S.E.M: Standard Error Mean; AST: Aspartate Transaminase; ALT: Alanine Aminotransferase
Introduction
Antibiotics are essential and unavoidable drugs for human and animal welfare. Antibiotics are used for treatment, prophylaxis, prevention of secondary microbial infections and food & feed productions. Uses of antibiotics are not problem, but indiscriminate uses and without maintaining proper withdrawal period might cause antibiotics residues in food and feed and evolve of resistance microorganisms. Only safe food can ensure sound health. Farmers use drugs, growth promoters, hormones and antibiotics to increase their production cause drugs residues in food chain and ultimately go to the end user human body [1,2]. Chronic exposure of antibiotics residues associated with hypersensitivity reaction, carcinogenicity, mutagenicity, teratogenicity, bone marrow depression, and disruption of normal intestinal flora [3,4] as well as resistance [5]. The history of antibiotic uses in food production concerns with preventive and curative measures against animal infection. Moreover, farmers used antibiotics to increase growth rate, improve FCR, carcass quality [6,7]. Indiscriminate uses of antibiotics in food producing animals lead to antibiotic residues and resistance in humans [8].
In Bangladesh growing broiler industries play a vital role in socio-economic values and livelihood in rural people [8]. The probable causes of animal derived resistant pathogens due to irrational uses of antibiotics in animal food production [9,3] which ultimately causes human resistance pathogens [6,10-13] The global consumption of antibiotics in animals is almost twice that than that of human humans [14] and globally 63.1±1.5 tons of antibiotics are annually used in livestock [7], of which more than 80% is used in food producing animals [7]. To combat the misuses of antibiotics, the World Health Organization (WHO), the American Medical Association, and the American Public Health Association have urged a ban on growth-promoting antibiotics [15]. The maximum residue level (MRL) of antibiotics in food has been recognized worldwide by the public and government authorities. The public and government authorities should strictly monitor the products contain above the MRL of antibiotics or drugs when they are sold for human consumption. Furthermore, withdrawal time and physicochemical analyses are mandatory to ensure the antibiotics in food animals do not exceed the maximum residue limit (MRL) before the food is marketed and appropriate use of antibiotics in poultry and livestock industry [11]. Of course, antibiotic residue contaminated food and feed should be banned with the legislation and proper monitoring and investigation to save human and animal health. We investigated cefalexin antibiotic residue above the MRL level in mice and found moderately hazardous effects in mice health.
Material and Methods
Statement of the experiment
The experiment was conducted in the Department of Pharmacology, Faculty of Veterinary Science, Bangladesh Agricultural University, Mymensingh. Swiss-Albino mice were used in this experimental.
Statement of ethical approval
The laboratory experimental mice were generated and at the end of the experiment sacrificed humanely following the ethical and welfare guidelines set by the Animal Welfare and Experimental Ethics Committee of Bangladesh Agricultural University [approval number: AWEEC/BAU/2022(15)]
Selection and preparation of the experimental shed
The animals were reared in the animal experimental room with controlled temperature (25 ± 1°C) & lighting (light/dark 12:12 h) in polypropylene cages having dimensions of 30×20×13 cm and soft wood shavings were used as bedding in every cages. They were given standard mice feed supplied by ICDDR, B (International Centre for Diarrheal Diseases and Research, Bangladesh) and water ad libitum. Animals were acclimatized to laboratory conditions at least one week prior to initiation of experiment. Mice were randomly divided into two groups namely control and cephalexin antibiotic treated mice. Each group of mice consist of ten mice (n=10). Control group was kept as untreated, whereas cephalexin antibiotic treated group was supplied cefalexin @ 250 mg/L drinking water (250ppm) ad libitum for a period of six months. All procedures were done in accordance with the Ethical Committee of Bangladesh Agricultural University (AWEEC/BAU/2022(15)) and in accordance with the internationally accepted principles for laboratory animal use and care.
Biosecurity measures
A strict biosecurity program was maintained inside and outside of the research laboratory as a most effective part of the disease prevention program. Entry to the experimental laboratory was highly restricted.
Collection of antibiotics
Cefalexin was collected from Popular Pharmaceuticals Ltd., Tongi, Gazipur, Bangladesh.
Commercial Name: CEFATM-1Vet
Generic Name: Cefalexin Monohydrate
Formulation: Powder
Available Pack Size: 100gm
Strength: Each 100gm Cefalexin Monohydrate BP, equivalent to Cefalexin 7.5 gm)
Dose: 22~33mg/kg body weight (22~33ppm)
Experimental used dose: 250 mg/Liter drinking water
Weight measurement
The mice were weighed weekly and recorded in a data book. The average body weights of the mice were taken in consideration. At the end of the experiment, monthly average body weight of mice of each group was presented as mean ± SEM.
Imminent inspection of clinical signs
The mice were observed closely during the experiment and the findings were recorded accordingly. General alertness, feed intake, water intake, locomotion, and mortality were also observed regularly.
Sacrificing and sampling
At the end of the experiment, mice were sacrificed ethically for blood, serum and tissue samples for different analyses. Blood was collected into sterile heparinized and non-heparinized vials during sacrifice and were immediately stored into refrigerator separately to perform haematological tests and enzymatic analysis. Liver, kidney, spleen, intestine, breast muscle and thigh muscle samples were collected, washed individually properly in physiological saline solution and preserved at -20°C for their extraction and analysis. For histological analysis, samples were collected and preserved in neutral formalin buffer solution.
Solvents and chemicals
Analytical grade of solvents/chemicals used in the experiment.
Differential leucocytes count (DLC)
Preparation of blood smears: Two grease free, dry and clean slides with smooth and unbroken edges were taken and one of them was placed horizontally on the table. A medium sized drop of blood was taken on the left side of the slide (smearing slide). Another one (spreader slide) was placed at the middle of the smearing slide at 45° angle and was drawn backward up to touching the drop of the blood. The blood was spread up to the breath of the spreader slide. Then it was pushed forward at a continuous and medium pressure at 45° angle. A thin smear of blood was made which was dried in the air.
Staining of blood smears: Smearing slide was placed on the standing rack horizontally and added sufficient amount of Wright’s stain and allowed for 5 minutes for staining. Equal amount of distilled water was added gently blown for proper mixing and kept for 3-5 min for proper reaction. Then it was washed with running tap water and dried by air.
Identification and counting: The smear slide was placed under 10x objective of a microscope to see the staining quality. The immersion oil (a drop) was given on the focusing area of the slide and observed under 100x objects. Randomly five fields of each slide were counted. Different DLC cells in each group were presented as mean ± SEM.
AST and ALT Enzymatic Analysis
Blood was collected from wing vein, left for 30 min for coagulation, centrifuge @ 7000rmp and serum was collected for biochemical AST and ALT analysis.
AST: AST and ALT both were measured as described by [16]
Principle: AST catalyses the transfer of amino group between L-Aspartate and α -ketoglutarate to form oxaloacetate and glutamate. The oxaloacetate reacts with NADH in the presence of Malate Dehydrogenase to form NAD. The rate of oxidation of NADH to NAD is measured as a decrease in absorbance which is proportional to AST activity in the sample. Kinetic determination of the aspartate aminotransferase (AST) activity:
L-Aspartate + α - Ketoglutarate ------ (AST) ------> Oxaloacetate + L-Glutamate
Oxaloacetate + NADH + H+ ----- (Malate Dehydrogenase)-->LMalate + NAD+
Preparation: Working reagent (WR): Mix: 4 vol. (R1) buffer + 1 vol. (R2) substrate.
In assay conditions the wavelength (340 nm), cuvette (1 cm light path) and constant temperature (25°/30°/37°C) were strictly maintained in all measurement. The instrument was calibrated with to zero with distilled water. 1mL working solution and 100 μ L of sample were taken into the cuvette. Mixed, incubated for 1 minute. Reading was taken at 0 minute and then after 1 minutes intervals for three times. Absorbance differences were calculated and expressed per minute absorbance
Calculation: ΔA/min x 1750 = U/L of AST.
Histopathology analysis
Tissues were fixed with 10% neutral formalin, embedded in paraffin, and then manually sectioned with a microtome to obtain 4–5 μ m-thick paraffin sections. De-waxed sections are then stained with hematoxylin and eosin (H&E). The mounted specimens were observed and were scored under light microscopy [17,18].
Materials used for TLC
For the detection of antibiotic by Thin Layer Chromatography, these samples were stored in deep freeze at -20ºC until further advanced procedures were performed. Samples (heart, liver kidney, spleen, thigh muscle and breast muscle) were blended with a mortar and pestle until tissues were mashed properly. These samples were taken into properly cleaned and sterilized petri dishes with proper care as well as covering. From this 0.5g of sample was taken into beaker with the help of electric balance and spatula. Then homogenization was done with addition of 1ml phosphate buffer (pH 7.2). After proper mixing, protein contents of these samples were precipitated with the addition of 0.25ml trichloroacetic acid (TCA) (30%) maintaining sufficient care and attention. Then the mixed samples were taken into properly cleaned and sterilized centrifuge tubes for centrifugation. Then centrifugation was performed at 7000 rpm for 20 minutes with the help of automatically time regulated centrifuge machine.
The supernatant was extracted and an equal volume of diethyl ether was added and mixed properly in order to perform defatation. Then the mixture was kept for 10 minutes to separate layers into an upper oily layer and bottom layer. Then these mixtures were separated from each other. After discarding the upper oily layer, only bottom layer was collected. This extraction of supernatant was repeated twice with diethyl ether. The extracts were evaporated until dryness. Then, extracts were collected and investigation was done three times a sample [19].
Statistical analysis
Statistical analysis was performed by one way ANOVA using Graph pad Prism; version 6. The results were expressed as mean ± standard error mean (S.E.M).
Results
3.1. Chronic exposure of cefalexin antibiotic residue above the MRL and its effect on body weight in mice
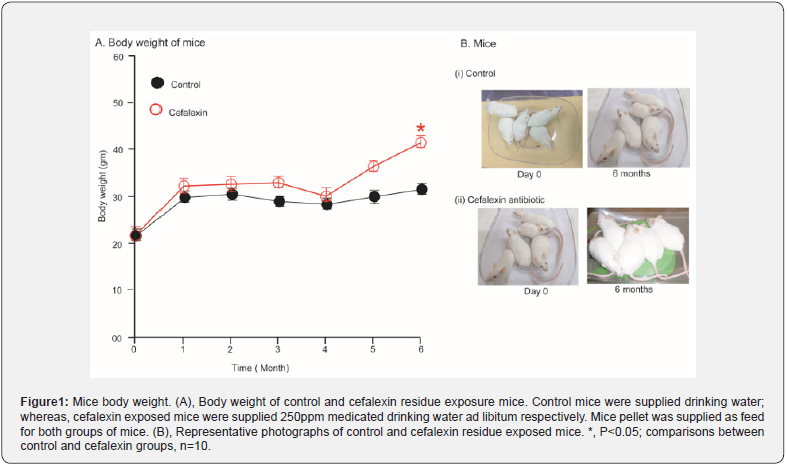
Body conditions and body weight represent vital health status in the bio-system. In Physiology animal always grows up in a regular pattern; however, hazards or diseases hamper the body weight indicating the abnormalities of the body. In some cases, overgrowth is an indicator of the abnormalities of the body. The body weight was presented in monthly in Figure 1. In control mice, body weight up regulated steadily up to 6th month of investigation but cefalexin antibiotic exposure mice abnormally up-regulated (P<0.05) the body weight indicated antibiotic growth promoting effects (Figure1).
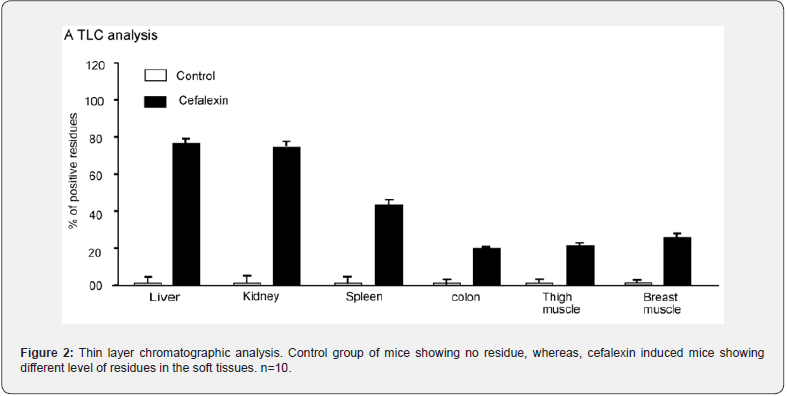
Chronic exposure of cefalexin antibiotic above the MRL and its residue in soft tissues in mice
Antibiotics residue in edible animal tissues is a global concerns. Human consumption of toxic levels of antibiotic residues above the MRL level in food origins is prohibited. We found chronic exposure of cefalexin antibiotic exposure in mice further deposited in soft tissues like liver, kidney, spleen, intestine, breast muscle, thigh muscle etc. (Figure 2). The deposition was more in liver and kidney and lower in spleen, intestine, thigh muscle and breast muscle (Figure 2). The data represented that there is no alternative ways rather to ban the residues containing animal products and byproducts for human consumption.
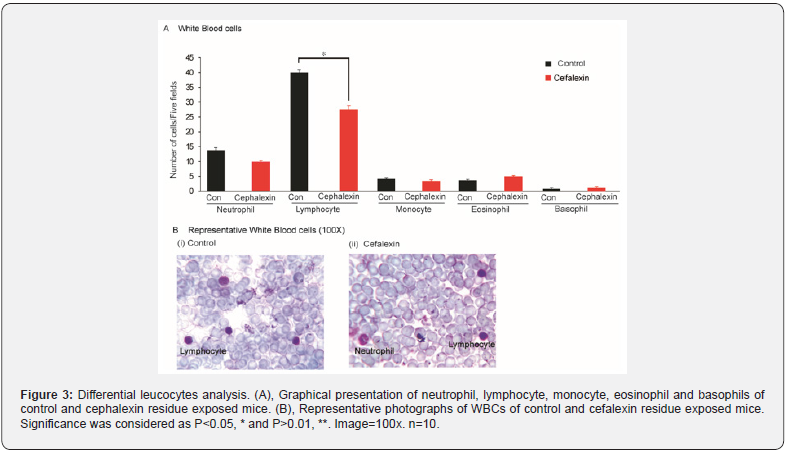
Long term exposure of ciprofloxacin antibiotic residue above the MRL and its effect on immune system in mice
Immune system plays vital role against health and diseases. In our study, we found that long term exposure of cephalexin antibiotic residue directly or indirectly hamper the lymphocyte balance in a significant manner (P<0.05) (Figure 3). Other leucocytes such as neutrophil, monocyte, eosinophil and basophil were also affected but statistically insignificant (Figure 3).
Long term exposure of cefalexin antibiotic residue above the MRL and its effect on enzyme AST and ALT
Aspartate transaminase (AST) and alanine aminotransferase (ALT) are important enzymes in liver. These enzymes are produced by liver and indicator of liver function. Under normal circumstances, these enzymes reside within liver cells to perform normal cellular functions and integrity. Liver damage causes sweep the enzymes into bloodstream. We found that 6 months ad libitum exposure of cefalexin antibiotic @ 250 ppm in water markedly increase AST and ALT level in blood (Figure 4). This data indicated that long term exposure and further deposition in liver hampered the liver functions.

Long term exposure of cefalexin antibiotic residue above the MRL and its effect on liver histology
Although long exposure of cefalexin antibiotic exposure @250 ppm in mice showed marked increased level of AST and ALT, however histology examination didn’t show any major abnormalities in liver. Liver showed enlarged central vein, infiltration of inflammatory cells into the central vein and some fatty changes (Figure 5).
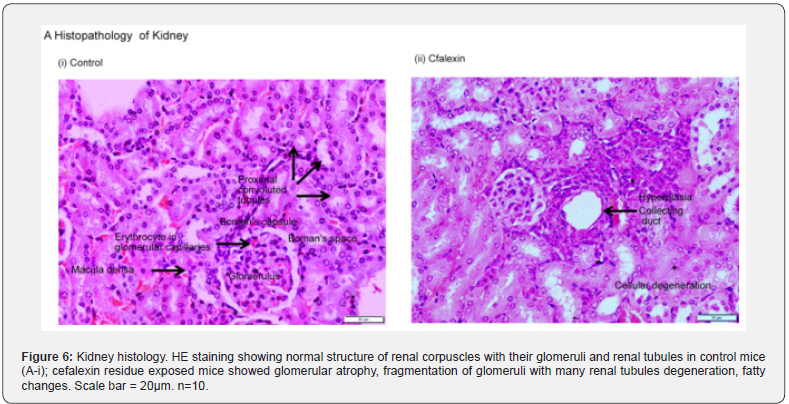
Long term exposure of cefalexin antibiotic above the MRL level and its effect on kidney histology
In control mice, histology of kidney demonstrated normal architecture of renal corpuscle with their glomeruli and renal tubules (Figure 6). Histology of cefalexin exposure mice displayed glomerular atrophy, fragmentation of glomeruli; renal tubules degeneration, sometimes hyperplasia also observed (Figure 6).
Long term exposure of cefalexin antibiotic above the permissible level and its effect on colon histology
Histology of control mice showed normal colon architecture with epithelial cells, goblet cells, crypt, lumen, stromal cells (Figure 7). Cefalexin antibiotic @ 250 ppm for a period of 6 months in drinking water didn’t demonstrate any marked abnormalities in colon structure in mice (Figure 7). This information gives a clue that antibiotics residue rarely affects the GIT.
Discussion
Indiscriminate uses of antibiotics could result resistant organism in the environment [20]. The medical science is on a big question for antibiotic resistance and a steady increase in the number of pathogens that show multi-drug resistance [21,22]. Antibiotic residue is a global problem; however, developing countries are more vulnerable than the developed countries. Antibiotic residues are associated with antibiotic resistance, immunosuppression, allergy, hepatotoxicity, bone marrow toxicity, nephrotoxicity, mutagenicity and even carcinogenicity [6]. In Bangladesh majority of the people are concerned about uses of antibiotics and they strictly follow the rules and regulation of antibiotics dose regiment, however, a few number of people don’t follow the rules strictly resulting resistant organism [23]. We have investigated the chronic exposure of cefalexin antibiotic @ 250 ppm in drinking water in mice for a period of 6 months. We found the cefalexin antibiotic increase the body weight in sub-therapeutic level. Antimicrobial agents for growth promotion in farm animal were practiced since the past. Sometimes, it was practiced as sub-therapeutic doses, sometimes as prophylactic measures, sometimes directly for growth promotion [24,1,25] As a matter of fact, the mechanisms by which antibiotics promote growth are not yet defined; however, studies have indicated that antibiotics may stimulate growth by their antimicrobial activities against pathogens and harmful bacteria.


We next investigated whether the residual level of exposure of cefalexin antibiotic further deposits in the soft tissues. The mode of administration might cause the accumulation of drugs in the liver, kidney, muscle and other vital organs and gradually execrated from the body through biotransformation. Limiting the metabolism and the elimination of drugs can result drug residues [26]. In our research, we found that the highest level of cefalexin antibiotic deposited in the liver followed by kidney, spleen, thigh muscle, breast muscle and colon. However, if the deposition remains for a long time it starts to affect the major functions of the body. Other scientists also reported antibiotics residues in liver and kidney in piglets above the MRL level [27].
The great problem of antibiotic residue is to alter the organ’s function and cellular alteration. Liver function is determined by its internal milieu of AST & ALT level. Any kind of hepatotoxicity, infections, stresses, and diseases in the liver causes AST & ALT leaked out to blood. Our study revealed that continuous exposure of antibiotic residue increased both AST and ALT level indicating an aberrant level of liver dysfunction.
Long-term exposure and unnecessary antibiotic burden in the body reduce the ability of macrophage cells to engulf the bacteria and foreign particles [28]. Health status is truly an index of immune status of the body, although in many circumstances, the immune system alone is not enough [29]. Antibiotic residue above the MRL associated with drug toxicity, allergic reactions, dermatitis, alteration of intestinal micro flora, antibiotic resistance [10], bone marrow & nephrotoxicity [6] and carcinogenicity [6], gallstones and quinolone cholestasis [30]. In our study we found that long-term exposure of cefalexin antibiotic residue altered immune cells in mice. Neutrophil and lymphocyte were found decreased in number, while eosinophil was higher and basophil was found unchanged in antibiotic treated group. Not all but some of antibiotics clear the bacterial infections as well as affect the immune system in the host [29].
We have further examined the histology of the long termterm effects to cefalexin antibiotic residue on liver, kidney and colon tissue. We found enlarged central vein, infiltration of inflammatory cells into the central vein and some fatty changes in liver. Glomerular atrophy, fragmentation of glomeruli, renal tubules degeneration was visible in kidney tissues. Other scientist also reported that antibiotic residue induced architectural abnormalities including fatty changes, enlarged central vein, infiltration of inflammatory cells in liver [31]. In our study, we could find any major architectural aberration in colon tissues.
Conclusions
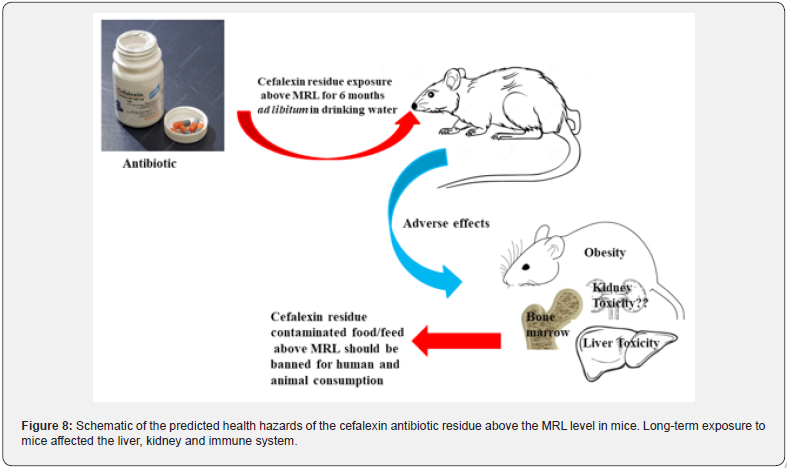
This research suggested that the chronic exposure of cefalexin antibiotic residue above the MRL to mice caused liver & kidney toxicity and lowered lymphocyte count. Therefore, chronic exposure of cefalexin antibiotic residue should be banned for human and animal consumption (Figure 8).
Author Contributions: Conceptualization, supervision & funding acquisition
Md. Shafiqul Islam designed the study, conceptualization, performed experiment, methodology, and edited the manuscript. Md. Shakil Islam edited & revised the manuscript. Sabbya Sachi edited the manuscript. All authors have read and agreed to publish the version of the manuscript.
Funding
This work was supported in part by a Grant-in-Aid for scientific research from the Ministry of Science and Technology, Government of the People’s Republic of Bangladesh by a grant in research. (Project No. 39.00.0000.009.99.023.23-363/SRG- 234533).
- Research Article
- Abstract
- Introduction
- Material and Methods
- Materials used for TLC
- Statistical analysis
- Results
- Discussion
- Conclusions
- Author Contributions: Conceptualization, supervision & funding acquisition
- Funding
- References
References
- Hao H, Cheng G, Iqbal Z, Ai X, Hussain HI, et al. (2014) Benefits and risks of antimicrobial use in food-producing animals. Front Microbiol 5: 288.
- You Y, Silbergeld EK (2014) Learning from agriculture: understanding low-dose antimicrobials as drivers of resistome expansion. Front Microbiol 5: 284.
- Okocha RC, Olatoye IO, Adedeji OB (2018) Food safety impacts of antimicrobial use and their residues in aquaculture. Public Health Rev 39: 21.
- Rather IA, Koh WY, Paek WK, Lim J (2017) The Sources of Chemical Contaminants in Food and Their Health Implications. Front Pharmacol 8: 830.
- Chen J, Ying GG, Deng WJ (2019) Antibiotic Residues in Food: Extraction, Analysis, and Human Health Concerns. J Agric Food Chem 67: 7569-7586.
- Bacanli M, Basaran N (2019) Importance of antibiotic residues in animal food. Food Chem Toxicol 125: 462-466.
- Van Boeckel TP, Brower C, Gilbert M, Grenfell BT, Levin SA, et al. (2015) Global trends in antimicrobial use in food animals. Proc Natl Acad Sci USA 112: 5649-5654.
- Chowdhury S, Ghosh S, Aleem MA, Parveen S, Islam MA, et al. (2021) Antibiotic Usage and Resistance in Food Animal Production: What Have We Learned from Bangladesh? Antibiotics(Basel) p: 10.
- Arsene MMJ, Davares AKL, Viktorovna PI, Andreevna SL, Sarra S (2022) The public health issue of antibiotic residues in food and feed: Causes, consequences, and potential solutions. Vet World 15: 662-671.
- Cunha BA (2001) Antibiotic side effects. Med Clin North Am 85: 149-185.
- Fei Z, Song S, Yang X, Jiang D, Gao J (2022) Occurrence and Risk Assessment of Fluoroquinolone Residues in Chicken and Pork in China. Antibiotics (Basel) p: 11.
- Muaz K, Riaz M, Akhtar S, Park S, Ismail A (2018) Antibiotic Residues in Chicken Meat: Global Prevalence, Threats, and Decontamination Strategies: A Review. J Food Prot 81: 619-627.
- Pereira A, Silva LJG, Rodrigues J, Lino C, Pena A (2018) Risk assessment of fluoroquinolones from poultry muscle consumption: Comparing healthy adult and pre-school populations. Food Chem Toxicol 118: 340-347.
- Aarestrup F (2012) Sustainable farming: Get pigs off antibiotics. Nature 486: 465-466.
- Graham JP, Boland JJ, Silbergeld E (2007) Growth promoting antibiotics in food animal production: an economic analysis. Public Health Rep 122: 79-87.
- Fatema K, Auditi TI, Biswas S, Ayesha SB, Helal Uddin M, et al. (2023) Investigations of hemato-biochemical and histopathological parameters, and growth performance of walking catfish (Clarias batrachus) exposed to PET and LDPE microplastics. Environ Toxicol Pharmacol 102: 104250.
- Islam MS, Kusakabe M, Horiguchi K, Iino S, Nakamura T, et al. (2014) PDGF and TGF-beta promote tenascin-C expression in subepithelial myofibroblasts and contribute to intestinal mucosal protection in mice. Br J Pharmacol 171: 375-388.
- Islam MS, Murata T, Fujisawa M, Nagasaka R, Ushio H, et al. (2008) Anti-inflammatory effects of phytosteryl ferulates in colitis induced by dextran sulphate sodium in mice. Br J Pharmacol 154: 812-824.
- Kenyon AS, Flinn PE, Layloff TP (1995) Rapid screening of pharmaceuticals by thin-layer chromatography: analysis of essential drugs by visual methods. J AOAC Int 78: 41-49.
- Rosenblatt FN (2009) The landscape of antibiotic resistance. Environmental health perspectives 117: A244-250.
- Lundborg CS, Tamhankar AJ (2017) Antibiotic residues in the environment of South East Asia. BMJ 358: j2440.
- Reis AC, Kolvenbach BA, Nunes OC, Corvini PEX (2020) Biodegradation of antibiotics: The new resistance determinants - part I. N Biotechnol 54: 34-51.
- Ahmed I, Rabbi MB, Sultana S (2019) Antibiotic resistance in Bangladesh: A systematic review. Int J Infect Dis 80: 54-61.
- Brussow H (2015) Growth promotion and gut microbiota: insights from antibiotic use. Environ Microbiol 17: 2216-2227.
- Ryan AM (2013) Will value-based purchasing increase disparities in care? N Engl J Med 369: 2472-2474.
- Manyi Loh C, Mamphweli S, Meyer E, Okoh A (2018) Antibiotic Use in Agriculture and Its Consequential Resistance in Environmental Sources: Potential Public Health Implications. Molecules p: 23.
- Gamboa-Cruz C, Barros S, Vila Pouca AS, Barbosa J, Freitas A (2021) Assessing antibiotic residues in piglet liver and kidney samples: How to manage the results obtained. Food Control 122: 107819.
- Yang JH, Bhargava P, McCloskey D, Mao N, Palsson BO (2017) Antibiotic-Induced Changes to the Host Metabolic Environment Inhibit Drug Efficacy and Alter Immune Function. Cell Host & Microbe 22: 757-765.
- Anuforom O, Wallace GR, Piddock LV (2015) The immune response and antibacterial therapy. Med Microbiol Immunol 204: 151-159.
- Hautekeete ML (1995) Hepatotoxicity of antibiotics. Acta Gastroenterol Belg 58: 290-296.
- Kleiner DE (2018) Histopathological challenges in suspected drug-induced liver injury. Liver Int 38: 198-209.






























