Prevalence of Acute Sinusitis in Pediatric Age Group in Satellite Town Quetta
Nida Tabassum Khan* and Muhammad Saad
Department of Biotechnology, Faculty of Life Sciences & Informatics, Balochistan University of Information Technology, Engineering and Management Sciences, Takatu Campus, Airport Road, Quetta, Balochistan, Pakistan
Submission: March 09, 2023; Published: April 04, 2023
*Corresponding author:Nida Tabassum Khan, Department of Biotechnology, Faculty of Life Sciences & Informatics, Balochistan University of Information Technology, Engineering and Management Sciences, Takatu Campus, Airport Road, Quetta, Balochistan, Pakistan
How to cite this article:Nida Tabassum Khan and Muhammad Saad. Prevalence of Acute Sinusitis in Pediatric Age Group in Satellite Town Quetta. J of Pharmacol & Clin Res. 2023; 9(2): 555758. DOI: 10.19080/JPCR.2023.09.555758
Abstract
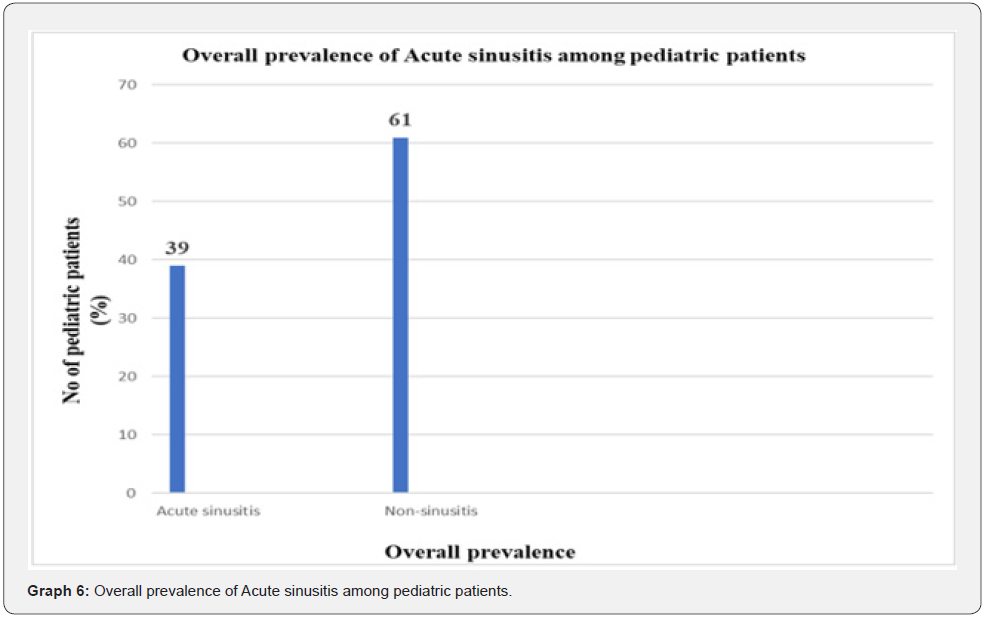
Current study concludes that the prevalence of Acute sinusitis among pediatrics age group in Satellite town Quetta is found to be relatively moderate (39%). In addition, a strong positive association between acute sinusitis and it associated symptoms were identified. Besides, triggering factors like stress, tension, cold and dust etc. escalates the intensity and quality of acute sinusitis i.e., severity of diseases. Another interesting finding of our studies revealed that in spite of moderate percentage of pediatric age group patients suffered from acute sinusitis but females were more affected than male patients which displayed lower prevalence rate. Thus, awareness and education regarding the implications of acute sinusitis among pediatric age group is must and considering the characteristics of our health system, we can infer that this study would be beneficial in the primary care setting in the future, encouraging general practitioners to make correct diagnosis and treatment of acute sinusitis.
Keywords: Paediatrics; Sinonasal; Post nasal drip; Acute; Headache
Introduction
Acute sinusitis is depicted as an exacerbation of the mucosal covering of the nasal passage and paranasal sinuses that perseveres as long as about a month [1,2]. It will in general be brought about by different variables, including allergens, respiratory diseases, microorganisms, or parasite as well as aggravations from the environment [3,4]. It is quite possibly of the most unavoidable clinical issue in pediatrics and has become more transcendent [5]. Acute sinusitis disturbs bodily fluid and causes obstruction of the sinus ostia as its pathophysiological causes [6,7]. Release of inflammatory mediators and bodily fluid hypersequestration, which disturbs the mucociliary transport framework, are factors that causes or are related with sinusitis in pediatrics [8,9]. Additionally, inflammation causes swelling, which blocks sinus outflow and can bring about bacterial infection which can possibly spread to the head and respiratory tract [10,11]. Besides, various sinusis triggers, including presence of pathogen, stress, strong, sneezing, cold/polluted air, pungent odor etc. [12,13].Thus, the aim of this research is to determine the overall prevalence of Acute sinusitis among paediatric patients and also to identify those factors that contributes towards such condition. However, since this study is a questionnaire based study therefore there could be under/over reporting of acute sinusitis prevalence among pediatric age group and additionally sample size was not very large. Thus, these were the limitations of this study.
Materials and Methods
This study is a cross sectional study conducted at Saiban family hospital among pediatric age group (1-12years) keeping sample size 100. The patients were selected at random and participation was voluntarily. All patients and their legal guardians provided informed consent.
Inclusion criteria
a) Pediatric age group (1-12years).
b) Having any one or two sinonasal symptoms persistent for 15 or more such as, runny nose (mucous discharge), nasal obstruction/congestion/fever/ headache/daytime coughing or difficulty in breathing etc.
c) Only those patients were included in the study that were not previously diagnosed with acute sinusitis and visited doctor’s clinic for first inspection since the occurrence of symptoms but may have suffered from sinusitis before.
Exclusion criteria
i. Patients which had some kind of other disease or disorder were excluded from the study such as primary or secondary diagnosis of cognitive impairment, craniofacial abnormalities, fungal diseases etc.
ii. Pediatric patients are already diagnosed with sinusitis.
iii. Pediatric patients less than one year of age.
Assessment of acute sinusitis specific symptoms in pediatric sample was achieved with the help of a questionnaire which exhibited adequate psychometric properties and also helps to determine its prevalence among the studied patients. Statistical analysis of the data was achieved using Microsoft excel 2013.
Results
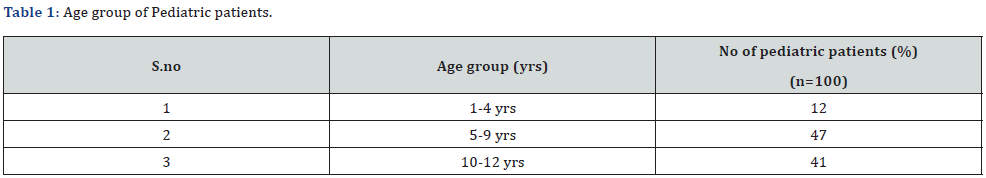
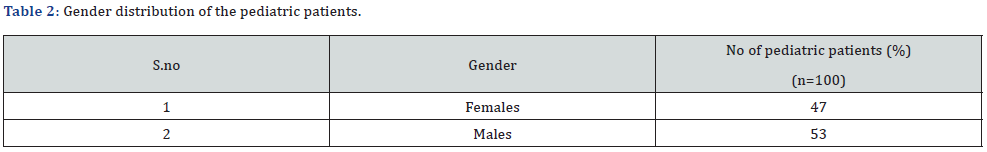
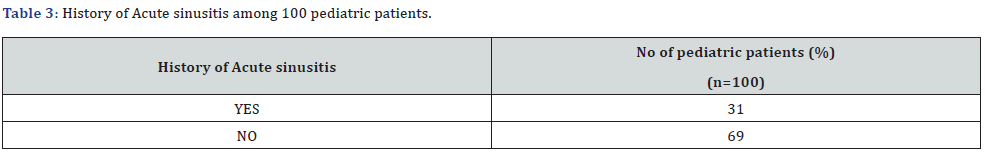
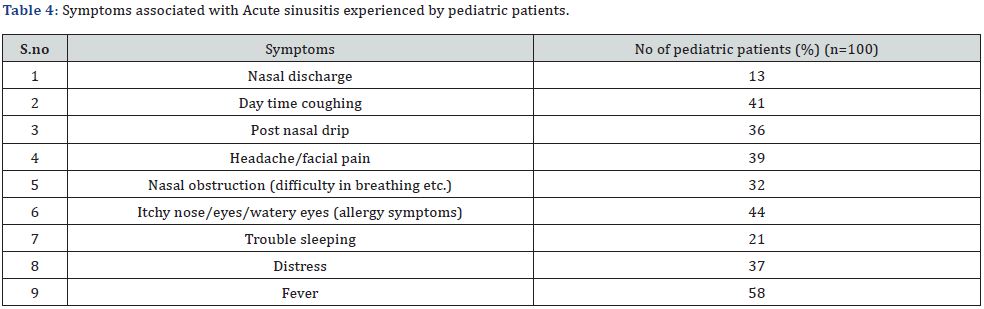
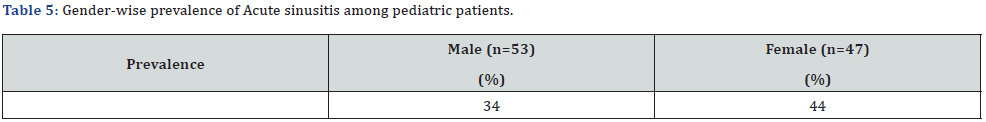
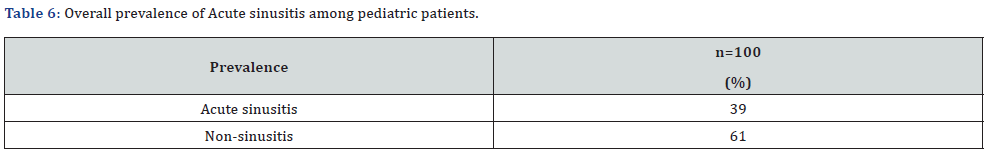
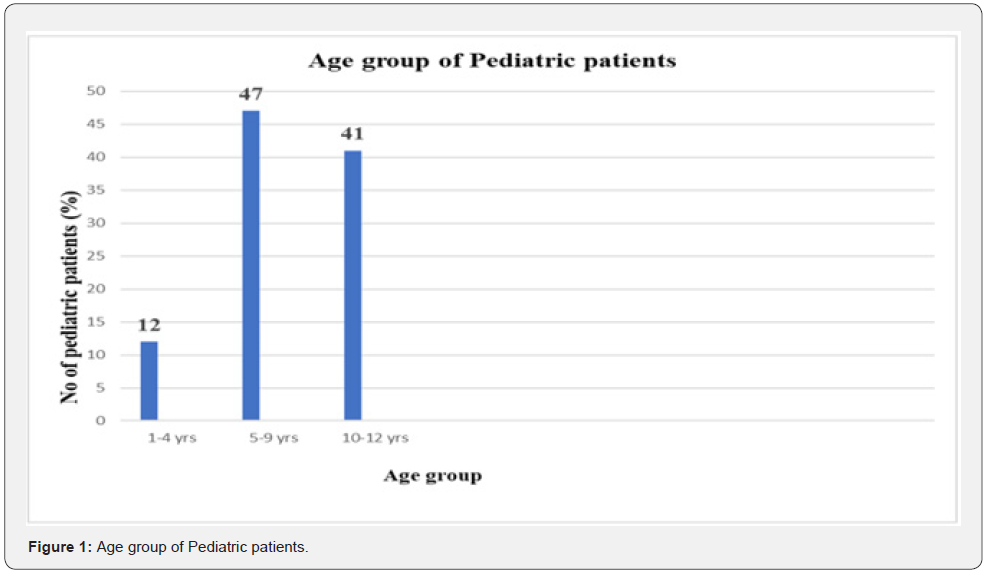
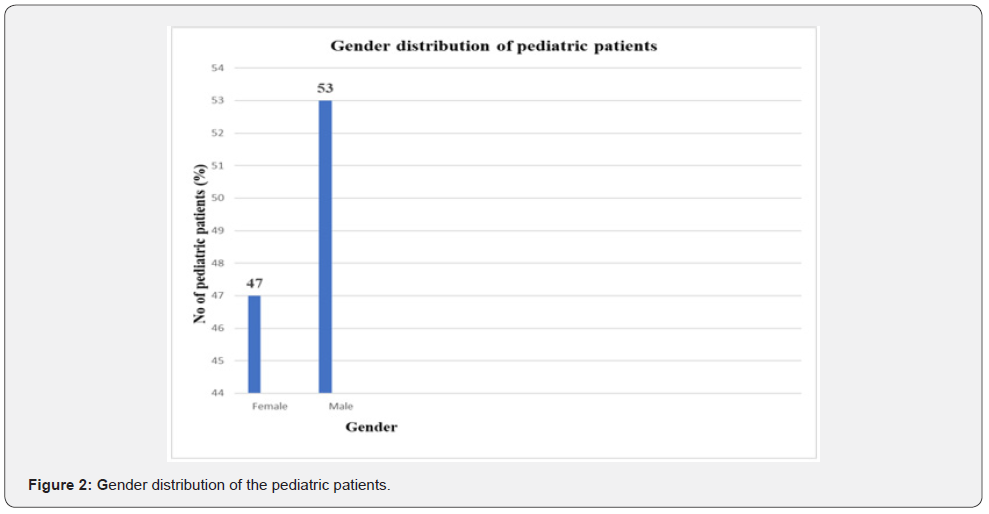
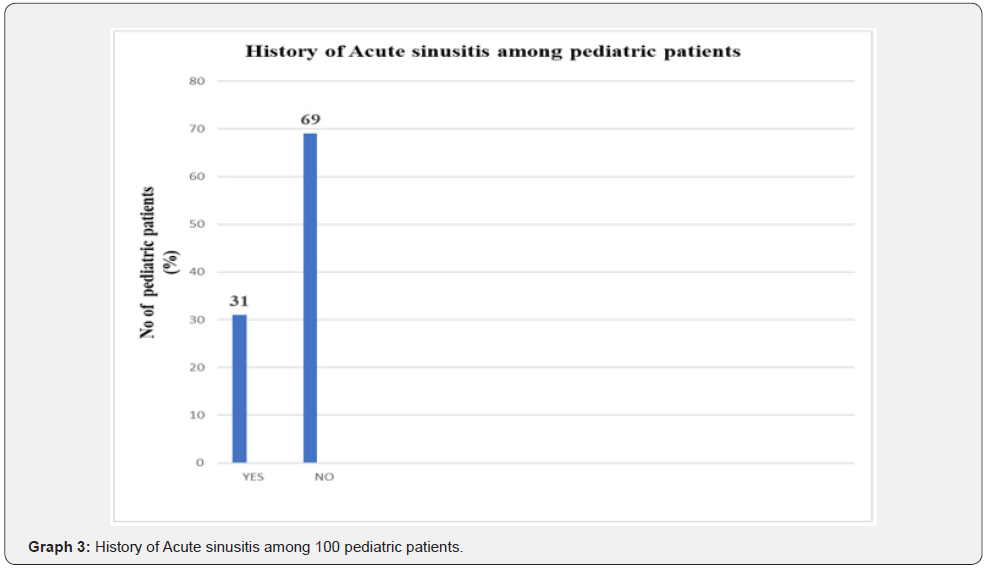
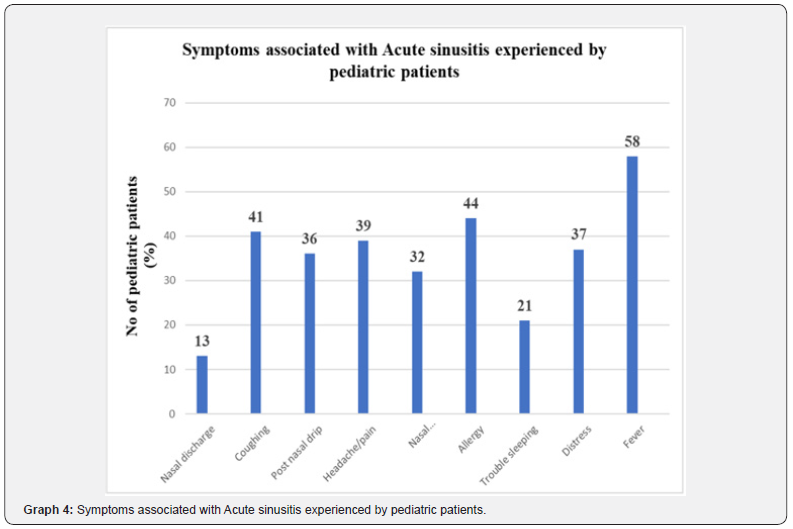
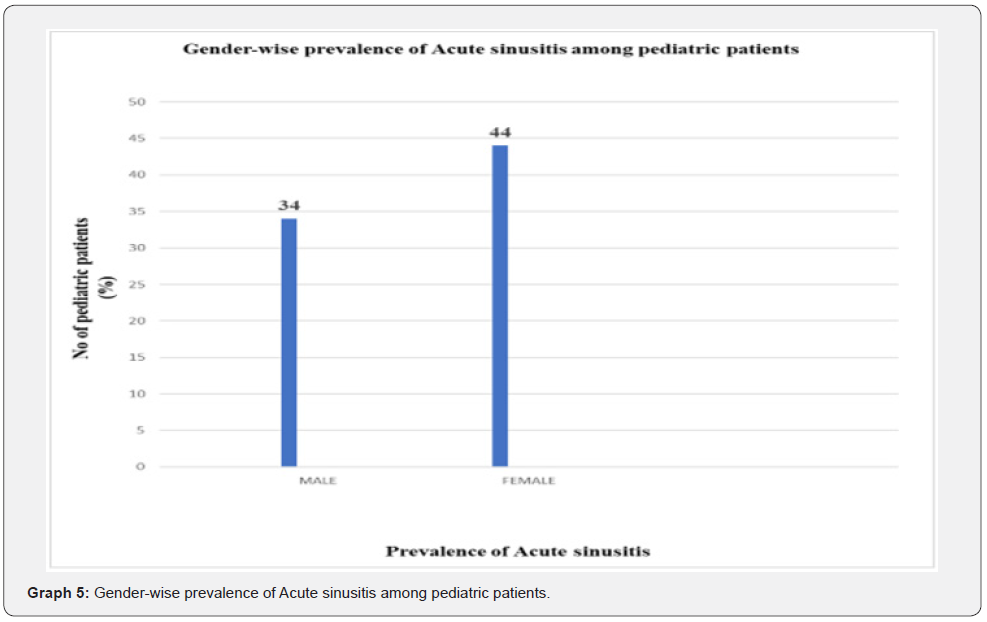
Table 1 & Graph 1 depicts the respective age group of the pediatric patients who participated in this study. Table 2 & Graph 2 depicts the gender of the pediatric patients who participated in this study. History of Acute sinusitis among 100 pediatric patients were given in Table 3 & Graph 3. Symptoms associated with Acute sinusitis experienced by pediatric patients were given in Table 4 & Graph 4. Gender-wise prevalence of Acute sinusitis among pediatric patients was given in Table 5 & Graph 5 Overall prevalence of Acute sinusitis among pediatric patients was given in Table 6 & Graph 6.
Discussion
The purpose of this study is to evaluate the prevalence and the leading causes of acute sinusitis among pediatric age groups living in Satellite town, Quetta. The results of current study showed that overall prevalence of acute sinusitis among n=100 pediatric patients was significantly low i.e., 39% [14] though a high proportion of pediatric patients i.e., 61% suffered from symptoms including headache, itchy nose/eyes i.e., allergic symptoms but were not diagnosed with acute sinusitis [15] as depicted in Graph 6.The possible reason for this high proportion is because these symptoms were quite similar to the symptoms of common cold/ seasonal fevers or infections therefore a large number of pediatric patients were not diagnosed with acute sinusitis since these patients suffered from common cold or seasonal fever perhaps [16]. Out of 100 sample size i.e., 34% of patients were males and i.e., 44% were females as shown in Graph 5. Another interesting fact found in the study were the variation seen between the symptoms. Graphically we can see that fever is the prime symptom in acute sinusitis with 58% of the individuals experiencing it [17] than nasal discharge which accounts for only 13% in individual patients as depicted in Graph 4.
Nasal discharge is a prominent symptom in common cold however in acute sinusitis post nasal drip is the clinical symptom in which mucus discharge from the nasal passage is obstructed instead mucus from nose or sinuses drips down the back of throat [18] .As far as the history of the patients with acute sinusitis is considered among 100 pediatric patients the results revealed that 31% had contracted acute sinusitis in the past which makes them more vulnerable to acute sinusitis infection [19] while remaining 69% of pediatrics had never experienced any episode of acute sinusitis. Perhaps a complete family history should be taken in account in future to identify the proneness of a particular pediatric patient to this respiratory distress [20]. Though, if these above-mentioned symptoms along with non-consistent symptoms such as nasal discharge, allergies etc. that varies from patient to patient are not treated will soon become chronic affecting the quality of life of a child [21]. Sinusitis can be characterized into many types including mild, severe and acute based on the severity of the symptoms for which clinical examination is a must [22]. Acute sinusitis should be treated if proper treatment is not administered on time, it can become chronic [23]. Additionally, increase of particulate matter in the atmosphere, plays a vital role in causing acute sinusitis or worsen its existing symptoms [24]. But precautionary measures like wearing masks, eating healthy etc. and proper medication could minimize the chances of its occurrence among children [25].
Conclusion
We consider this study as a helpful guide to properly diagnose acute sinusitis and distinguish it from common cold on the basis of symptoms. In addition, the identified environmental factors that causes or worsen acute sinusitis symptoms among children could be overcome with the help of medication or precautionary measures. By comparing the healthcare system of our country to other countries we can say that this study will be favorable in primary care settings in coming future.
- Research Article
- Abstract
- Introduction
- Materials and Methods
- Results
- Discussion
- Conclusion
- References
References
- Worrall G (2011) Acute sinusitis. Can Fam Physician 57(5): 565-567.
- Diaz I, Bamberger DM (1995) Acute sinusitis. In Seminars in respiratory infections 10(1): 14-
- Low DE, Desrosiers M, McSherry MB, Garber G, Williams Jr, et al. (1997) A practical guide for the diagnosis and treatment of acute sinusitis. CMAJ 156(6): S1-14
- Brook I (2013) Acute sinusitis in children. Pediatr Clin North Am 60(2): 409-424.
- Wald ER (1992) Sinusitis in children. N Engl J Med 326(5): 319-323.
- Hytönen, Timo A, Anne PM (2000) Complications of acute sinusitis in children. Acta Oto-Laryngologica 120(545): 154-157.
- Reid JR (2004) Complications of pediatric paranasal sinusitis. Pediatr radiol 34(12): 933-942.
- Manning SC (1993) Pediatric sinusitis. Otolaryngologic Clinics of North America 26(4): 623-638.
- Cauwenberge PV, Ingels K (1996) Effects of viral and bacterial infection on nasal and sinus mucosa. Acta otolaryngol 116(2): 316-321.
- Friedman R, Ackerman M, Wald E, Casselbrant M, Friday G (1984) Asthma and bacterial sinusitis in children. J Allergy clin immunol 74(2): 185-189.
- DeMuri GP, Wald ER (2012) Acute bacterial sinusitis in children. N Engl J Med 367(12): 1128-1134.
- Peters AT, Spector S, Hsu J, Hamilos DL, Baroody FM, et al. (2014) Diagnosis and management of rhinosinusitis: a practice parameter update. Ann Allergy Asthma Immunol 113(4): 347-385.
- Badr DT, Gaffin JM, Phipatanakul W (2016) Pediatric rhinosinusitis. Curr Treat Options Allergy 3(3): 268-281.
- Eniolaa EJA, Bolaa AY, Clementx N (2014) The prevalence of nasal diseases in Nigerian school children. Journal of Medicine and Medical Sciences 5(4): 71-77.
- Short S, Bashir H, Marshall P, Miller N, Olmschenk D (2017) Diagnosis and treatment of respiratory illness in children and adults. Bloomington: Institute for Clinical Systems Improvement.
- Recommendation, A. E. P. C. Treating the Common Cold.
- Fireman P (1992) Diagnosis of sinusitis in children: emphasis on the history and physical examination. J Allergy clin immunol 90(3): 433-436.
- Wald ER (1991) Purulent nasal discharge. Pediatr infect dis J 10(4): 329-333.
- Wald ER (1992) Sinusitis in infants and children. Ann Otol Rhinol Laryngol Suppl 155: 37-41.
- Fireman P (1992) Diagnosis of sinusitis in children: emphasis on the history and physical examination. J Allergy clin immunol 90(3): 433-436.
- Kay DJ, Rosenfeld RM (2003) Quality of life for children with persistent sinonasal symptoms. Otolaryngol Head Neck Surg 128(1): 17-26.
- Shaikh N, Hoberman A, Kearney DH, Colborn DK, Kurs-Lasky M, et al. (2013) Signs and symptoms that differentiate acute sinusitis from viral upper respiratory tract infection. Pediatr Infect Dis J 32(10): 1061-1065.
- Dykewicz MS (2003) 7 Rhinitis and sinusitis. Journal Allergy and clinical immunology 111(2): S520-S529.
- Silviu-Dan F (2014) Pediatric chronic rhinosinusitis. Pediatric Annals 43(8): e201-e209.
- Lieser JD, Derkay CS (2005) Pediatric sinusitis: when do we operate?. Curr Opin Otolaryngol Head Neck Surg 13(1): 60-66.






























