Medication Adherence and Associated Factors Among Patients with Epilepsy at Follow Up Clinics of Jimma Town Public Hospitals, Jimma, South West, Ethiopia, 2019
Ismael Ahmed, Abebe Abera Tesema*, and Tigist Demeke
Institute of health faculty of health sciences, School of nursing and midwifery, Jimma university, Ethiopia
Submission: October 19, 2019;Published:January 22, 2020
*Corresponding author:Abebe Abera Tesema, Institute of health, faculty of health sciences, School of nursing and midwifery, Jimma University, Ethiopia
How to cite this article:Abebe Abera Tesema, Ismael Ahmed, Tigist Demeke. Medication Adherence and Associated Factors Among Patients with Epilepsy at Follow Up Clinics of Jimma Town Public Hospitals, Jimma, South West, Ethiopia. J of Pharmacol & Clin Res. 2020; 8(1): 555735. DOI:10.19080/JPCR.2019.08.555735
Abstract
Background: Epilepsy is a neurological disorder, which alters brain activities, causing seizures or periods of unusual behavior, sensations, and sometimes loss of awareness. It results in multidimensional and long-term effect on the patients and society. Adherence to therapeutic medication is critical for patients with epilepsy. The issue of adherence still considered as secondary treatment gap and the most important cause of poorly controlled epilepsy in developing countries particularly in Ethiopia. Therefore, the aim of this study is to assess medication adherence and associated factors among patients with epilepsy at follow up clinics in Jimma town public hospitals, April 08 to May 20/2019.
Methods: To conduct the study we used institution based cross-sectional design. We collected the data by using structured interviewer administered questionnaire and data extraction checklist. Simple random sampling was used to select study participants. The collected data entered into EPI data version 3.5.3 and exported to SPSS version 23 for analysis. Variables with p-value of <0.25 on bivariate analysis were entered for multivariate analyses. P-value of <0.05 on multivariate analysis was considered as statistically significant.
Result: From 301 study participants 297 patients were actually involved in the study giving a response rate of 98.7%. Of these 297 respondents 169(56.9%) were male, 145 (48.8%) were in the age group of 18 -23 years and 142(47.8%) were single by their marital status. concerning their adherence to antiepileptic medications 151(50.8%) had good adherence. Source of medication, felt stigma, seizure frequency and medication concern belief were significantly associated with adherence to anti-epileptic medications.
Conclusion: This study found that about half of the study participants had good adherence to anti-epileptic medications and some factors were found to be significantly associated with adherence. Nurses and other health care providers should provide health education and medication related counseling for all patients with epilepsy to improve adherence.
Keywords:
Adherence; Anti-epileptic medication; Associated factors; Jimma Ethiopia
Introduction
Epilepsy is the most common chronic neurological disorder characterized by recurrent and unprovoked seizure. It results in brief episodes of involuntary movement that may involve one part of the body or the entire body. It affects about 50 million people of worldwide and almost 80% of them living in developing countries. Epilepsy is the second most burdensome neurologic disorder worldwide in terms of disability-adjusted life years and with lifetime prevalence of 7.60 per 1,000 persons [1,2]. International League against Epilepsy classifies epilepsy by manifestations during seizure attack and EEG feature between attacks as partial seizures, generalized seizures and unclassified seizures. This clas sification is important for understanding of underlying etiology, selecting appropriate treatment and understanding the prognosis of seizure types [1,3].
The primary cause of epilepsy is not unknown but congenital anomalies, perinatal injuries, intracranial tumors, CNS infection, vascular and metabolic abnormalities are secondary causes of epilepsy. Most causes of secondary epilepsy are preventable and treatable [1,2]. Epilepsy symptom can be successfully treated with one or more antiepileptic medication even though about 50% of patients manifest mild to moderately severe adverse effects. Currently available anti-epileptic drugs can control seizure around 70-80% in patients with new onset epilepsy [1,2,4]. Epilepsy is important public health problem with 0.6% of global burden of disease posing significant impact on less developed countries where epilepsy incident is 10 times more common than the developed world. It results significant economic impact in terms of health care need, premature death and loss of work productivities.
Different scholars define Adherence as “the extent to which an individual’s behavior regarding taking medications, following a dietary plan, and performing lifestyle changes, follows agreed recommendations from a health-care provider.” Medication adherence increase if the patients and families are involved in treatment choice as well as mutual agreement between the health provider. Adherence to anti-epileptic medications result in decrement of relapses, minimized frequency of seizures, decreased cost of health care, increased therapeutic benefits and better patient outcomes [5-7]. Factors like forgetfulness, number of medications prescribed, dosing frequency, type of seizure and duration of illness influence medication adherence among epileptic patients [6,8].
Epilepsy affects an estimated 2.3 million adults in the US and more than 200,000 new cases per year [9,10]. The World Health Organization (WHO) estimates that 80% of PLWE live in developing countries with higher incidence and prevalence than high-income countries with median prevalence of 9.5/1,000 compared to 8/1,000 in Europe with widely varying prevalence among countries [11,12]. In Africa around 10 million people are directly affected by epilepsy and there are wide treatment gaps to 100% in some communities [13]. In Ethiopia prevalence of epilepsy was 5.2/1000 with annual incidence of 64 per 100,000 populations [14].
Epilepsy results in variety of medical, social, psychological and economic impact particularly in undeveloped countries in which its incidence and prevalence is highly increasing [2,15]. Worldwide social stigma and discrimination toward patients with epilepsy and their families make it difficult to overcome the disease since it results in lack of social support or experience social isolation, embarrassment, fear and discrimination, and some parents may feel guilty. Individuals with epilepsy are significantly more likely to have medical or psychiatric comorbidities than those without epilepsy, and these comorbidities strongly correlated with negative impacts on subjective health status and quality of life [15-18].
Worldwide, mortality of epilepsy is 2 – 3 times higher than in the general population and it is thought to be higher in developing than developed world particularly in Sub-Saharan Africa. Low socio-economic status, comorbidity like cerebrovascular diseases and neoplasms increase the risk of death from epilepsy in Sub-Saharan Africa than in developed countries. Having epilepsy and receiving antiepileptic drug has a clear impact on self-esteem and Even today, many patients with epilepsy find themselves stigmatized and marginalized. The negative attitude towards patients with epilepsy makes the patients to be excluded socially, drop from school and left without employment [17,19,20].
The treatment gap, (i.e., the difference between the number of people with active epilepsy and those, whose seizures are appropriately treated) is high in low and middle-income countries with overall 56% remain untreated. A study indicated that high proportion of patients with epilepsy (80-90%) in resource-poor countries are not receiving appropriate treatment for their condition and many of them discontinue initiated treatment soon due to medication or non-medication related problems like inadequacy, side effects of medication or poor adherence that may result in decreased quality of life, increases burden of health care, mortality and challenging its management [2,14].
Adherence to medication is vital in preventing or minimizing the frequency of seizures and their increasing impact on everyday life and increase effectiveness of antiepileptic drugs. The most important cause of poorly controlled epilepsy is poor adherence to drug regimen. The magnitude of low adherence to AEDs range from 26.0% to 79%, with increased prevalence in developing countries [21]. Non-adherence to AED is considered as a secondary treatment gap and is an additional burden to the high treatment gap. Patient related factors like forgetfulness and stigmatization, medication-related factors such as cost, side effects, poly pharmacy, dosing frequency and disease related factors like seizure type, severity and duration of illness are common factors influencing medication adherence patients with epilepsy [22].
Non-adherence to AED result in significant worsening of disease, increasing treatment failure, morbidity, mortality, health care costs, time of hospitalization, burden of inpatient and emergency department services and it also affects the family members socially, economically, and psychologically. In epilepsy, unlike some other chronic medical conditions, for which missing several doses of medications may have little or no effect even a single missed dose can cause treatment failure and trigger seizures. Non-adherence to AED result in recurrence of seizure which further result in poor quality of life, reduce productivity, feeling of helpless and seizure related joblessness. The mortality rate of none-adherent patients was three times higher than that of adherent patients. Poor adherence to a viable AEDs introduces to the more complex treatments involving greater toxicity with uncertain prognosis and has significant impact on reduction of mental and emotional wellbeing, including impaired cognition [20,21,23-26].
Even though Epilepsy is a widely recognized health condition, it is still poorly understood, even among people who know someone with the disorder. Adherence to therapeutic medications is critical for epileptic patient so far, the issue of adherence still considered as secondary treatment gap and the most important cause of poorly controlled epilepsy particularly in developing countries. To the best of our knowledge even though stigma surrounding the diseases is high which contributes for significant impact on patient’s adherence to medication there is limited study on medication adherence and associated factors in developing countries particularly in Ethiopia. Therefore, this study aimed to assess medication adherence and associated factors among patients with epilepsy on follow up at Jimma town public hospitals.
Literature Review
Globally epilepsy affects about 50 million people of which 80% live in developing countries. The bad thing is around 40 million people living with epilepsy are not receiving appropriate treatment [7,8]. The magnitude of non-adherence to AEDs range from 26.0% to 79%, with increased prevalence in developing countries [5,21]. A study conducted in USA revealed that 63% of the study participants were adherence to Anti-epileptic drugs. It also shows that there was a significant association between increased seizure frequency, belief about medication and adherence. Another study reports that self-reported adherence was correlated with polytherapy but none of the socio-demographic variables were significantly associated with adherence [27,28]. A cross-sectional study conducted in Kansas, reports that being employed and educational attainment were significantly associated with adherence whereas [29]. The study examined psychosocial correlates of medication adherence in a socio-economically and racially diverse sample of patients with epilepsy at Bellevue Hospital in USA shows that prevalence of adherence to AEDs was 64%. It reports that poor social support is significantly correlated with adherence to AEDs [30]. Study conducted in United Kingdom states that 41% of study participants were adherence to anti-epileptic drugs and a negative correlation between adherence and frequency of seizures [31]. Another study conducted at United Kingdom reports that 63% of the respondents were adherent to AEDs [32]. Systematic review conducted on identifying the barriers to antiepileptic drug adherence in Ireland identifies the adherence to AEDs in Brazil, United States of America and China was 34%, 64% and 60% respectively. It also showed that being woman, types of epilepsy, frequency of seizure in last month, social support, medication belief and monotherapy where significantly associated with AED adherence [32]. A study conducted in China reports that there were no significant association between types of epilepsy, frequency of seizure, social support, medication belief and monotherapy and adherence [33]. Study conducted at Paris France revealed that 79% of respondents were adherent to AEDs and occupational status was negatively associated with AEDs [26]. A cross-sectional study in Palestine, showed that the magnitude of high, medium and low adherence to AEDs were 14.7%, 49.3% and 36% respectively. It reports that adherence to AEDs was positively and significantly correlated with age and duration of illness however, drug regimen and sex of respondents were not significantly associated with adherence to AEDs [34]. A study conducted in Saudi Arabia states that 38.3% of the study participants were adherent to AEDs and the number of drugs, social support, seizure frequency, stronger belief of medication and felt stigmatized were the most important factors that were significantly associated with adherence [35]. A Study conducted in Malaysia found 64.1% non-adherence to AEDs and duration of epilepsy, medication beliefs (uncertainty about necessity of AEDs) and age of respondents were significantly associated with adherence [36]. Another study in Kuala Lumpur Hospital of Malaysia also found high prevalence of non-adherence 49.3% and it revealed that seizure frequency and Payment for medication were significantly associated with medication adherence [37]. Study in Bangalore in India shows that 72.3% of respondents were adherent to AEDs and economic status and type of were significantly associated with adherence [7]. Another study in India revealed that 90.10% of participants were adherent to AEDs and monthly cost of the medications was the main factor that influence medication adherence [38].
A study conducted in China shows there were no significant difference in socio- demographic, clinical and treatment characteristics between the low adherence and the moderate-to-high adherence[33] but, a study conducted in India revealed that age, education status, marital status and poly-therapy had a statistically significant association with self-reported adherence [39]. A cross-sectional study done in China reports that 51.9% of respondents were adhere to AEDs and adherence was significantly associated with duration of illness [20]. Other study conducted in China shows 66.7% of respondents were adherent and there was significant difference in seizure types and number of AEDs and social support between the non-adherent and adherent group [40].
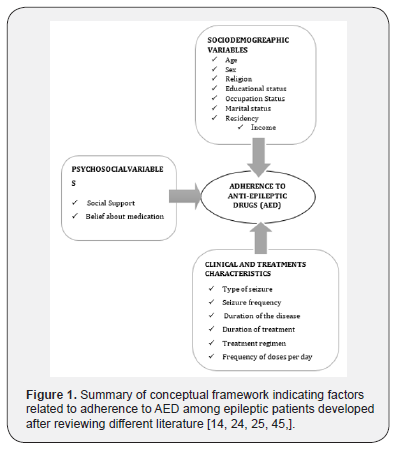
A cross-sectional study conducted among the rural Population of Kolar indicates that 50% of epileptic patients were adherent to AEDs and Gender, social support, educational status, occupation of the patient and no of tablet taken per day where significantly associated with adherence to AEDs [41]. In Kenya study revealed that the adherence to AED was 46% and adherence was significantly associated with duration of treatment [42]. A study conducted at Dilla Ethiopia showed that the rate of adherence to AEDs was 61.9% and ways of getting medication, social support and duration of treatment were found to be significantly associated with antiepileptic drug adherence [25]. A study conducted in Northwest Ethiopia revealed that 62.2% of respondents were adherent to AEDs and duration of treatment, ways of getting medication, social support and stigma were significantly associated with adherence [24] (Figure 1) .
Methods and Materials
The study was conducted in two public hospitals in Jimma town namely Jimma Medical Center (JMC) and Shanan Gibe Hospital (SGH)) from April 08 - May 20/2019.Jimma town is located 357 km in Southwest from Addis Ababa, capital city of Ethiopia. Both hospitals provide inpatient, outpatient, emergency care, maternal and child service and chronic follow clinics. JMC established in 1930, is one of the oldest public hospitals in the country and it is the only referral hospital in the south western part of the country providing service for more than 18 million people with catchment area of 17,500 km2 whereas SGH is a general hospital serving as district level facility [43]. More than 12,384 and 5832 of which 750 and 370 were patients with epilepsy had follow up at chronic clinics of JMC and SGH respectively.
Study design and population
Institution based cross-sectional study was conducted on 297 adult patients with epilepsy who were randomly selected from those on follow up. Those patients taking AEDs at least for three months and no change in AEDs regimen for the past three months were included in the study. Patients with incomplete medical record and individuals who are unable to communicate due to serious neurological deficit and other serious illness were excluded from the study. Proportional allocation followed by simple random sampling was used to select the study subjects. The sample size was calculated using single population proportion formula by taking proportion of adherence from study done in Dilla University Referral Hospital P= 61.9% and then corrected for population less than 10,000 [25].
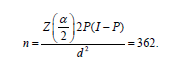
Correction formula: 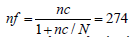 and then considering 10% non-response rate, total sample size is 274+27= 301
and then considering 10% non-response rate, total sample size is 274+27= 301
Data Collection procedures and instrument Data were collected by using structured interviewer (four BSc nurses) administered questionnaire prepared in English and translated to the local languages Afaan Oromo and Amharic by language experts who are fluent in the languages. Patients medical records were retrieved using adopted data abstraction checklist from previous study conducted at JMC [44]. The questionnaire contains four parts: socio-demographic variables, clinical and treatment related factors, psychosocial variables and Morisky 8-item medication adherence scale [45].
Adherence: Measured by eight-item Morisky Medication Adherence Scale (MMAS) that is widely used to measure self-reported adherence adopted from previous study. Items 1-7 are yes/no questions, in which a “no” answer receives a score of 1 and a “yes” answer receives a score of 0, except for item 5, which is reverse scored. Item 8 is measured on a five-point scale. The responses “never”, “once in a while”, “sometimes”, “usually”, and “all the time” are scored, 1, 0.75, 0.50, 0.25, and 0, respectively. Total score ranges from 0 to 8 [25].
The felt stigma: -assessed with the Jacoby Scale (JS) composed of three questions. Each item was a Boolean question (no = 0, yes = 1). The score of the JS is established from the sum of each item [22].
Social support: -assessed by using the Oslo 3-items social support scale in which the first item had 4- point scale and the other two items had 5-point Likert scale. The sum score of this scale is ranged from minimum of 3 to the maximum 14 [24].
Beliefs about medication: Patients’ belief about their medication was assessed using the belief about medicines questionnaire (BMQ), which has been validated for use in different chronic illness group studies [14]. It contains 18 questions in two parts (general beliefs and specific beliefs about drug). In this study, specific belief about the drug, which contains ten items was used. The specific belief explores patients’ beliefs about the medications prescribed for a specific condition (epilepsy) and it contains two parts, specific- necessity which assess patients’ belief about the necessity of the prescribed medications for controlling their illness and specific- concerns which assess their concerns about the potential adverse consequences of taking medication. Each question was scored based on 5-point Likert scale (1-Strongly disagree, 2-Disagree, 3- No comments, 4-Agree, 5- Strongly agree).
Operational definition
Medication Adherence: - Refers to the extent to which a patient’s behavior corresponds with the recommendations of a health professional with respect to timing, dosage, and frequency of medication persistence as the duration of time from initiation to discontinuation of therapy.
Low adherence: -Patients scores < 6 of 8 item MMAS. Medium adherence: - Patients scores 6-7 of 8 item MMAS.
High adherence: - Patients scores 8 of 8 item MMAS.
Overall adherence: - Dichotomized as adherent and non-adherent. In this study individual in category of medium adherence and high adherence taken as adherent and low adherence as non-adherent [14].
Poor social support: - Respondents scores3–8 of Oslo 3-items social support scale.
Moderate social support: -Respondents scores9–11of Oslo 3-items social support scale.
Strong social support: - Respondents scores12–14of Oslo 3-items social support scale [24].
Felt stigmatized: -Respondents scores Jacob stigma scale score = 0
Not felt stigmatized: -Respondents scores Jacob stigma scale score > 0 [22].
Strong medication necessity belief: -Respondents scores mean and above of the five-item medication necessity scale score.
Low medication necessity belief: - Respondents scores below mean of the five-item medication necessity scale score.
Strong medication concern belief: -Respondents scores mean and above of the five-item medication concern scale score Low medication concern belief: -Respondents scores below mean of the five-item medication concern scale score [14].
Data processing and analysis
After checked for complete ness and cleaned the data were entered into Epi data version 3.5.3 and exported to SPSS version 23.0 for analysis. Descriptive statistics was used to describe the data and variables with p-value <0.25 on bivariate analysis were candidate for multivariate analyses. Finally, variables with p-value < 0.05 on multivariate analyses were considered as statistically significant.
Ethical consideration
Ethical clearance was obtained from the Institutional Review Board (IRB) of Jimma University, Institute of Health, Faculty of Health Science. Official letter was obtained from Research and Postgraduate Coordinating office to JMC and SGH. Informed consent was obtained from the respondents after the aim of the study was briefly explained to them. All information obtained from the patients and records were kept confidential.
Results
Socio-demographic characteristics of the study participants.
Out of the calculated sample of 301 patients, 297 were included in the study giving a response rate of 98.7%. From a total study participant, 169 (56.9%) were male. Almost half 145 (48.8%) of the study participants were in the age category of 18-25 year followed by 70 (23.6%) in26-33 year. Regarding their occupation 111(37.4%) respondents were farmers. Ninety-five (32%) of the study participants were illiterate. About three-fourth of respondents 191 (64.3%) were rural residents. More than half 175 (58.9%) and less than one-third 91(30.6%) of respondents had an income of <500 and >1000 Ethiopian Birr respectively (Table 1).
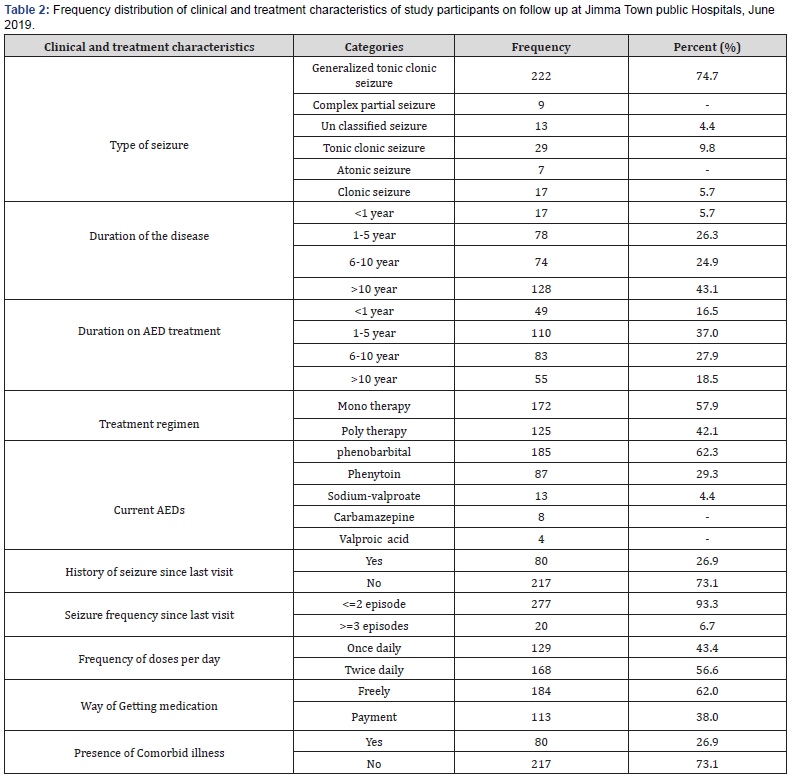
Clinical and treatment related variables
Majority, 222 (74.7%) of the study participants had generalized tonic clonic seizures. Less than half 128 (43.1%) respondents had disease for more than 10 years. More than one third of the respondents 110 (37.0 %) had treatment for 6-10 years. Regarding number of medications 172(57.9%) were on mono therapy regimen. Around two-third of the study participants 185(62.3%) were taking Phenobarbital followed by phenytoin which accounts for 87(29.3%). Concerning episodes of seizure 80(26.9%) of respondents were experiencing seizures since their last visit with most of them had experiencing one and two episodes of seizure. With regard to frequency of medication 129(43.4%) participants take their drugs once daily. Most of respondents, 184(62.0%) respondents were getting medication freely. Of total respondents 217 (73.1%) had no co morbid illness (Table 2).
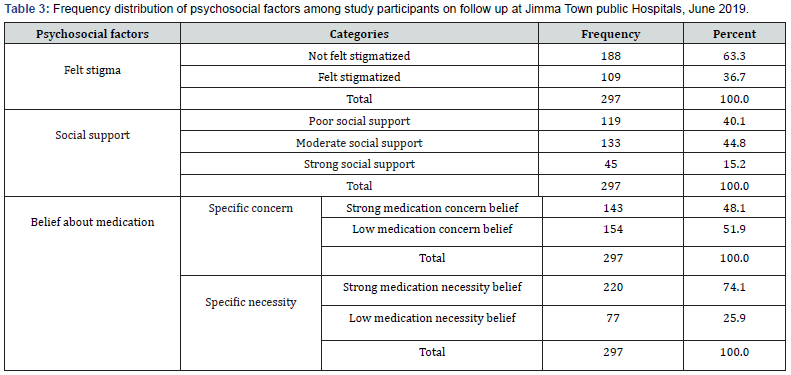
Psychosocial factors
More than one-third 109(36.7%) of respondents reported they had felt stigma. About 133(44.8) and 119(40.1%) respondents had moderate and poor social support respectively. Around three-fourth 220(74.1%) of the study participants had strong medication necessity belief. Less than half143(48.1%) of the respondents had strong medication concern belief (Table 3).
Level of medication adherence among study participants
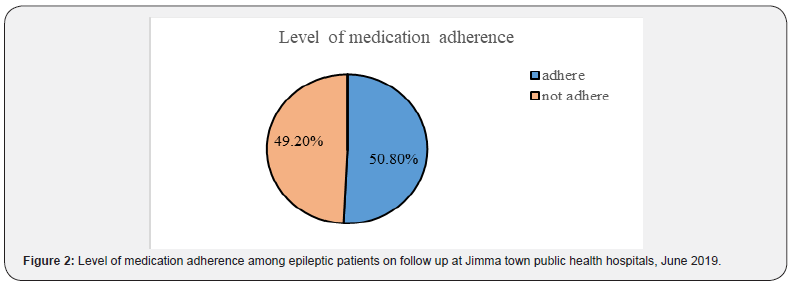
The study revealed that 50.8% of the patients reported to have good adherence to anti-epileptic medications (Figure 2).
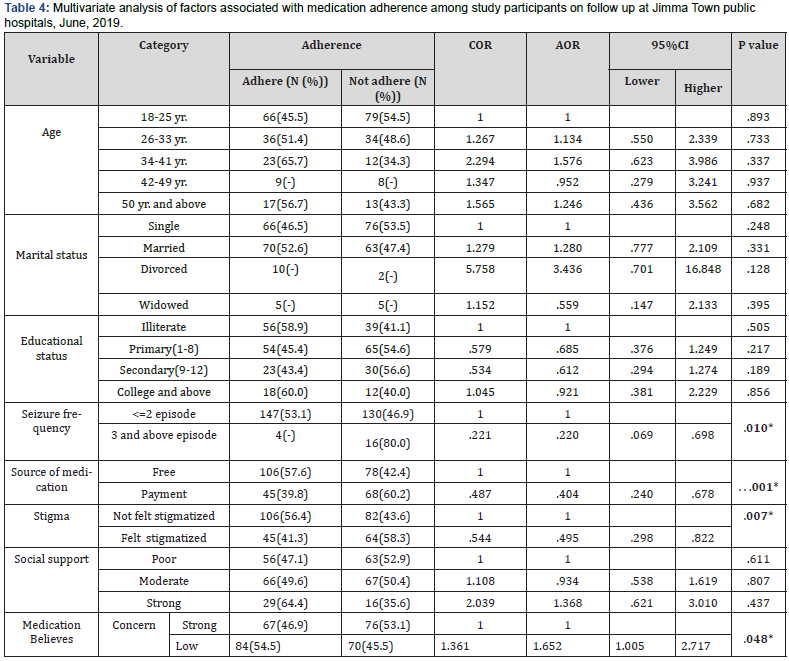
Factors associated with adherence to Antiepileptic drugs
After identifying candidate variables in binary logistic regression, we run multivariate logistic regression analysis and the result indicate that variables such as source of medication (AOR=0.404, 95% CI: 0.240-0.678, P- .001), felt stigma (AOR=0.495, 95% CI: 0.298-0.822, P- .007), seizure frequency (AOR=0.220, 95% CI: 0.069-0.698, P- .010) and medication concern belief (AOR=1.652, 95%CI: 1.005-2.717, P- .048) were significantly associated with medication adherence. Study participants who were getting their medication by payment were 59.6% less likely to adhere to AED than those who were getting their medication freely (AOR=0.404, 95% CI: 0.240-0.678, P- .001). Respondents who reported having felt stigmatized due to their disease were 50.5% times less likely to adhere to AED than those who were not felt stigmatized (AOR=0.495, 95% CI: 0.298-0.822, P- .007). Respondents who had experienced three and more episodes of seizure since their last visit were 78% times less likely to adhere to AED than those who had experiencing two and less episodes of seizure (AOR=0.220, 95% CI: 0.069-0.679, P- .010). The study participants who had low medication concern belief about adverse consequences of the prescribed medication were 1.65times more likely to be adherent to AED than those who had strong medication concern belief about adverse consequences of medications (AOR=1.652, 95%CI: 1.005- 2.717, P- .048) (Table 4).
Discussion
Adherence to medication is vital in preventing or minimizing the impact of disease on everyday life and increase effectiveness of antiepileptic drugs. This cross-sectional study assessed the level of medication adherence to AED among patients with epilepsy and show that 50.8% of study participants were adherent to anti-epileptic medications. In line to this study, study conducted in Malaysia (37), China (20), and India (42) found that, 50.7%, 51.9% and 50% of respondents were adherent to anti-epileptic medications respectively. However the finding our study is lower than study conducted in USA (27), Paris (26), India (7), China (40), United Kingdom (32), Dilla University Referral Hospital (25) and Northwest Ethiopia (24) which states 63%, 79%,72.3%, 66.7%, 79.5% 61.9% and 62.2% of the study participants were adherent to anti-epileptic medications respectively. This discrepancy in finding might be due to difference in socio-demographic status of study participants, difference in sample size, number of prescribed medications, side effects and frequency of medication, severity of the disease etc. It might also be due to variation in availability of medication and accessibility to health care.
Adherence to AEDs in this study is higher than study conducted in United Kingdom (31), Brazil (32), Riyadh National Hospital (35), Malaysia (36), and Kenya (43) in which 41%, 34%, 38.3%, 35.9% and 46% of the study participants were adherent to antiepileptic medications respectively. This discrepancy might be due to difference in study period and sample size used, difference in cut point of adherence level. In this study, ways of getting medication and seizure frequency were significantly associated with adherence to AEDs. In line to this, study conducted in Malaysia shows that seizure frequency and payment for medication were significantly associated with adherence to AEDs [37]. Similarly, study conducted in USA (27), Ireland (32), South east Asia (22) states that frequency of seizure since last month of their visit were significantly associated with adherence. Study carried out in Indian (38) and Northwest of Ethiopia (Debre Markos and Finote Selam Hospitals) (24) revealed that monthly cost (payment) was significantly associated with adherence. The consistency in finding might be due to the facts that most of developing counties are sharing economic problems, which has its own impact on adherence to AEDs related to ways of getting medication.
In contrast to this study, study conducted in China (33,41), and Malaysia (36) found that frequency of seizure was not significantly associated with adherence to AEDs. Discrepancy in the finding might be due to difference in sample size and socio-demographic characteristics of the study participants. In this study, felt stigma was significantly associated with adherence to AEDs. In line to this, study conducted in Riyadh National Hospital Saudi Arabia (35) and Northwest Ethiopia (24) revealed that felt stigma was significantly associated with adherence. In contrast to our finding, study conducted in India shows no significant association between adherence and stigma [38]. The probable reason for difference in the finding may be due to difference in socioeconomic status of study participants and sample size.
Medication concern belief of adverse effects of medication were significantly associated with adherence to AEDs. This finding was supported by a study conducted in Ireland, which states medication concern belief of adverse effects of medication was significantly associated with adherence to AEDs [32]. In contrast to this, study conducted in Bellevue Hospital in USA (30), china (32) and Riyadh National Hospital in Saudi Arabia (35) revealed that there were no significant association between concern about adverse effect of medication adherence. The inconsistency in the finding may be due to difference in educational status of study participants.
Limitation of the study
i. The level of adherence may be overestimated or underestimated since the measures relied on self-reporting
ii. The cross-sectional design of the study fails to assess patients’ adherence behaviors over time.
Conclusion
Even though Medication adherence remains an important issue in epilepsy treatment, this study found that about half of the study participants had good adherence to anti-epileptic medications and some factors were found to be significantly associated with adherence. Among the variables studied payment for medication, felt stigma, having more episodes of seizure and strong medication concern belief of adverse effect of medication were factors contributed for low adherence to AEDs. Providing medication is not enough for epilepsy management, rather assessment of medication adherence among patients with epilepsy should be a routine part of epilepsy management. Moreover, the high rate of non-adherence in this study calls for researchers to do further large-scale longitudinal studies to provide adequate evidence about the cause-effect relationship between the predictor variables and adherence. Nurses and other health care providers should provide health education and medication related counseling for all patients with epilepsy to improve adherence.
Implications for Nursing Practice
As the finding of this study indicated nearly half of the patients with epilepsy have poor adherence to anti-epileptic medications. Therefore, as nurses are the front-line health professionals who frequently meet and care for these chronic patients this finding is alerting for nurses. Nurses should teach and counsel the patients and their families/care givers about the importance of good adherence and consequences of poor adherence to the medication.
Acknowledgement
The authors of this study would like to forward our deepest gratitude to Jimma University, respective data collectors and staff of chronic follow up clinics of both hospitals. Finally, we thank all individuals and colleagues who directly or indirectly contributed in this paper.
Conflict of interest
The authors of the study confirmed that there is no financial and other type of conflict of interest in this paper.
Funding
This study was funded by Jimma University, Ethiopia and the funder has no interference with the conduction, analysis and publication process.
Authors’ contribution
EA is a principal investigator of this study while TD and AA were involved in the study initiating/conceptualization, designing, and interpretation of finding with EA. AA and EA done the analysis and prepared and reviewed the manuscript for publication. All of the authors have read and approved the manuscript for publication. AA formulated methodology and a corresponding author for publication.
References
- Suzanne C, Dubendorf P (2010) Brunner & Suddarth’s Textbook of Medical-Surgical Nursing. (12th Edn),Thieme Medical Publishers, pp. 1875-1882.
- (2018 ) World health orginization epilepsy fact sheet.
- Kasper D (2018) Internal Medicine. 20thEdnEdward C (Ed.), Elsevier Inc, pp. 523-534.
- Longo’s DF (2008) Harrison’s Principles of Internal Medicine. 17th McGraw-Hill, USA, pp. 2046-2050.
- Smith F, Clifford S (2011) Adherence to medication among chronic patients in Middle Eastern countries. East Mediterr Heal J17(4):356–362.
- Chinnaiyan S, Narayana S, Nanjappa VP (2017) Adherence to Antiepileptic Therapy in Adults. J Neurosci Rural Pr8(3):417–420.
- Gurumurthy R, Chanda K (2017).An evaluation of factors affecting adherence to antiepileptic drugs in patients with epilepsy. Singapore Med J58(2):98–102.
- Fiest KM, Sauro KM, Wiebe S, Patten SB, Dykeman J, et al. (2016) Prevalence and incidence of epilepsy A systematic review and meta-analysis of international studies. Am Acad Neurol 88(3):296–303.
- Report MW (2013). National Epilepsy Month. Morbidity and Mortality Weekly Report 62.
- Escoffery C (2017) Development of the Adult Epilepsy Self-Management Measurement Instrument. Epilepsy Behav50:172–183.
- Mbuba CK, Newton CR (2009) Packages of Care for Epilepsy in Low- and Middle-Income Countries. PLoS Med6(10):1–5.
- (2018) WHO. Epilepsy 8 [Internet]. epilpsy and behaviour, Genava.
- Mugumbate J, Zimba AM (2018)Epilepsy in Africa: Past, present, and future. Int Bur Epilepsy79:239–241.
- Niriayo YL, Mamo A, Kassa TD, Asgedom SW, Atey TM, et al. (2018).Treatment outcome and associated factors among patients with epilepsy. Sci Rep 8(1) : 173-175.
- Shahar MA, Omar AM, Hasmoni MH (2017) Assessment of Knowledge , attitude and practices of Epilepsy Patients ’ towards their illness and treatment in a tertiary care hospital in Kuantan. J Med Sci 16(4):545–553.
- Boling W,Fletcher A (2018)Quality of Life and Stigma in Epilepsy, Perspectives from Selected Regions of Asia and Sub-Saharan Africa. Brian Sci8(59):1–11.
- Kerr MP (2012)The impact of epilepsy on patients ’ lives. Acta Neurol Scand Suppl 194:1–9.
- Manacheril R, Faheem U, Labiner D, Drake K, Chong J (2015)Psychosocial Impact of Epilepsy in Older Adults. Healthcare (Basel)13(2):1271–1283.
- Hills MD (2007)The psychological and social impact of epilepsy. Neurol Asia12(Supplement 1):10–2.
- Liu J, Liu Z, Ding H, Yang X (2013) Adherence to treatment and influencing factors in a sample of Chinese epilepsy patients. Epileptic Disord15(5):289–294.
- Liu J, Xu R, Liu Z, You Y, Meng F (2015) Factors influencing medication adherence. Epileptic Disord 17(1):47–51.
- Harimanana A (2013) Associated factors with adherence to antiepileptic drug. Epilepsy research104(1-2):158-166.
- Hixson J (2017)Self-Management in Epilepsy Care : Background , Barriers , And Solutions. Eur Med J 54–60.
- Getnet A, Woldeyohannes SM, Bekana L, Mekonen T, Fekadu W, et al. (2016) Antiepileptic Drug Nonadherence and Its Predictors among People with Epilepsy. Behav Neurol 1–6.
- Shegaw MR,Kassa R, Ali Y, Addissu N (2017) Prevalence and Associated Factors of Antiepileptic Drugnonadherence Among Epileptic Patients Attending at Out Patient Departement of Dilla University Referral Hospital, Dilla,gedeo,snnpr, Southern Ethiopia. Int J Biosci Med1-2:1–11.
- Laville F, Roux N, Rathelot, Giorgi, Vanelle, et al (2018) Factors limiting adherence to antiepileptic treatment : A French online patient survey. J Clin Pharm pharmatutical43:73–79.
- Nakhutina L, Gonzalez JS, Margolis SA, Spada A, Grant A (2011) Adherence to antiepileptic drugs and beliefs about medication among predominantly ethnic minority patients with epilepsy. Epilepsy & Behavior22(3):584-586.
- Carbone L, Zebrack B, Plegue M, Joshi S, Shellhaas R (2013)Treatment adherence among adolescents with epilepsy: what really matters?.Epilepsy & Behavior27(1):59-63.
- Paschal AM, Rush SE, Sadler T (2014). Factors associated with medication adherence in patients with epilepsy and recommendations for improvement. Epilepsy & Behavior 31:346-350.
- Shallcross AJ, Becker DA, Singh A, Friedman D, Jurd R,et al (2015) Psychosocial factors associated with medication adherence in ethnically and socioeconomically diverse patients with epilepsy. Epilepsy and Behavior46: 242–245.
- Jones RM, Butler JA, Thomas VA, Peveler RC, Prevett M (2006) Adherence to treatment in patients with epilepsy : Associations with seizure control and illness beliefs. Gaziantep Med J 504–508.
- Rourke GO, Jordan J, Brien O (2017) Identifying the barriers to antiepileptic drug adherence among adults with epilepsy. Seizure Eur J Epilepsy 45: 160–168.
- Guo Y, Ding X, Lu R, Shen C, Ding Y, et al (2015) Depression and anxiety are associated with reduced antiepileptic drug adherence in Chinese patients. Epilepsy andBehav50:91–95.
- Sweileh WM, Ihbesheh MS, Jarar IS, Abu AS, Sawalha AF et al (2011) Self-reported medication adherence and treatment satisfaction in patients with epilepsy. Epilepsyand Behavior21(3):301–305.
- Gabr WM, Shams ME (2015) Adherence to medication among outpatient adolescents with epilepsy. Saudi Pharm J23(1):33–40.
- Tan XC, Hons BP, Lau CL, Clin PM, Mpharm FWT, et al. (2015) Factors affecting adherence to antiepileptic drugs therapy in Malaysia. Neurol Asia20(3):235–241.
- NagashekharaK, Murthy L, Mruthyunjaya AT (2016) Evaluation of self ‑ reported medication adherence and its associated factors among epilepsy patients in Hospital Kuala Lumpur. J Basic Clin Pharm7(4):105–109.
- Honnekeri B, Rane S, Vast R, Khadilkar S V (2018). Factors Affecting Medication Adherence in Epilepsy Patients. J Assoc Physicians Indi 66:24–27.
- PashaM, Debdipta (2017) Assessment of factors influencing self reported drug adherence to anti- epileptic drugs at a tertiary care hospital. Int J Res Pharmacol Pharmacother 6(2):163–169.
- Wang S, Chen C, Jin B, Yang L, Ding Y, et al (2017) The association of psychosocial variables with adherence to antiepileptic drugs in patients with temporal lobe epilepsy. Epilepsy andBehavior77:39–43.
- Chinnaiyan S, Narayana S,Nanjappa VP (2017) Adherence to Antiepileptic Therapy in Adults. J Neurosci Rural Pr8(3):417–420.
- Mbuba CK, Ngugi AK, Fegan G, Ibinda F, Muchohi SN, et al (2012) Risk factors associated with the epilepsy treatment gap in Kilifi , Kenya : a cross-sectional study. Lancet Neurol11(8):688–696.
- Gurshaw M, Agalu A, Chanie T (2014) Anti-epileptic drug utilization and treatment outcome among epileptic patients on follow-up in a resource poor setting. Gaziantep Med J6(3):47–52.
- Hiwot G, Nezif D, Sofia A, Alinur M, Mohammed A (2014) Medication adherence in epilepsy and potential risk factors associated with non adherence in tertiary care teaching hospital in southwest Ethiopia. Gaziantep Med J 20(1):59–65.
- AbarayaM, Seid Sh, AmenSh (2018) Determinants of preterm birth at Jimma University Medical Center. doves Press J 9:101–107.






























