Evaluation of Drug Utilization pattern in Ocular Diseases with Respect to Pharmacoepidemiology in Outpatient
Jarinabanu Tahashildar1
, Ravi Shekhar singh 2* and Jameela Tahashildar31Department of Pharmacology, Dr.D.Y. Patil. Medical College, Kolhapur, India
2Department of Pharmacology, Dr. P.D.M. Medical college, India
3Department of Pharmacology,GM C Udaiur, India
Submission: January 22, 2019;Published: April 17, 2019
*Corresponding author: Ravi Shekhar Singh, Department of Pharmacology, Dr. P.D.M.Medical college, Amravati, India
How to cite this article: Jarinabanu Tahashildar, Ravi Shekhar singh, Jameela Tahashildar. Evaluation of Drug Utilization pattern in Ocular Diseases with Respect to Pharmacoepidemiology in Outpatient. J of Pharmacol & Clin Res. 2019; 7(1): 555703. DOI: 10.19080/JPCR.2019.07.555703
Abstract
Objective: Eye is very important sensory organ in the body. Eye complaints are common in general practice and some of them, if neglected leading to blindness. so, the establishments of an effective eye care delivery system for the treatment of eye diseases and prevention of blindness is linked to the existing general services and resources available. The objective of this work is to study and assess the patterns of prescription and drug utilization by specific drug use indicators in respect to pharmacoepidemiology, in ophthalmology outpatient department of a tertiary care teaching hospital.
Materials and Methods: The data of 600 cases was collected to record the required information from the OPD drug prescription cards of each patient including patient’s demographic details. All the drugs prescribed recorded including its dosage form, route of administration, frequency of administration, indication for which prescribed, duration of therapy. The data recorded was analyzed by WHO/INRUD Core Drug Use Indicators and additional indices.
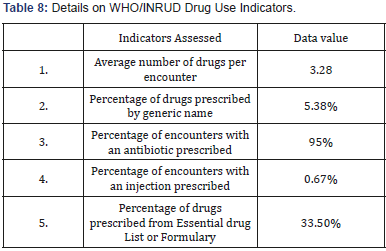
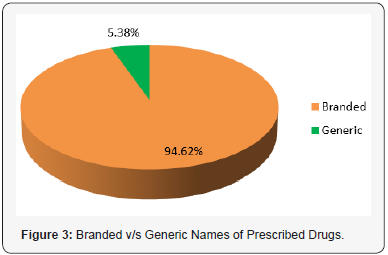
Result: The average number of drugs per prescription was 3.28. Percentage of drug prescribed by generic name was only 5.38%. Percentage of encounters with antibiotics was 95%. percentage of encounter with injections was 0.67%. Percentage of drugs prescribed from National Essential Drug List was only 33.50%.
Conclusion: This study of prescription analysis gives a message to the prescribing ophthalmologist to achieve rational and safe effective health care.
Keywords: Ocular diseases; Pattern of Drug Utilization
Introduction
Eye is very important sensory organ in the body. Eye complaints are common in general practice and some of them, if neglected leading to blindness [1] So the establishment of an effective eye care delivery system for the treatment of eye diseases and prevention of blindness is linked to the existing general services and resources available [2]. So optimum management of ocular diseases has large impact in prevention of loss of vision in patients suffering from eye problems. Appropriate management of these patients reduces the burden of the ocular health problem [3]. In recent years, drug utilization studies are powerful exploratory tools to ascertain the role of drugs in society [4] and their assessment is important for clinical, educational and economic purposes [5]. The drug utilization pattern needs to be evaluated from time to time so as to increase therapeutic efficacy and decrease adverse effects [6]. Drug utilization study is an essential part of pharmacoepidemiology, which describes the extent, nature and determinants of drug exposure. To improve the overall drug use, especially in developing countries, international agencies like World Health Organization (WHO) and International Network for Rational Use of Drugs (INRUD) have applied themselves to evolve standard Drug Use Indicators [7] based on the field testing which are done in the following 12 developing countries Indonesia, Bangladesh and Nepal: other tests took place in Guatemala, Malawi, Nigeria, Tanzania and well as in Ecuador, Sudan, Uganda, Yemen and Zimbabwe. Results of which identified lacunae like polypharmacy, low prescribing by generic names and essential drug list, also overuse of antibiotics and injections [8].
Drug utilization studies have been conducted in a different discipline of medicine and institutes/health care facilities in India [4,9-12] and also abroad [13,14] Drug utilization studies have been conducted in a different discipline of medicine and institutes/health care facilities in India [9-12] and also abroad [13,14]. Looking into increasing importance of drug utilization studies, there was a need to conduct a similar study in the field of ophthalmology in our hospital. The present study was undertaken to evaluate the pattern of drug utilization in respect to pharmacoepidemiology, and current prescribing practices of the ophthalmologist using WHO/INRUD basic indicators. This data provide feedback to the prescribers; identify and decide interventions to improve drug use to ensure rational use of medicines. it will also provide the hospital authorities a baseline data for development of Drug Policy and Standard Treatment Guidelines to ensure rational utilization of drugs ultimately benefiting the society
Aims and Objectives
Primary objective
To obtain baseline data of current prescribing practices in ophthalmology outpatient using the following WHO/INRUD indicators.
a. Average number of drugs per encounter/prescription
b. Percentage of drugs prescribed by generic name
c. Percentage of encounters with an antibiotic prescribed
d. Percentage of encounters with an injection prescribed
e. Percentage of drugs prescribed from Essential Drug List
Secondary objective
To study the most commonly used drugs is respect to the following:
a. Pharmacoepidemiology
Material and Methods
This “Drug Utilization study in ophthalmology outpatients” was conducted in outpatient department of Ophthalmology of Geetanjali Medical College & Hospital, a Tertiary care teaching hospital, Udaipur. Approval of Ethics Committee was obtained from Institutional Ethical Committee and permission to carry out the study was obtained from the Professor and Head, Department of Ophthalmology of Geetanjali Medical College & Hospital, Udaipur. This study was open label, prospective, cross sectional, descriptive type of observational study. The study was conducted in Outpatient department of Ophthalmology Geetanjali Medical College & Hospital, a Tertiary care teaching hospital, Udaipur. Patients attending Ophthalmology outpatient department, of Ophthalmology Geetanjali Medical College & Hospital, Udaipur. Duration of study was 2013-2014. Sample n = 600 (According to WHO/INRUD manual “How to investigate drug use in Health Facilities”).
Inclusion criteria
Patients of both sex and any age attending OPD of Ophthalmology with newly registered during study period.
Exclusion criteria
Patients with follow-up cases, Diabetic retinopathy, Hypertensive retinopathy, Cataract, Refractive errors, Patients not willing to give verbal/written consent, Glaucoma. The purpose and the details of the study were explained to the participants who met the inclusion criteria in Hindi language, after which Verbal/Written informed consent was taken from the participants and then enrolled in the study.
Methodology
Data was collected prospectively from prescriptions of the patients visiting outpatient department of Ophthalmology of Geetanjali Medical College & Hospital from 10.00 AM to 1.00 PM during the study period. A total of 600 patients’ prescription during the course of the study after fulfilling inclusion and exclusion criteria was included in the study and audited. The data of 600 cases was collected to record the required information from the OPD drug prescription cards of each patient including patient’s demographic details (name, age, sex, occupation and address). All the drugs prescribed recorded including its dosage form, route of administration, frequency of administration, indication for which prescribed, duration of therapy. The data recorded was analyzed by WHO/INRUD Core Drug Use Indicators and additional indices. To obtain baseline data of current prescribing practices in outpatient department of Ophthalmology, the following WHO/ INRUD indicators were applied
a. Average number of drugs per encounter/prescription: Helps to evaluate the degree of polypharmacy.
b. Percentage of drugs prescribed by generic name: Helps to evaluate the tendency to prescribe by generic name.
c. Percentage of encounters with an antibiotic prescribed: Helps to evaluate the overall level of use of the most important, but commonly overused and costly form of drug therapy.
d. Percentage of encounters with an injection prescribed: Helps to evaluate the overall level of use of the most important, but commonly overused and costly form of drug therapy.
e. Percentage of drugs prescribed from essential drug list: Helps to evaluate the degree to which practices conform to national drug policy, as indicated by prescribing from the national essential drug list or formulary. (National Essential Drug List, Government of India 2003 was taken as reference).
Additional Parameters
Percentage of antibiotics prescribed: Helps to evaluate the degree and extent of antibiotic use.
Percentage of antibiotics prescribed from essential drug list: Helps to evaluate the degree to antibiotic practices conform to national drug policy, as indicated by prescribing from the national essential drug list.
Commonest class and type of antibiotic prescribed: Helps to evaluate the frequently prescribed antibiotics.
The distribution of diseases treated with antibiotics: Helps to evaluate the frequency of usage of antibiotics in different ocular conditions. Percentage of fixed dose combination of drugs prescribed, and most frequently prescribed fixed dose combination.
Observations and Results
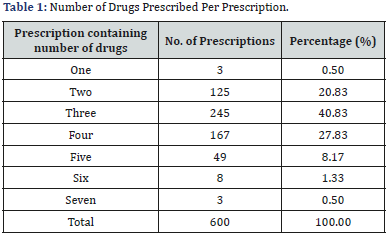
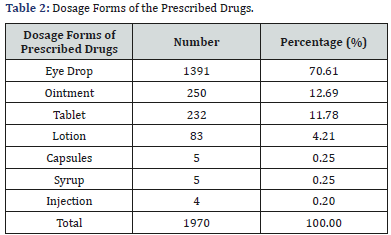
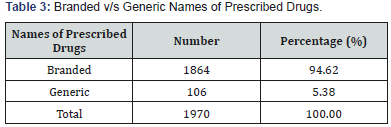
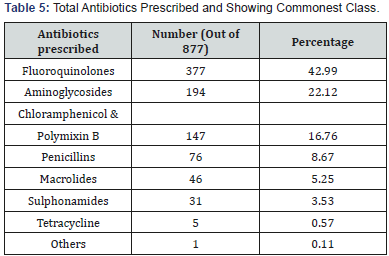
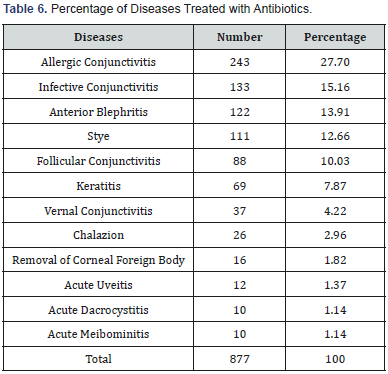
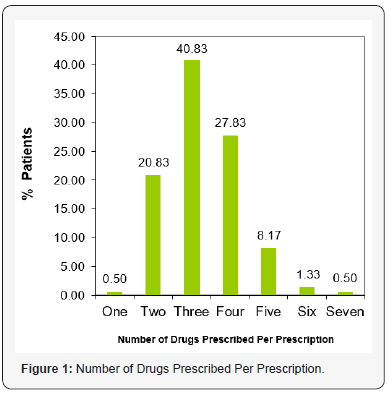
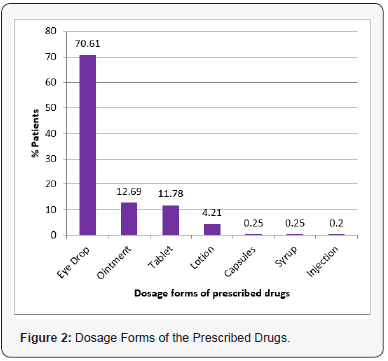
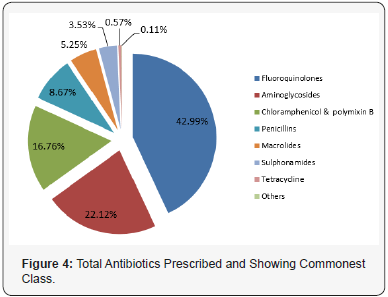
In this study, the total 600 patient’s prescriptions were analysed. Out of 600 patients, 348 (58%) were from urban area, 252 (42%) from rural area. The demographic profile showed that out of total 600 patients, 337 (56.17%) were males and 263 (43.83%) were females. Distribution of patients according to age was studied. The age of the patients was ranged from pediatric to geriatric group. The maximum number of patients belong to the age group of 30-60 years. Study of distribution of the patients according to occupation shows that the maximum number of patients belonged to dependents followed by students, job holders, business people, labours and health care professionals. Distribution of diseases treated in the OPD showed that Allergic Conjunctivitis 260 (43.33%) was the most common disease. Infective Conjunctivitis 84 (14.00%) was the second most common condition followed by Anterior Blephritis 74 (12.33%), Stye 45 (7.50%), Vernal Conjunctivitis 36 (6.00%), Follicular Conjunctivitis 33 (5.50%), Keratitis 24 (4.00%), Chalazion 15 (2.50%), Anterior Uvietis 11 (1.83%), Corneal Foreign Body 8 (1.33%), Acute Meibominitis 6 (1.00%), Acute Dacrocystitis 4 (0.67%). In this study the total number of drugs prescribed in 600 patients were one thousand nine hundred seventy (1970). The number of drugs per prescription varied from 1 to 7. The average number of drugs per prescription in this study was 3.28 (Table 1 & Figure 1). Drugs were prescribed in seven different dosage forms. Eye drops were the most commonly prescribed dosage forms 1391 (70.61%) followed by Ointments 250 (12.69%), Tablets 232 (11.78%), Lotion 83 (4.21%), Capsules 5 (0.25%), Syrup 5 (0.25%), Injection 4 (0.20%) out of total 1970 dosage forms (Table 2 & Figure 2). In our study the frequency and dosage were mentioned 100% but duration of treatment was 99.39%. In frequency and dosage, even the tapering dosage of corticosteroids in a very well manner and easily understanding way to the patient were prescribed. Out of 1970 prescribed drugs, 1864 (94.62%) drugs were prescribed by brand name and only 106 drugs were prescribed by generic name. thus, the percentage of drugs prescribed by generic name was only 5.38 (Table 3 & Figure 3). Use of antibiotics was frequent and number of encounters with antibiotics was 570 out of 600 cases. Thus, the percentage of encounters with antibiotics was 9. Use of injections was minimal and number of encounters with injection was 4 out of 600 cases. Thus, the percentage of encounters with injections was 0.67%. Out of 1970 prescribed drugs, only 660 drugs were from Indian National essential drug list 2003 and 2011. thus, the percentage of drugs prescribed from National Essential drug list was 33.50%. Total drugs prescribed in the 600 patients were 1970. Antibiotics were the most commonly prescribed drugs 877 (44.52%), Lubricants 444 (22.54%) was the second most common drugs prescribed, Antihistaminics were at third position 294 (14.92%) followed by Steroids 108 (5.48%), Anti-dandruff (Baby Shampoo) 81 (4.11%), Non-steroidal Antiinflammatory Drugs 77 (3.91%), Mydriatics 23 (1.17%), Anti-allergic 18 (0.91%), Anti-viral Agents 14 (0.71%), Immunosuppresants 12 (0.61%), H2 Receptor Blocker 10 (0.51%), Normal Saline 7 (0.36%) and Ocular Decongestants 5 (0.25%) (Table 4). Antibiotics constituted (877) 44.52% of the total number of drugs prescribed (1970). Out of 877 prescribed antibiotics, 564 (64.31%) were prescribed as Fixed Dose combination with other agents. Out of 877 prescribed antibiotics, only 158 antibiotics were from Indian National Essential drug list 2003 and 2011. thus, percentage of antibiotics prescribed from Essential drug list was 18.02%. Commonest Class and Type of Antibiotic Prescribed (Most Commonly Prescribed Antibiotic): The most common class of antibiotic prescribed was Fluoroquinolone and constituted 42.99% of the total antibiotics prescribed in this study, of which Moxifloxacin was the most frequently prescribed antibiotic (Table 5 & Figure 4). Total number of antibiotics prescribed for Allergic Conjunctivitis 243 (27.70%), Infective Conjunctivitis 133 (15.16%), Anterior Blepharitis 122 (13.91%), Stye 111 (12.66%), Follicular Conjunctivitis 88 (10.03%), Keratitis 69 (7.87%), Vernal Conjunctivitis 37 (4.22%), Chalazion 26 (2.96%), Corneal Foreign Body Removal 16 (1.82%), Anterior Uveitis 12 (1.37%), Acute Dacrocystitis 10 (1.14%) and Acute Meibominitis 10 (1.14%) (Table 6). As observed in this study, most of the cases were treated empirically without culture and sensitivity request. Total Prescribed Fixed Dose Combinations and Most Commonly Prescribed Fixed Dose Combinations: Out of total 1970, 649 (32.94%) were prescribed fixed dose combinations. Tobramycin and Fluorometholone was the most frequently prescribed fixed dose combination (Table 7). WHO has suggested five core prescribing indicators to evaluate the rationality of drug use? The details of WHO/INRUD indicators are summarized (Table 8).


Discussion
Drug utilization studies are important for obtaining data about the patterns and quality of use, the determinants of drug use and the outcomes of use. The main aim is to facilitate the rational use of medicines in the population. For developing countries like India, a national drug policy is needed to rationalize the drug use. To achieve this, it is very important to determine drug use patterns and monitor drug use profiles over time. Drug prescriptions form a very important point of contact between the health care provider and the user [15]. It provides an insight into the nature of health care delivery system and reflects physician’s attitude towards the disease and the role of drug in its treatment. There has been development of new therapeutic agents which have made it possible to cure or provide the symptomatic control of many clinical disorders. However, in many circumstances’ drugs are not used rationally for optimal benefits and safety [16]. Therefore, pharmacoepidemiology can be a powerful tool that can benefit the patient and public health but only if used appropriately by providing the insights into various aspects of drug prescribing. The present study is mainly to describe current prescribing pattern and drug use by application of WHO/INRUD core indicators, which are highly standardized and highly recommended rather than attempting to judge individual prescription as rational or irrational and also to provide the baseline data for further investigations or qualitative research in order to determine the main factors which contribute to inappropriate prescribing behaviour. This study would also serve as the basis for follow-up intervention. This study is the part of prescription auditing.
As per pharmacoepidemiology in drug utilization studies, our study has covered a wide variety i.e. large number of people both from urban as well as rural area, both sexes and all ages from paediatric to geriatric age group. So, the drugs are widely used in large number of people and their side effects/benefits are analysed among them. After screening 600 OPD patient’s prescriptions, it was found that there was no sex preponderance. So male: female = 1.2:1 among the patients and the maximum number of patients belonged to age group of 30-60 years in OPD. These findings showed that the eye diseases are usually not sex linked but may be age related. As aging causes a gradual decrease in the secretion from the various glands of the eye and ultimately affects the stability of tear film, which is important for clear vision and comfort of the eye. Tear instability may be the result of several diseases [2] and also causes dry eye which is prone for allergy as well as infection. The economic status of the patients revealed that most of the patients are dependents and students. Dependents mean those who are not independent economically and their health care expenditure is one more additional economic burden on the family.
In our study allergic conjunctivitis (43.33%) was the most common disease among distribution of diseases treated in OPD. The other studies showed infective conjunctivitis was the commonest disease in different regions across India [17]. Due to dry humid environment, dust, more of pollution due to marble mining, allergic conjunctivitis is common in our region. The average number of drugs per prescription is an important index as it tends to measure the degree of polypharmacy. It provides scope for review and educational interventions in prescribing practices. In our study the average number of drugs per prescription was 3.28, which shows polypharmacy [7]. Other hospital-based studies in India reported 3-5 drugs per prescription [10,18- 20]. Earlier study done at New Delhi reported (3.03) [18] which is almost the same range of our study or a little lower than our study. While studies done at Jammu (1.87) [15] and Karnataka (2) showed lower number of drugs per prescription than our study.
It is preferable to keep the number of drugs per prescription as low as possible, since higher figures leads to increased risk of drug interactions, adverse effects, development of bacterial resistance, increased cost to patients and errors of prescribing. In this study most commonly prescribed dosage formulation were eye drops. The results were like other studies done at New Delhi, Jammu and Karnataka also had eye drops at the top of the list [15,18]. This shows that most of the drugs are commonly prescribed by topical route in our study (87.77%). This finding supports the use of topical preparation for treating eye disease as they have site specific action, less systemic absorption resulting in fewer side effects and convenient for patients to use [21]. In our study the percentage of drugs prescribed by generic name was 5.38%. However, prescribing drugs by generic name makes the treatment low cost and rational as it avoids prescription writing and reading errors and confusion of dispensing of different brand names which sounds alike and spell similar [15]. The ophthalmologist suggested that the low number of prescribing by generic name drugs was due to non-availability of all ophthalmologic products by generic names.
The study at Jammu and Karnataka had low prescriptions by generic names (1%) while study at New Delhi reported higher percentage (35%) of prescription by generic names than our study. In general, generic drugs are less expensive as compared to the brand names that contain the same active ingredients (Brady, 2003). In our study the percentage of encounters with an injection was 0.67%, which was in 4 prescriptions with injection of corticosteroids given intralesionly. This prescription with injection was the rational and the right choice of medication for the disease i.e. chalazion. Use of injection should be limited because it can cause local toxicity and increase the cost of the treatment for the patient (Brunton et al., 2006). The frequency, dosage, and duration of drug therapy are the 3 important parameters, if they are not clearly mentioned in prescription can result in indiscriminate and injudicious use of drugs [22]. In our study the frequency and dosage were mentioned 100% but duration of treatment was 99.39%. In frequency and dosage, even the tapering dosage of corticosteroids in a very well manner and easily understanding way to the patient were prescribed. This shows that good knowledge about the prescription writing of the prescribers. The same parameters were noted in other study in which the frequency of application was recorded in 93% and duration of treatment was mentioned in 75% of all prescriptions audited [23] which were lower than our study.
In our study antibiotics (44.51%) were the most commonly prescribed drugs followed by lubricants (22.54%), antihistaminics (10.81%), steroids (5.48%), baby shampoo (4.11%), nonsteroidal anti-inflammatory drugs (3.9%), mydriatics (1.17%), anti-allergic (0.91%), anti-viral (0.71%), immunosuppressants (0.61%). The percentage of prescribing antibiotics was rightly indicated except in allergic conjunctivitis. But in our study, most of the cases were allergic rhino conjunctivitis which is caused by staphylococcal bacterial endogenous allergens in nasal cavity or upper respiratory tract and to prevent purulent discharge or secondary infection, antibiotics were prescribed [2]. In almost all cases of anterior blephritis, baby shampoo was prescribed. It is recommended by standard books like Parson’s [2] for the treatment of anterior blephritis. In this case, small white scales accumulate along the lashes and associated frequently with dandruff of the scalp. These crusts will be loosened by bathing of the eyes with 1:4 baby shampoos. This softens the deposits and easily picked or rubbed off with pledget of cotton wool [2]. Empirical treatment in eye conditions is based on the likely etiology, severity of the condition, the available medical treatment (i.e. drugs) and surgical treatment. Ongoing treatment is modified by clinical response as there is large degree of variations in organism type and their resistance pattern [24-27].
In our study antibiotics were most commonly prescribed drugs. The percentage of encounters with antibiotics was 95% in our study. Other hospital-based studies in ophthalmology in India have reported at New Delhi (34%) (Biswas et al., 2001), Jammu (32%) [15], Karnataka (30.18%) and Ahmedabad (59%) [17] encounters with antibiotics which is lower than our study. The high use of antibiotics may reflect the severity of infections and low sanitation in our region. Irrelevant use of antibiotics can lead to the increased adverse effects and increased chance of bacterial resistance to the antimicrobial agents (Rees et al., 2000). Antibiotics constituted 44.52% of the total drugs prescribed. Out of which 35.69% were single antibiotics and 64.31% were prescribed as fixed-dose combination (FDC) with other antibiotics, nonsteroidal anti-inflammatory drugs (NSAID), and glucocorticoids. Fluoroquinolones (42.99%) were the most common group of antibiotics prescribed which were like reports of previous other studies done in ophthalmology at Delhi, Jammu, Karnataka and Ahmedabad. Moxifloxacin was preferred in our study compared to other studies which documented Ciplofloxacin and Ofloxacin, as Moxifloxacin was a new generation Fluoroquinolone with a wider spectrum of activity against Gram negative as well Gram-positive organisms, less side effects and due to reports of emergence of resistance to other ocular antibiotics. It was prescribed for various ocular conditions which included infective conjunctivitis, uveitis, stye, blepharitis, meibominitis, allergic conjunctivitis with purulent discharge, and preseptal cellulitis.
The percentage of antibiotics prescribed from NEDL was 33.50% which was also on the lower side and reflected lack of concept regarding essential drugs. In our study 32.94% were prescribed as fixed dose combinations of total prescribed drugs. This shows an increasing use of FDCs in modern ophthalmic practices. Fixed dose combination of Tobramycin + Fluorometholone eye drops was the most commonly prescribed FDC followed by Moxifloxacin + Dexamethasone, Chloramphenicol + Polymixin B, Amoxicillin + Clavunalic acid tablets. Fixed dose combinations have certain drawbacks like dose cannot be individualized for the drugs used in the combination and drugs with different pharmacokinetic patterns cannot be combined. So, it should be used only when it is necessary. Otherwise inappropriate use of the fixed dose combinations can lead to increased adverse drug reactions and increased financial burden to the patient (Brunton et al., 2006). A rising trend in the prescribing of topical antiallergy (Olopatadine) and ocular lubricants was documented in our study. This could be due to availability of emerging new efficacious drugs in the management of allergic conjunctivitis and dry eye syndrome.
Summary and Conclusion
The present study was undertaken to study and assess the patterns of prescriptions and drug utilization by using WHO/ INRUD indicators in ophthalmology outpatient in relation to pharmacoepidemiology, pharmacovigilance, Pharmacoeconomics. This study of prescription analysis gives a message to the prescribing ophthalmologist to achieve rational, safe and costeffective health care. The following are the findings:
a. The average number of drugs per prescription was 3.28.
b. Percentage of drug prescribed by generic name was only 5.38%.
c. Percentage of encounters with antibiotics was 95%.
d. Percentage of encounter with injections was 0.67%.
e. Percentage of drugs prescribed from National Essential Drug List was only 33.50%.
In the study, we found that the newer generation Fluoroquinolone, “Moxifloxcin” was the most commonly prescribed antibiotic and fixed dose combination of Tobramycin + Fluorometholone eye drop was most commonly prescribed FDC among fixed dose combinations for the treatment of various ophthalmic diseases. The prescribing and drug use pattern observed in the present study was within the accepted pattern of treatment of ocular diseases but the study showed ample of scope for the improvement by encouraging the prescriber to prescribe by generic name and selection of drugs from Essential Drug List, to avoid polypharmacy, to encourage continuous monitoring and analysis in day-to-day practices. Our ophthalmologist suggested that low prescribing generic name drugs were due to nonavailability of all the ophthalmic products by generic names. The hospital administration should always look into the issues of the hospital by continuous monitoring of the prescriptions and making the essential and generic name drugs available in the hospital pharmacy. The prescription can then be re-audited to measure the impact of intervention. This will not only help in rationalizing the prescription practices based on the feedback from these studies but also, we can compare these practices between different institutions, regions, and countries. The study suggests educational initiative, development of therapeutic drug committee with drug policy and National Essential Drug List based hospital formulary ensure the rational use of medicines.
Acknowledgement
Authors are grateful to the college for giving library facility to search the literature related to the topic.
Conflict of interest
Authors did not have any conflict of interest.
References
- Satoskar RS, Rege NN, Bhandarkar SD (2013) Pharmacology and pharmacotherapeutics. Revised (23rd edn), 71: 1034.
- Sihota R, Tondon R (2007) Parson's Diseases of the Eye, (20th edn),
- Able RS, Able AD (1997) Ocular diseases: In Avery's Drug Treatment, (4th edn), Ethiopia.
- Sutharson L, Hariharan RS, Vamsadhara C (2003) Drug utilization study in Diabetology out-patient setting of a tertiary hospital. Indian J Pharmacol 35: 237-240.
- Uppal R, Chhabra A, Narang A (1984) Pattern of drug use in neonatal intensive care unit. Indian Pediatr 35: 647-649.
- Krishnaswamy, K Dinesh KB, Radhaiah G (1985) A drug survey: Precepts and Practices. Eur J Clin Pharmacol 29: 363-370.
- WHO (1993) Action Programme on Essential Drugs? How to investigate drug use in health facilities: selected drug use indicators. Geneva, World Health Organization.
- Hogerzeil HV, Bimo, Ross DD, Laing RO, Ofori AD, et al. (1993) Field tests for rational drug use in twelve developing countries. Lancet 1993; 342(8884): 1408-1410.
- Gupta N, Sharma D, Garg SK, Bhargava VK (997) Audit of prescriptions to study utilization of antimicrobials in a tertiary hospital. Indian J Pharmacol 29: 411-415.
- Karande S, Sankhe P, Kulkarni M (2005) Patterns of Prescription and Drug Dispensing. Indian J Pediatrics 72: 117-121.
- Kulkarni RA, Kochhar PH, Dargude VA, Rajadhyakshya SS (2005) Patterns of antimicrobial use by surgeons in India. Indian J Surg 67: 308-315.
- Maini R, Verma KK, Biswas NR, Agrawal SS (2002) Drug utilization study in dermatology in a tertiary hospital in Delhi. Indian J Physiol Pharmacol 46(1): 107-110.
- Alam K, Mishra P, Prabhu M, Shankar PR, Palaian S, et al. (2006) A study on rational drug prescribing and dispensing in outpatients in a tertiary care teaching hospital of Western Nepal. Kathmandu University Medical Journal 4(16): 436-33.
- Palaian S, Shankar PR, Hegde C, Hegde M, Ojha P et al. (2008) Drug Utilization Pattern in Dental Outpatients in Tertiary Care Teaching Hospital in Western Nepal. NYSDJ 63-67.
- Nehru M, Kohli K, Kapoor B, Sadhotra P, Chopra V, et al. (2005) Drug Utilization Study in Outpatient Ophthalmology Department of Government Medical College Jammu. JK Science 7(3): 149-151.
- Husar DA (1995) Patients compliance in Remington: The Science and Practice of Pharmacy, (19th edn), pp. 1796-1806.
- Prajapati VI, Yadak AK (2012) Drug use in ophthalmology outpatient department A prospective study at a tertiary care teaching hospital. Indian Journal of Pharmacy Practice 5: 2.
- Biswas NR, Jindal S, Siddiquei MM, Maini R (2001) Patterns of prescription and drug use in ophthalmology in a tertiary hospital in Delhi. Br J Clin Pharmacol 51: 267-269.
- Kanakambal S, Murgesh N, Shanthi M (2001) Drug prescribing pattern in a tertiary care teaching hospital in Madurai. Indian J Pharmacol 33: 223.
- Mirza NY, Desai S, Ganguly B (2008) Prescribing pattern in a pediatric out-patient department in Gujarat. Bangladesh J Pharmacol 4: 39-42.
- Gangwar A, Singh R, Singh S, Sharma BD (2011) Pharmacoepidemiology of drugs utilized in ophthalmic outpatient and inpatient department of a tertiary care hospital. Journal of Applied Pharmaceutical Science 1(9): 135-140.
- Brunton LL, Lazo JS, Parker KL (2006) Ocular pharmacology. In Goodman and Gilman’s, The Pharmacological basis of Therapeutics (11th edn), Brunton LL, Lazo JS, Parker KL (Eds.), McGraw-Hill: New York, USA, pp. 1707-1737.
- Sharma SC, Uppal R, Sharma PL (1990) Rational use of topical corticosteroids in dermatology. Ind J Pharmacol 22: 141-144.
- Daniel M [2003] Overview initial antimicrobial therapy for microbial keratitis Br J Ophthalmol 0: 1172-1174.
- Biswas NR, Biswas RS, Pal PS, Jain SK, Malhotra SP, et al. (2000) Patterns of prescriptions and drug use in two tertiary hospitals in Delhi. Indian J Physiol Pharmacol 44(1): 109-112.
- Brady C Ask a pharmacist, why do some medications cost so much? I'm trying to save money by buying generic brands, but are they really a good value? In: Brady C (Ed.), Chatelaine (English edition), Toronto, Canada, 76: 1.
- Rees RE, Betts RF, Gamustop B (2000) Handbook of Antibiotics. (3rd edn), Lippincott William and Wilkins, Philadelphia, USA.






























