A1c Trends in Patients with Type 2 Diabetes receiving continuous Diabetes care during the COVID-19 Lockdown
Michelle Chu1*, Talin Bchakjian2, Li Ding3 and Scott Mosley4
1University of Southern California, Alfred E. Mann School of Pharmacy and Pharmaceutical Sciences, Los Angeles, California
2Los Angeles General Medical Center, Los Angeles, Californa
3Department of Population and Public Health Sciences, Keck School of Medicine, Los Angeles, California
4University of Southern California, Alfred E. Mann School of Pharmacy and Pharmaceutical Sciences, Los Angeles, California
Submission: June 19, 2023; Published: June 24, 2023
*Corresponding author:Michelle Chu, University of Southern California, Alfred E. Mann School of Pharmacy and Pharmaceutical Sciences, Los Angeles, 1985 Zonal Ave, Los Angeles, California, Email ID: Lee118@usc.edu
How to cite this article:Michelle Chu, Talin Bchakjian, Li Ding, Scott M. A1c Trends in Patients with Type 2 Diabetes receiving continuous Diabetes care during the COVID-19 Lockdown. J of Pharmacol & Clin Res. 2023; 9(3): 555762. DOI: 10.19080/JPCR.2023.09.555762
Abstract
Background: Clinic access was significantly limited during the initial COVID-19 lockdown, and consequently it was reported that the outcome of diabetes has worsened. It is unknown if a similar observation exists in patients who had continuous access with primary care team during the initial lockdown. This paper reviews the A1c trends and visit patterns before, during, and after the initial COVID-19 lockdown for those whose care was not interrupted.
Methods: This is a retrospective single site study. Total of 165 adults who had visits with primary care teams between March 19, 2020 through May 22, 2020, was identified. The study examined their A1c trends and visit patterns over three periods: pre-lockdown from January 1, 2019 through March 18, 2020, initial lockdown from March 19, 2020 through May 22, 2020, and post-lockdown from May 23, 2020 through December 31, 2020. Data were analyzed using Chi-square and linear regression to report A1c trends and visit patterns before and after the COVID-19 initial lockdown.
Results: Mean A1c level was lower post-lockdown than pre-lockdown (8.75% vs 9.72%, p < 0.0001), with a significant drop occurring during the lockdown. Phone visits were the dominant type of visits post-lockdown. After adjusting for visit and clinician types, more missed visits were observed during post-lockdown compared to pre-lockdown.
Discussion: A1c levels post-lockdown were significantly lower than pre-lockdown for patients with continued primary care team access for diabetes management, despite more missed visits. Further research on behavioral factors that could have influenced A1c and visit patterns may improve team diabetes care.
Keywords: Clinical Pharmacist; Collaboration; Diabetes management; COVID-19 lockdown; A1c; Primary Care Physician
Introduction
The COVID-19 pandemic created many challenges to delivering continuous quality diabetes care. Such barriers included the temporary closure of primary care clinics due to a Statewide Stay-at-Home Order, limited access to routine care, and heightened fear of severe COVID-19 infections associated with diabetes [1-5]. Although there have been reports of worsening diabetes control during the pandemic, this is unclear for patients who maintained their care from a primary care team during the lockdown and throughout the pandemic [6,7]. The aim of this study is to observe the pre-, during, and post-COVID 19 lockdown A1c trends and visit patterns for patients with type 2 diabetes having continuous access to a primary care team during the initial lockdown implemented by Los Angeles County in March 2020 [8].
Methods
This retrospective study analyzed data from electronic medical records from a primary care clinic at one of the largest county-operated medical centers in Los Angeles. The study has three periods: pre-lockdown, defined as January 1, 2019-March 18, 2020; initial lockdown, defined as March 19, 2020-May 22, 2020; and post-lockdown, defined as May 23, 2020-December 31, 2020. Patients with type 2 diabetes who are 18 years and older and received diabetes care from a primary care team at least once during the initial lockdown period and had at least two A1c values from the pre- and post-lockdown period were included. Patients were excluded if they received care from an endocrinologist. Demographics including self-reported ethnicity are reported as a mean and standard deviation for continuous variables. Frequency and percentages are reported for categorical variables, and Chisquare tests are used for comparisons. For A1c levels, linear regression with random effects adjusting patient clustering was used for analysis. The time of A1c collection was used as three linear segments in the regression model. Poisson regression was used for missed visits with robust variance and patient clustering. Face-to-face vs. phone visits, pre vs. post- lockdown period, and pharmacist vs. primary care physician visits were included in the model. The significance level is set as 2-sided, 0.05. All analyses were conducted using SAS 9.4 (SAS Institute Inc., Cary, NC, USA.).
Results
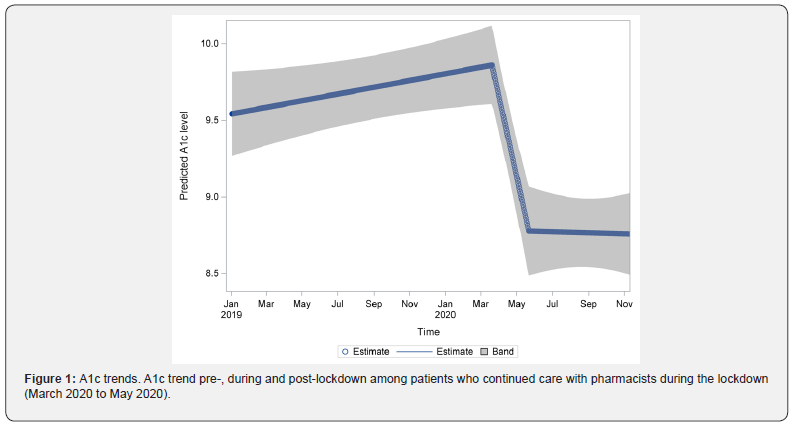
A total of 291 patients were identified, and 165 met the inclusion criteria. Most patients were female (60%), Hispanic (90%), and indicated Spanish (79%) as their primary language (Table 1). About 77% of the patients had Medicaid as their primary health insurance. More than two-thirds of the patients had at least three comorbid conditions, with about 20% having clinical atherosclerotic cardiovascular disease (ASCVD). There were 739 A1c data points during the pre-lockdown period, 64 during the initial lockdown period, and 389 during the post-lockdown period. The mean A1c level was significantly lower post-lockdown compared to pre-lockdown (8.75 (8.52, 8.98) vs. 9.72 (9.52, 9.93), p < 0.0001). After adjusting for heterogeneity, an upward trend in A1c was observed during the pre-lockdown period (0.022, p = 0.057); however, a significant drop in A1c was observed during the initial lockdown period (-0.52, p < 0.0001) (Table 2 & Figure 1). A significant trend in A1c reduction was not observed during the post-lockdown period (p = 0.91). A total of 843 face-to-face visits and 876 phone visits with pharmacists occurred during the study period. Most visits (83%) were conducted face-to-face during the pre-lockdown period, with approximately 21% being missed visits. During the post-lockdown period, phone visits (99%) were predominant, with 11% being missed visits (Table 3).
When comparing the two types of visits during the pre-lockdown period, the rate of missed face-to-face visits was significantly higher than the phone visits (21% vs. 4%, p < 0.0001). However, a similar observation was not seen during the post-lockdown period. The average rate of missed visits for an individual patient was 25% during pre-lockdown and 15.7% post-lockdown. A total of 902 face-to-face and 398 phone visits with primary care physicians occurred during the study period. The type of visits and missed visits during each period showed a similar pattern to that of the pharmacists (Table 3). During the pre-lockdown period, the rate of missed face-to-face visits was significantly higher than that of missed phone visits (19% vs. 7%; p = 0.01) for primary care physicians, but a similar pattern was not observed during the post-lockdown. On an individual-patient basis, the average rate of missed visits for primary care physicians was 15.1% pre-lockdown and 20.7% post-lockdown Our regression data showed that patients were 37.9% more likely to miss phone visits, compared to face-to-face visits, after adjusting for the timing and clinician types (RR (95% CI) 0.379 (0.284-0.504), p < 0.0001). Compared to pre-lockdown, patients were 90.6% more likely to miss any visits during the post-lockdown period after adjusting for the visit and clinician types (RR 95%CI, 1.906 (1.459-2.491), p<0.0001). There was no difference in the likelihood of missed visits based on the clinician type, pharmacist vs. primary care physician (RR 95% CI, 0.884 (0.731-1.069), p = 0.2).
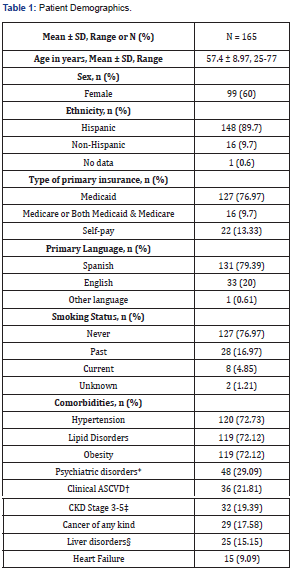
*Includes depression, anxiety, substance use disorder.
†Includes history of myocardial infarction, stroke or cerebrovascular accident, coronary artery disease, peripheral artery disease.
‡Includes end-stage renal disease and hemodialysis.
§Includes hepatitis of any kind and cirrhosis.
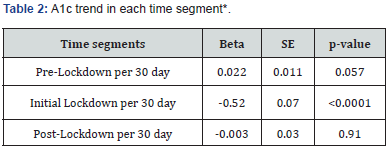
*Adjusted for participants heterogeneity.
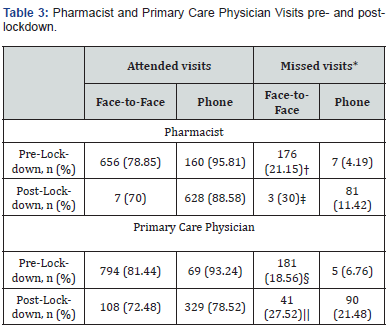
*Missed visit comparison
†p<0.0001
‡p=0.10
§p=0.01
||p=0.14
Discussion
This real-world observational study compares the A1c trends and patients’ visit patterns during the pre-, initial-, and postlockdown periods. The A1c levels during the pre-lockdown period were higher with an upward trend, dropped significantly during the initial lockdown, and then showed a slightly downward trend over time. The difference in the average A1c between pre- and post-lockdown was about 0.97%, which is considered clinically significant [9]. This magnitude of A1c reduction is also consistent with those shown in similar studies [10,11]. The A1c reduction still occurred despite the care delivery switch from face-to-face to phone visits due to the initial lockdown [12]. This suggests that the quality of diabetes care at the study site did not seem to be affected. The study site was staffed by 24 resident physicians, 1.4 FTE clinical pharmacists, and 0.4 FTE clinical resident pharmacists and had approximately 7,000 empaneled patients who are predominantly Spanish-speaking and receiving Medicaid and financial assistance. Physicians and pharmacists at this clinic have collaborated over several years to deliver type 2 diabetes management under a collaborative practice agreement. This gives pharmacists the authority to modify drug treatments. This type of co-management has shown to improve A1c levels by 0.5% to 1% at minimum, medication adherence, and self-management strategies [13,14]. Similar improvements in A1c have occurred via telehealth models, along with this study demonstrating the positive role of pharmacists in diabetes care [15]. The reduction in A1c during the post-lockdown period was not related to visit patterns. More phone visits were offered during the postlockdown period; therefore we expected lower rates of missed visits during this period and overall compared to face-to-face visits [16].
However, our study showed that phone visits were more likely to be missed than face-to-face visits when the lockdown time and clinician type were adjusted. Patients were 91% more likely to miss any visit types during the post-lockdown period compared to the pre-lockdown. It indicates that the high number of phone visits during the post-lockdown did not translate to patients’ higher adherence to the visits. Therefore, the rate of missed visits did not seem to influence the observed A1c improvements for these patients. Due to the limitations in this study, it is difficult to conclude the true impact primary care teams had on A1c improvement during the lockdown period. We did not compare the A1c changes to patients who did not receive co-management from physicians and pharmacists throughout the initial lockdown. It is unknown whether a similar trend was seen for those patients. When we observed an A1c drop during the initial lockdown period, COVID-19 was still new and induced fear, impacting people’s behavior and lifestyle [17]. Moreover, the pandemic negatively changed habits and lifestyles, affecting sleep quality, healthy behaviors, weight gain, and emotional and mental health [17,18]. Information regarding patients’ behavioral changes or attitudes during the lockdown periods was not collected for this study. Although not directly measured, our data suggest that continuous interactions between patients and primary care teams during the lockdown may have contributed positively to their diabetes management.
A common theme emerged during the visits: patients’ desire to prioritize their health through diet modifications and improved adherence to diabetes self-management practices. In addition, the primary care teams consistently noted that patients expressed fear of diabetes as an identified risk factor for severe complications and mortality related to COVID-19 infection, which seemed to drive their positive health behavior change [5,19]. Further exploration of behavioral changes affecting diabetes management, including patients with and without interruption to care, may help elucidate the factors for A1c improvement during the pandemic. Despite the arising challenges healthcare professionals faced during the pandemic, pharmacists and physicians worked closely together to co-manage diabetes. This study demonstrates that continuous patient access by phone visits through a collaborative practice between pharmacists and physicians improved A1c levels during the initial lockdown. Therefore, these results serve as a model for integrating pharmacists into diabetes care as a standard practice for all diabetes management.
References
- Mohseni M, Ahmadi S, Azami-Aghdash S (2021) Challenges of routine diabetes care during COVID-19 era: A systematic search and narrative review. Prim Care Diabetes 15(6): 918-922.
- Mertens G, Gerritsen L, Duijndam S, Salemink E, Engelhard IM (2020) Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March 2020. J Anxiety Disord 74: 102258.
- Czeisler MÉ, Marynak K, Clarke KEN (2020) Delay or avoidance of medical care because of COVID-19–related concerns - United States, June 2020. MMWR Morbidity and Mortality Weekly Report 69(36): 1250-1257.
- Chatterji P, Li Y (2021) Effects of the COVID-19 Pandemic on Outpatient Providers in the United States. Med Care 59(1): 58-61.
- Chee YJ, Tan SK, Yeoh E (2020) Dissecting the interaction between COVID-19 and diabetes mellitus. J Diabetes Investig 11(5): 1104-1114.
- Eberle C, Stichling S (2021) Impact of COVID-19 lockdown on glycemic control in patients with type 1 and type 2 diabetes mellitus: a systematic review. Diabetol Metab Syndr 13(1): 95.
- Patel SY, McCoy RG, Barnett ML, Shah ND, Mehrotra A (2021) Diabetes Care and Glycemic Control During the COVID-19 Pandemic in the United States. JAMA Intern Med 181(10): 1412-1414.
- AJMC Staff (2020) A timeline of covid-19 developments in 2020. AJMC.
- Little RR, Rohlfing C (2013) The long and winding road to optimal HbA1c measurement. Clin Chim Acta 418: 63-71.
- Matzke GR, Moczygemba LR, Williams KJ, Czar MJ, Lee WT (2018) Impact of a pharmacist-physician collaborative care model on patient outcomes and health services utilization. Am J Health Syst Pharm 75(14): 1039-1047.
- Machado M, Bajcar J, Guzzo GC, Einarson TR (2007) Sensitivity of patient outcomes to pharmacist interventions. Part I: systematic review and meta-analysis in diabetes management. Ann Pharmacother 41(10): 1569-1582.
- Demeke HB, Merali S, Marks S (2020) Trends in use of telehealth among health centers during the COVID-19.
- Adams A, Klepser M, Klepser D (2015) Physician-Pharmacist Collaborative Practice Agreements: A strategy to improve adherence to evidence-based guidelines. Evidence-based Medicine & Public Health.
- Giberson S, Yoder S, Lee MP (2015) Improving patient and health system outcomes through advanced pharmacy practice. A Report to the U.S. Surgeon General. Office of the Chief Pharmacist. U.S. Public Health Service.
- Woodhouse AG, Orvin C, Rich C, Crosby J, Keedy CA (2022) Diabetes outcomes before and during telehealth advancements surrounding COVID-19. J Am Pharm Assoc (2003) 62(1): 214-217.
- Hoffman DA (2020) Increasing access to care: telehealth during COVID-19. J Law Biosci 7(1): lsaa043.
- Pedrosa AL, Bitencourt L, Fróes ACF (2020) Emotional, Behavioral, and Psychological Impact of the COVID-19 Pandemic. Front Psychol 11: 566212.
- Giuntella O, Hyde K, Saccardo S, Sadoff S (2021) Lifestyle and mental health disruptions during COVID-19. Proc Natl Acad Sci U S A 118(9): e2016632118.
- Musche V, Kohler H, Bäuerle A (2021) COVID-19-Related fear, risk perception, and safety behavior in individuals with diabetes. Healthcare (Basel) 9(4): 480.






























