Thyroid Disorders Presenting in The Acute Medical Unit
Eka Nandoshvili1* and Steve Hyer2
1Department of Endocrinology, Epsom & St Helier University Hospitals NHS Trust, UK
2Department of Endocrinology, Epsom & St Helier University Hospitals NHS Trust, UK
Submission: March 29, 2019;Published: April 15, 2019
*Corresponding author: Eka Nandoshvili Department of Endocrinology, Epsom & St Helier University Hospitals NHS Trust, UK
How to cite this article: Eka Nandoshvili, Steve Hyer. Thyroid Disorders Presenting in The Acute Medical Unit. J of Pharmacol & Clin Res. 2019; 7(1): 555702. DOI: 10.19080/JPCR.2019.07.555702
Abstract
The recognition of thyroid disorders in the Acute Medical Unit is not always easy as the symptoms and signs may be non-specific and easily mistaken for other illnesses. In the elderly, for example, the insidious nature of thyroid disorders may be mistaken for normal ageing. Thyroid conditions presenting in the Acute Medical Unit range from asymptomatic subclinical thyroid dysfunction to life-threatening severe hyperthyroidism (thyroid storm) or extreme hypothyroidism (myxoedema coma). We describe our experience in an Acute Medical Unit in a busy general hospital and refer to the published literature.
Introduction
Thyroid dysfunction comprises both clinical and subclinical thyroid deficiency (hypothyroidism) and thyroid excess (hyperthyroidism). Subclinical thyroid dysfunction is defined as normal free thyroid hormones (fT4, fT3) but abnormal TSH values. About 15% of patients admitted to hospital will have subclinical thyroid dysfunction [1]. Overall, about 2% of hospital in-patients in the UK will be newly diagnosed with hypothyroidism [2]. By contrast 0.3 - 1% of in-patients will have previously undiagnosed hyperthyroidism, a rate similar to that seen in the community [3]. In our hospital, all patients with medical conditions are admitted via the Acute Medical Unit (AMU). We were interested to examine the pattern of thyroid disorders presenting to our AMU and to assess the impact of the thyroid condition on their hospital stay.
Methods
We investigated all adult admissions via our AMU from January to December 2018 coded as having a primary or secondary diagnosis of thyroid disorder. We used the ICD-9 hospital codes for thyroid disorders (E000 - E079). Sixteen patients (13 females, 3 males) were identified. The clinical records of these patients were then examined to determine the clinical presentation of these patients, the nature of their thyroid disorder, the management of their condition and the impact on their hospital stay.
Results
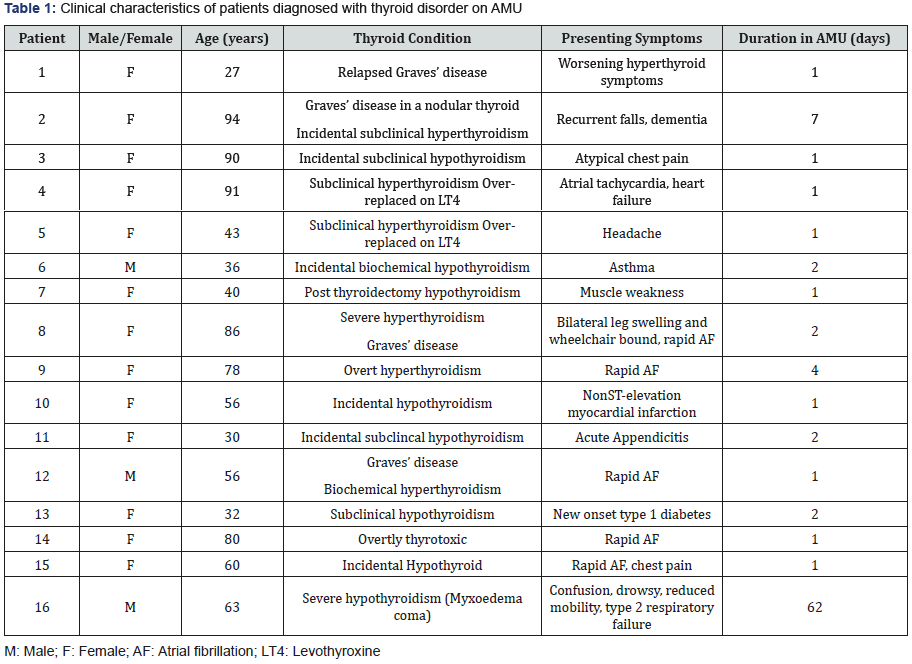
The clinical characteristics of the patients are shown in Table 1. The patients were predominantly female (13/16) and aged 27 - 94 years. Of the eight patients with hypothyroidism, five were subclinical. By contrast, only 3 of the eight hyperthyroid patients were classified as subclinical. In the elderly patients (defined as those over 75), thyroid excess was more common (2 subclinical, 3 overt hyperthyroidism) than thyroid deficiency (1 subclinical hypothyroidism). Atrial fibrillation occurred in both hyperthyroid and hypothyroid patients. The median duration of hospital stay was 1 day [range 1-62].
Discussion
The results of this survey might suggest that thyroid disorders do not commonly account for clinical presentations to this hospital. However, this data is based on hospital coding which relied upon the discharge diagnosis. Only if a thyroid disorder was entered as a diagnosis in the discharge summary would the patient have been identified. Prevalence data based on laboratory results would almost certainly result in a much higher prevalence of abnormal thyroid function. The low number of patients identified might also reflect missed diagnoses. The presentation of hyperthyroidism in the elderly is frequently less obvious than in younger patients as older patients typically present with apathy and weight loss rather than with hyperdynamic symptoms such as tremor, heat intolerance and agitation [4]. Elderly patients with hyperthyroidism may present with agitation and confusion although this presentation was not seen in this small series. Similarly, patients with hypothyroidism may present to their doctors with non-specific symptoms such as fatigue and depression [5].
The majority of identified patients had a short stay on AMU and were discharged on treatment to be followed in outpatient clinics. This might suggest that the thyroid condition had little clinical impact. However, we found 3 patients with rapid atrial fibrillation associated with hyperthyroidism which, at least in one patient, precipitated congestive heart failure. Thyroid storm or severe hyperthyroidism is characterized by a hyper-metabolic state, neuropsychiatric change and often cardiac failure [6]. It carries a high mortality especially in older patients.
We identified one patient in this cohort with severe hypothyroidism requiring transfer to the High Dependency Unit. Often referred to as ‘myxoedema coma’ (although neither oedema nor coma may be present), the condition is more common in elderly females and is associated with a high mortality rate [7]. This patient had a prolonged hospital stay requiring mechanical ventilation and intravenous thyroxine. His recovery was complicated by hospital acquired pneumonia and acute myocardial infarction. Treatment of hypothyroidism with levothyroxine in older patients or those with cardiac disease needs to be done cautiously as it can provoke angina or cardiac rhythm disorders. Subclinical thyroid dysfunction is common in hospitalized patients. Subclinical hyperthyroidism is associated with atrial fibrillation and osteoporosis. Current guidelines recommend treatment when the TSH is fully suppressed (<0.1 mU/l) especially if over 65 years and cardiac risk factors are present [8]. Dose adjustment is needed if the subclinical hyperthyroidism is due to excessive doses of levothyroxine. Subclinical hypothyroidism (SCH) is often asymptomatic. It is important to recognize and treat women with SCH who are planning a pregnancy or who are pregnant as soon as possible as levothyroxine may improve cognitive function in the offspring. Treatment for SCH is recommended for non-pregnant adults if the serum TSH exceeds 10 mU/l even if no symptoms [9]. However, treatment of SCH is not generally recommended in those aged over 80 years. Testing thyroid function when patients are severely ill can prove challenging because of physiological changes that are thought to prevent excessive catabolism (‘euthyroid sick syndrome’) [10]. Patients typically have low circulating free thyroid hormone levels and low TSH concentration which recover as the illness resolves. This phenomenon may contribute to the high prevalence of abnormal thyroid results observed in hospitalized patients. For this reason, routine testing of thyroid function in patients admitted acutely to hospital is not recommended [11].
Conclusion
With the widespread availability of thyroid hormone testing, abnormalities of thyroid function are commonly observed especially when patients are tested in hospital settings. Results need to be interpreted carefully in relation to the clinical situation. Although uncommon, serious thyroid conditions which may potentially be life-threatening may present to the acute physician and a high index of suspicion is needed so that these disorders are detected early. Patients with thyroid disorders may present with non-specific or atypical symptoms especially in the elderly and in these patients, meticulous clinical assessment is needed in order to make the right diagnosis.
References
- Spencer CA, Eigen A, Shen D (1987) Specificity of sensitive assays of thyrotropin (TSH) used to screen for thyroid disease in hospitalized patients. Clin Chem 33: 1391-1396.
- Vanderpump MPJ, Tunbridge WMG (2002) Epidemiology and prevention of clinical and subclinical hypothyroidism. Thyroid 12: 839-847.
- Vanderpump MPJ, Tunbridge WMG, French JM (1995) The incidence of thyroid disorders in the community; a twenty-year follow up of the Whickham survey. Clin Endocrinol 43: 55-68.
- Bhattacharyya A & Wiles PG (1999) Thyrotoxicosis in old age: a different clinical entity? Hosp Med 60: 115-8.
- Tachman ML, Guthrie GP (1984) Hypothyroidism: diversity of presentation. Endocr Rev 5(3): 456-465.
- Wartofsky L Braverman LE, Utiger RD (2005) Thyrotoxic storm. In: Werner's and Ingbar's the thyroid (9th edn), Lippincott Williams and Wilkins, Philadelphia, USA, pp. 652-657.
- Matthew V, Misgar RA, Ghosh S (2011) Myxedema Coma: A New Look into an Old Crisis. J Thyroid Res pp. 493-462.
- National Institute for Health and Care Excellence (NICE) Hyperthyroidism (2019) Clinical Knowledge Summaries.
- National Institute for Health and Care Excellence (NICE) Hypothyroidism (2018) Clinical Knowledge Summaries.
- Neto AM, Zantut-Wittman DE (2016) Abnormalities of Thyroid Hormone Metabolism during Systemic Illness: The Low T3 Syndrome in Different Clinical Settings. International Journal of Endocrinology p. 9.
- UK Guidelines for the Use of Thyroid Function Tests (2006)






























