- Review Article
- Abstract
- Purpose of the Study
- Introduction
- Provision of Pharmacy Services
- Pharmacists-led Medication Reconciliation
- Patient Counseling and Education
- HMR
- Barriers to Pharmaceutical Care
- Practice-Setting Constraints
- Intra-Professional Barriers
- Compensation Benefits
- Medication Risk Management
- Outpatient Service Through Telemedicine
- Challenges of Chronic Health Management
- Epilogue
- References
Pharmacists in Ambulatory/ Outpatient Care
AK Mohiuddin*
Department of Pharmacy, World University of Bangladesh, Bangladesh
Submission: January 19, 2019;Published: April 04, 2019
*Corresponding author: AK Mohiuddin, Faculty of Pharmacy, World University of Bangladesh, Bangladesh
How to cite this article: AK Mohiuddin. Pharmacists in Ambulatory/ Outpatient Care. J of Pharmacol & Clin Res. 2019; 7(1): 555701. DOI: 10.19080/JPCR.2019.07.555701
- Review Article
- Abstract
- Purpose of the Study
- Introduction
- Provision of Pharmacy Services
- Pharmacists-led Medication Reconciliation
- Patient Counseling and Education
- HMR
- Barriers to Pharmaceutical Care
- Practice-Setting Constraints
- Intra-Professional Barriers
- Compensation Benefits
- Medication Risk Management
- Outpatient Service Through Telemedicine
- Challenges of Chronic Health Management
- Epilogue
- References
Article Synopsis
Pharmacy is evolving from a product-oriented to a patient-oriented profession. This role modification is extremely healthy for the patient, the pharmacist, and other members of the health-care team. However, the evolution will present pharmacists with a number of new challenges. Now, more than in the past, pharmacists must make the acquisition of contemporary practice knowledge and skills a high priority, to render the level of service embodied in the concept of pharmaceutical care. Pharmacy educators’ organizations and regulatory bodies must all work together to support pharmacists as they assume expanded health-care roles. Pharmacy and the health-care industry must work to ensure that the pharmacist is compensated justly for all services. But before this can happen it will be necessary for pharmacy to demonstrate value-added to the cost of the prescription. Marketing of the purpose of pharmacy in the health-care morass and of the services provided by the pharmacist is needed to generate an appropriate perceived value among purchasers and users of health-care services. Pharmacists should view themselves as dispensers of therapy and drug effect interpretations as well as of drugs themselves. Service components of pharmacy should be identified clearly to third party payers and be visible to consumers, so that they know what is available at what cost and how it may be accessed. In the future, pharmacy services must be evaluated on patient outcome (i.e., pharmaceutical care) rather than the number of prescriptions dispensed, and pharmacy must evolve toward interpretation and patient consultation, related to the use of medication technologies.
Abstract
Wandering consideration drug store practice is characterized as the arrangement of incorporated, available medicinal services benefits by drug specialists who are responsible for tending to prescription needs, creating continued organizations with patients, and rehearsing with regards to family and network. This is practiced through direct patient consideration and drug the board for mobile patients, long haul connections, coordination of consideration, persistent support, wellbeing and wellbeing advancement, triage and referral, and patient training and self-administration. The walking care drug specialists may work in both an institutional and network-based facility engaged with direct consideration of a different patient populace. An assortment of strength facilities is accessible for sensitivity and immunology, pulmonology, endocrinology, cardiology, nephrology, nervous system science, social wellbeing, and irresistible malady. Such administrations for this populace may exist as an essential consideration facility or an autonomous claim to fame center, ordinarily in a PCMH, which is instrumental in organizing care between different suppliers. When a training site is distinguished, it is vital to build up a solid, trusting, and commonly helpful association with the different chiefs (e.g., overseers, suppliers) required with the center. In the event that drug store administrations are as of now in presence, the drug store chief might have the capacity to recognize and at first contact the fitting individual. In the event that another drug specialist is giving clinical administrations, this individual would be an asset to help decide territories for development of patient consideration and to whom to coordinate the proposed field-tested strategy. Extra people to consider as an underlying purpose of contact incorporate the center administrator, facility medicinal chief, or clerical specialist to both of these people. On the off chance that the facility setting is associated with a restorative school, it might be important to contact the Department of Family Medicine head.
Abbrevations: PCMH: Patient-Centered Medical Home; CAT: Communication Accommodation Theory; MTM: Medication Therapy Management ; TOC: Transitions of Care ; HMR: Home Medicines Reviews ; MMR: Medication Management Review ; PC: Pharmaceutical Care ; NAPRA: National Association of Pharmacy Regulatory Authorities; IPC: Interprofessional Collaboration ; DRPs: Drug-related problems ; JPCC: Joint Commission of Pharmacy Practitioners ; MR: Medication Reconciliation
- Review Article
- Abstract
- Purpose of the Study
- Introduction
- Provision of Pharmacy Services
- Pharmacists-led Medication Reconciliation
- Patient Counseling and Education
- HMR
- Barriers to Pharmaceutical Care
- Practice-Setting Constraints
- Intra-Professional Barriers
- Compensation Benefits
- Medication Risk Management
- Outpatient Service Through Telemedicine
- Challenges of Chronic Health Management
- Epilogue
- References
Purpose of the Study
Discussion and projection of pharmacists’ jobs and duties in walking care settings
Methodology
The examination is led through optional information seek from a few sources from books, specialized pamphlets, papers, di aries, and numerous different sources. The present investigation was begun from the earliest starting point of 2018. PubMed, ALTAVISTA, Embase, Scopus, Web of Science, and the Cochrane Central Register of was completely sought. The watchwords were utilized to look for changed distributers’ diaries like Elsevier, Springer, Willey Online Library, Wolters Kluwer were widely pursued.
Findings
Ambulatory Care Pharmacy tends to the arrangement of coordinated, open social insurance administrations of walking patients changing from the healing center to home or another consideration office. Given the emphasis on walking care as a possibility for wellbeing framework recharging, it is vital to assess the arrangement of home consideration administrations to guarantee that care is enhanced and addresses patient issues.
Limitation of the study
There are an excessive number of data accessible with respect to wandering pharmacists’ jobs and obligations, superiorities in social insurance field among others in human services calling. Data just accessible from presumed diaries are included here.
Practical Implication
Students, specialists and experts of various foundation and controls pharmacists, specialists, medical attendants and wellbeing administrative specialists need to procure much from this article.
- Review Article
- Abstract
- Purpose of the Study
- Introduction
- Provision of Pharmacy Services
- Pharmacists-led Medication Reconciliation
- Patient Counseling and Education
- HMR
- Barriers to Pharmaceutical Care
- Practice-Setting Constraints
- Intra-Professional Barriers
- Compensation Benefits
- Medication Risk Management
- Outpatient Service Through Telemedicine
- Challenges of Chronic Health Management
- Epilogue
- References
Introduction
Walking alludes to patients not possessing beds in healing facilities or other inpatient settings. Mobile patients are noninstitutionalized patients who have the obligation regarding getting their prescription, putting away it, and taking it. They could possibly be outpatients, contingent on where they get their treatment. They may even be in a wheelchair and, entirely, not mobile, but rather in the event that they are not regulated, they will have indistinguishable fundamental duty regarding their medicine from strolling patients. Different assignments are utilized to order patients: systematized, noninstitutionalized, inpatient, outpatient, confined to bed, and wandering. Wandering patients might be inpatients of an organization, for example, a healing center or broadened care office, in the event that they are not limited to bed. Be that as it may, the term wandering patient has turned out to be increasingly prohibitive in its cutting-edge utilization essentially to mean a noninstitutionalized patient. Regardless of whether patients counsel a doctor who may endorse medicine or whether they choose to treat themselves, the network pharmacist more than likely will come into contact with them. It is critical, in this way, for the pharmacist to have a comprehension of these patients so that as a pharmacist and individual from the social insurance group, the most ideal medicinal services for wandering patients might be given through appropriate utilization of information and judgment.
Scope of ambulatory care practice
Human services change has made an interest in change in the conveyance of social insurance administrations. Empowering the presentation of the medicine master in giving patient-focused consideration is an essential component in the progression of conveying quality clinical administrations. The mobile setting is the place most people in the US get medicinal services [1]. Thus, walking care is a developing field of pharmacy practice. Work of enrolled pharmacists is anticipated to rise drastically in doctor workplaces and therapeutic focus outpatient facilities inside next 10 years. The writing likewise underpins the constructive outcomes of pharmacy practice in wandering consideration settings, for example, diminished benzodiazepine use, enhanced uneasiness scores, enhanced heart results, and enhanced consistence [2]. Social insurance installment change will have broad impacts on wellbeing framework conduct, including a move of assets from inpatient care to wandering consideration. Wellbeing frameworks will give reestablished consideration-well past lip benefit-to established general wellbeing activities (i.e., illness counteractive action and wellbeing advancement). They have higher desires for initiative by pharmacists on an expansive exhibit of prescription use issues that influence institutional achievement. Given the attention on mobile consideration as a possibility for wellbeing framework recharging, it is imperative to assess the arrangement of home consideration administrations to guarantee that care is improved and addresses patient issues. An about 85% certifiable reaction got that almost all wellbeing frameworks will have solid monetary impetuses to keep their patients sound and not needing surprising expense medicinal services administrations, especially inpatient care, fortifies the significance of keeping “in danger” populaces sound. A noteworthy ramification of this expectation is that wellbeing framework pharmacy must grasp wandering consideration [3]. Pharmacy Forecast 2016– 2020, distributed by the American Society of Health-System Pharmacists Research and Education Foundation, predicts that medicinal services installment change will result in a critical move of wellbeing framework assets from inpatient to mobile consideration. Medicinal services conveyance and financing will move self-assuredly to extend pharmacist benefits in wandering consideration facilities [4,5]. The gauge is the fourth yearly report the establishment has created for doctor’s facility and wellbeing framework pharmacists. Other featured subjects incorporate:
a) The need to optimize the deployment of pharmacy talent.
b) An emerging oversupply in some regions of pharmacists for entry-level positions.
c) New tools to measure and improve pharmacist and departmental performance.
d) Continuing attention to “meaningful-use” requirements for information technology.
e) Implications of the patient empowerment movement for pharmacies [6].
Optimizing pharmacy workforces over the next five years will involve placing greater emphasis on ambulatory care. Threefourths of the forecast panelists believe that at least a quarter of health systems will require patient-care pharmacists to be responsible for both inpatients and outpatients. Also, at least a quarter of health systems are expected to shift 10% or more of their inpatient pharmacy positions to ambulatory-care positions. This shift towards ambulatory care is expected to result in a vacancy rate of at least 10% for ambulatory-care pharmacy leadership positions [7].
Pharmacists in Ambulatory care
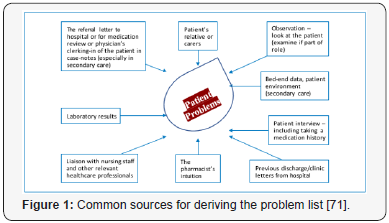
ll individuals who go out on a limb of genuine or potential drug treatment issues. These issues are a noteworthy wellspring of grimness and mortality when left undetected and uncertain and drive colossal expenses over the wellbeing framework. As drug treatment specialists, pharmacists give drug treatment the board administrations worked around an organization between the pharmacist, the patient (or his or her parental Figure 1), doctors and different individuals from a patient’s medicinal services group. As wandering consideration pharmacy practice develops, there has been a continuous exertion to distinguish the ideal job of the staff pharmacists in outpatient care and to give linkages to favored results. In any event 25% of wellbeing frameworks, patient consideration pharmacists will have umbrella obligations, including the two inpatients and outpatients, for seeking after the best results from drug treatment [4]. Their vision is to be a dependably standard setting in its arrangement of direct patient consideration and to ceaselessly create strategies that enhance this training. They encourage protected, viable, effective and affordable utilization of prescriptions with the point of upgrading patient consideration by qualified and prepared staff. Pharmacists assume a basic job in the sheltered, quality and powerful utilization of drugs in enhancing patient’s physical and mental wellbeing [8]. They are instrumental in overseeing medicine related issues to supplement the all-encompassing consideration for patients all through the association. Pharmacists give training to patients and parental figures on the protected and suitable utilization of prescriptions, guide taking drugs consistence, screen and oversee medicine reactions, just as screen for unsafe drug connections [9]. Also, they represent considerable authority in suggesting ideal drug treatment for simultaneous therapeutic issues, with the point of improving treatment results and encouraging the progression of consideration as patients coordinate once more into the network [10-14].
Expertise in Therapy Management
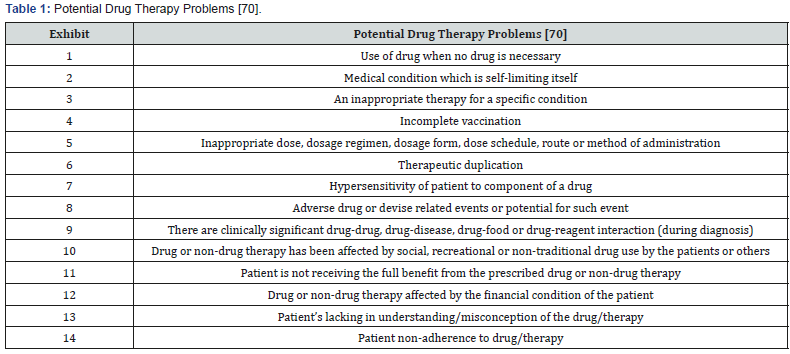
The goal of pharmacy service is to identify and resolve actual or potential drug therapy problems (Table 1) for patients and to promote the safe and effective use of medications and enable patients to achieve positive, targeted therapy outcomes. The medication management framework includes the following:
Assessment: The pharmacist assesses each patient through observation, dialogue and consideration of clinical indicators. Medication counselling opportunities are key times for pharmacists and patients to discuss medications and patients’ concerns about their therapy. Communication Accommodation Theory (CAT) describes behavioral, motivational and emotional processes underlying communication exchanges. Five CAT strategies (approximation, interpretability, discourse management, emotional expression and interpersonal control) permit identification of effective communication. In most European countries, feedback is embedded in education, training and daily professional activities. It is a valuable tool for indicating whether things are going in the right direction or whether redirection is required. Treatment alternatives are assessed for appropriateness, effectiveness and safety (including interactions), to prevent and resolve medication- related problems [15-17].
Care plans: The pharmacist creates a plan in consultation with the patient and, when necessary, other members of the health care team. The care plan includes goals and actions to achieve the patient’s personal health goals through optimal drug therapy. Patient participation means involvement of the patient in decision making or expressing opinions about different treatment methods, which includes sharing information, feelings and signs and accepting health team instructions [18]. Actions include patient and/or caregiver education about chronic disease, writing a prescription to continue care, initiating new treatment and disease prevention such as immunization and lifestyle modification programs. There is a huge opportunity for pharmacists to have a significant impact on reducing healthcare costs, as they have the expertise to detect, resolve, and prevent medication errors and medication-related problems [19]. Care plans also include medication support systems such as compliance packaging and medication reminders.
Monitoring compliance and evaluating effectiveness: Adherence to therapies is a primary determinant of treatment success. Failure to adherence is a serious problem which not only affects the patient but also the health care system. The pharmacist monitors the patient’s compliance with and response to drug therapy through regular follow-ups [20,21]. Tertiary hospitals manage patients with complex care needs. Hospital pharmacists frequently dispense medicines when there is limited global experience with use, but where local prescribers feel their benefit outweighs the risk. These allow for progress evaluation and support and early detection of adverse effects, drug misuse or abuse [22].
Committed Relationship with Patients
Many patients interact with the health system at multiple points. Medication therapy may be started, altered or adjusted at any point along this continuum of care by multiple providers. But pharmacists are the health professionals with the best potential to effectively coordinate medication across the continuum. As important members of the health care team, pharmacists work collaboratively with patients’ other health care providers in all types of patient care settings ranging from community pharmacies to hospitals and long-term care facilities [23]. In particular, community- based pharmacists are accessible and uniquely positioned to support a continuum of primary care, the challenges of living with chronic disease, assisting people to remain in their homes as they age and assisting people living with mental illness or chronic diseases [24]. The first step in the provision of pharmaceutical care is the establishment of a committed relationship with the patient. To that end, pharmacists must seek and be granted authority by their patients to intervene on their behalf. Pharmacists also may need to secure permission from other health-care providers and patient caregivers (e.g., in cases in which the patient is a child or unable to visit the pharmacy in person) to provide pharmaceutical- care services. The key to doing so in all instances is effective communication. Building a committed relationship cannot occur at a distance. The pharmacist-patient relationship has changed over the past 30 years from one in which pharmacists focused solely on filling prescriptions without questioning a physician’s order to one in which pharmacists recommend drug therapy to prescribers and offer personalized advice to patients on how to maximize the benefits of their medication [25]. In addition, by its very nature, pharmaceutical care is an iterative and ongoing process, as long as the patient has unresolved medication-related problems. Therefore, once a rapport has been established, the pharmacist must interact regularly with the patient to strengthen the relationship and to collect additional data necessary to ensure that the patient’s pharmaceutical-care needs continue to be met [26].
- Review Article
- Abstract
- Purpose of the Study
- Introduction
- Provision of Pharmacy Services
- Pharmacists-led Medication Reconciliation
- Patient Counseling and Education
- HMR
- Barriers to Pharmaceutical Care
- Practice-Setting Constraints
- Intra-Professional Barriers
- Compensation Benefits
- Medication Risk Management
- Outpatient Service Through Telemedicine
- Challenges of Chronic Health Management
- Epilogue
- References
Provision of Pharmacy Services
In the initial organizational plan or proposal, it is important to detail the individual who will be providing services, the services to be provided, the entity (e.g., patient, caregiver, health care team) to whom services will be provided, the time required for the services, the expected outcomes, and a proposed workflow. Ultimately, the goal would be to implement the Pharmacists’ Patient Care Process as defined by the Joint Commission of Pharmacy Practitioners (JCPP). In such a process, the pharmacist is integrated into the delivery of care for the patient in an interprofessional setting [27]. Services to consider implementing include medication reconciliation, MTM, preventative services, and patient-specific medication education and behavioral counseling. However, outpatient pharmacy basic services and functions may include:
Medication Dispensing
The principal idea of medicine is to give the correct prescription to the correct patient after appropriate ID. Drugs ought to be administered at the correct portion, course of organization, frame and length of treatment. For patients, the remedy holder name might be the main wellspring of directions on the best way to take their drugs. In the United States, the lawful necessities for a remedy name are set by government law and state resolutions. The holder ought to be practically identical to that which makers use to bundle drug items and should save an item’s character, quality, quality, and immaculateness and forestall defilement. Wellbeing highlights, for example, a youngster safe conclusion ought to be given. Pharmaceutical items bought from universal online drug stores are not endorsed by the FDA and may not meet US rules for marking and bundling. Pharmacy staff works in close coordinated effort with the diverse restorative offices, nursing administrations and dietary office to address client issues. This is especially helpful with complex patients who have various prescribers and more than one condition requiring treatment. Prescription apportioning databases are progressively accessible for pharmacists on huge populaces, especially in nations that give general inclusion to medications [28-30].
Delivery of Transition Care Medications
Usually home care prescriptions are dispensed and refilled from the ambulatory pharmacy as a service to this patient population. Medicare beneficiaries are covered by the US Social Security Amendment, passed in 1965 and then amended in 1972, which extended health care services to all persons 65 years of age or older. Medicare Part A covers inpatient hospital care, hospice care, and home health care, with deductibles and limits placed on each type of care. Beneficiaries are also eligible for Medicare Part B coverage, which, for a relatively small health insurance premium, allows senior citizens to obtain extended coverage for physician services, outpatient hospital services, home health care services, and a limited number of outpatient drugs (e.g., hepatitis B vaccine, immunosuppressant drugs, pneumococcal and influenza vaccines, and some oral cancer drugs). Optimizing the TOC process, reducing medication errors, and preventing ADEs are important focus areas in the current health care system, as emphasized by The Joint Commission and other health care organizations. Providing a complete and accurate medication reconciliation (MR) at the time of transition is important and improves TOC, especially since most AEs that occur during TOC are adverse drug events. Another study determined that nearly 50% of patients experienced at least one outpatient medical error caused by failure to implement the intended discharge plans for recently hospitalized patients. Ambulatory pharmacists have the unique opportunity and skillset to develop and participate in TOC processes that will enhance medication safety and improve patient care [31-34].
- Review Article
- Abstract
- Purpose of the Study
- Introduction
- Provision of Pharmacy Services
- Pharmacists-led Medication Reconciliation
- Patient Counseling and Education
- HMR
- Barriers to Pharmaceutical Care
- Practice-Setting Constraints
- Intra-Professional Barriers
- Compensation Benefits
- Medication Risk Management
- Outpatient Service Through Telemedicine
- Challenges of Chronic Health Management
- Epilogue
- References
Pharmacists-led Medication Reconciliation
Medication discrepancies arising at care transitions have been reported as prevalent and are linked with adverse drug events (ADEs) (e.g. re-hospitalization) [35]. More than 25% of errors can be attributed to incorrect medication histories, demonstrating that this is an error-prone process. Gleason and colleagues found that more than 33% of patients had at least one medication discrepancy at admission, and 85% of these originated from the medication history. Obtaining an accurate medication history during transitions of care has been shown to reduce errors that could lead to patient harm and is the foundation of the medication reconciliation process. Reconciliation involves building a complete list of a person’s medications, checking them for accuracy, reconciling and documenting any changes. Pharmacy personnel can play a key role in medication safety and prevention of discrepancies upon hospital admission. Buckley and colleagues discovered that greater than 97% of medication histories documented by health care providers other than pharmacists were associated with at least one medication discrepancy [35-40].
- Review Article
- Abstract
- Purpose of the Study
- Introduction
- Provision of Pharmacy Services
- Pharmacists-led Medication Reconciliation
- Patient Counseling and Education
- HMR
- Barriers to Pharmaceutical Care
- Practice-Setting Constraints
- Intra-Professional Barriers
- Compensation Benefits
- Medication Risk Management
- Outpatient Service Through Telemedicine
- Challenges of Chronic Health Management
- Epilogue
- References
Patient Counseling and Education
In the counseling process, a multi-cultural competence of dispenser is among the key factors affecting his/her successful communication with patients for achieving optimal use of medications. Patient counseling by dispenser is a key competency element in the medication treatment process. To this end, it is critical for the dispensers to provide desirable and understandable information to patients about their dispensed medications. The dispenser is in a critical position to answer whatever concerns and enquiries of patients toward their medications and even alternate therapeutic approaches they may seek or hear from others. Accordingly, the Australian Pharmaceutical Advisory Council outlines the type of information and resources that should be delivered to patients. Moreover, list of medicines provided on exit from the healthcare facility should be prepared in communication and collaboration with the patient for ease of improving adherence to treatment regimens and patient outcomes. However, for a non-teaching facility, the addition of clinical pharmacy services may alter workflow pace because the practitioner may be accustomed to moving from one patient to the next without stopping to discuss the treatment plan with the health care team. It may be more challenging to provide recommendations and interventions for each individual patient, and as such, an alternative workflow may be necessary. This may include a pharmacist-specific patient and family education visit, which may reduce the time the practitioner needs to spend with each patient, thus allowing a potential increase in provider patient volume. Crowd and noisy hospital environment, over-loaded physicians, and innumerable patients limited hospital staffs to supply more professional services. Counseling people were increased 4 folds in 2015 compared to in 2013. On the one hand, with the development of the pharmaceutical counseling center, more and more people realized the importance of drug safety and accuracy. [41-46].
- Review Article
- Abstract
- Purpose of the Study
- Introduction
- Provision of Pharmacy Services
- Pharmacists-led Medication Reconciliation
- Patient Counseling and Education
- HMR
- Barriers to Pharmaceutical Care
- Practice-Setting Constraints
- Intra-Professional Barriers
- Compensation Benefits
- Medication Risk Management
- Outpatient Service Through Telemedicine
- Challenges of Chronic Health Management
- Epilogue
- References
HMR
MMRs are an excellent example of optimal pharmaceutical care delivery. MMRs were originally conducted by pharmacists and have been a prime component of the expanded clinical services provided by pharmacists worldwide. Home medication reviews are a subtype of MMRs in which patients are interviewed by a health professional in their own home. This was originally designed for pharmacists to recover relevant information from the patient’s home that is of value and could otherwise be overlooked by health care professionals. It is intended for the pharmacist to observe the patient’s management of their medications and to educate the patient so that the quality use of medicines can be achieved. The HMR has the potential to be a useful tool in patients’ management of their medications. There are clear benefits when per-formed well. HMR is an Australian initiative introduced in 2001 to improve quality use of medicines. The pharmacist reviews the patient’s drug therapies for drug interactions, adverse effects and inconsistencies with the current published views on therapies. GPs plays a vital role in determining whether patients are likely to benefit from this service as HMRs require a referral from a GP. Studies show that GPs believe HMRs potentially improve medication safety, awareness and management. Home medicines review can:
a. Clarify and assure patients about proper use of their medications.
b. Increase the patients understanding of their physicians’ clinical intentions.
c. Promote co-operation between the patient and his clinician.
d. Promote better patient compliance with medication regimens and dosages.
e. Maximize health outcomes from treatment provided [47-51].
- Review Article
- Abstract
- Purpose of the Study
- Introduction
- Provision of Pharmacy Services
- Pharmacists-led Medication Reconciliation
- Patient Counseling and Education
- HMR
- Barriers to Pharmaceutical Care
- Practice-Setting Constraints
- Intra-Professional Barriers
- Compensation Benefits
- Medication Risk Management
- Outpatient Service Through Telemedicine
- Challenges of Chronic Health Management
- Epilogue
- References
Barriers to Pharmaceutical Care
A variety of factors have impeded pharmacists’ ability to implement pharmaceutical care and can be grouped into four general categories.
Individual pharmacist characteristics
Studies have been conducted to establish the challenges to Pharmaceutical care implementation in community and hospital pharmacies in developed countries. The pharmacists’ attitudes such as the lack of understanding of the concept, misconception such as patients’ unwillingness to pay, fear of changing roles and lack of personal motivation reported. Pharmacists who commit to managing the pharmacotherapy of their patients must be familiar with current advances in the treatment of common diseases and with literature resources/ databases that are available to assist them to make sound therapeutic decisions. The attitudes are characterized by conflicts and egos resulting from differences in status/authority, responsibilities, and training. Finally, oral and written communication skills are central to the provision of pharmaceutical care. Pharmacists need to be trained in applying general affective communicative strategies, listening and reflecting, and responding to uttered cues. Combined with non-specific verbal behavior techniques, such as social talk, these techniques are especially important in addressing patient concerns. Pharmacists should refine their communication styles and patterns constantly to ensure patients receive the information they require for effective treatment. They not only create a safe and inviting atmosphere between the pharmacist and patient but also encourage patients to disclose their emotions and concerns. Furthermore, changing the consultation dynamic may also help; from a professional “coolness” approach at the beginning of the consultation to becoming warmer and avoiding non-verbal cut-offs at the end. Incorporating more open-ended questions and follow-up questions throughout the home visit could increase the flexibility of the protocol and might invite patients to express their concerns. [46], [52-56].
- Review Article
- Abstract
- Purpose of the Study
- Introduction
- Provision of Pharmacy Services
- Pharmacists-led Medication Reconciliation
- Patient Counseling and Education
- HMR
- Barriers to Pharmaceutical Care
- Practice-Setting Constraints
- Intra-Professional Barriers
- Compensation Benefits
- Medication Risk Management
- Outpatient Service Through Telemedicine
- Challenges of Chronic Health Management
- Epilogue
- References
Practice-Setting Constraints
There are numerous constraints involved, consisting of supply- side (e.g. workforce shortages), demand-side (e.g. obstacles of access to healthcare) and healthcare system constraints (e.g. regulatory constraints). Resource constraints and other factors associated with a particular practice setting also are mentioned frequently as barriers to the provision of pharmaceutical care. For example, pharmacists often complain that they do not have time to provide pharmaceutical care in addition to their normal responsibilities. A lack of financial resources also is mentioned often as a barrier to the provision of pharmaceutical care. Under constrained financial conditions, healthcare services need to demonstrate that they remain cost-effective, given the investment in their provision. Purchasing additional equipment, hiring and training additional personnel, and redesigning the pharmacy can be quite expensive. A further complication exists when the management of the pharmacy organization is not committed to the provision of pharmaceutical care. In that situation, support for even minor modifications of the practice environment may be completely absent. Most pharmacists should be able to offer pharmaceutical care to a limited number of patients without incurring large expenses. Then, as the number of patients receiving care is expanded, pharmacists can gradually modify the environment to be more conducive to patient-oriented services [19], [57-60].
- Review Article
- Abstract
- Purpose of the Study
- Introduction
- Provision of Pharmacy Services
- Pharmacists-led Medication Reconciliation
- Patient Counseling and Education
- HMR
- Barriers to Pharmaceutical Care
- Practice-Setting Constraints
- Intra-Professional Barriers
- Compensation Benefits
- Medication Risk Management
- Outpatient Service Through Telemedicine
- Challenges of Chronic Health Management
- Epilogue
- References
Intra-Professional Barriers
A fragmented system can be defined as one lacking the integration required to achieve unity of effort. Each part of the system tends to focus on internal tasks and resources, overlooking the system as a whole. Fostering IPC has become one of the core demands of policymakers, funding parties, and health care professionals in practice worldwide. Patients benefit when pharmacists work together. Good team functioning is associated with improved patient outcomes, heightened staff satisfaction, and reduced burnout. In contrast, poor team functioning is associated with poor patient care through adverse events, lack of coordination, and spiraling costs. The NAPRA highlights the importance of collaboration in pharmacist practice. This standard applies not only to pharmacist collaboration with other health care professionals but also to pharmacist collaboration with other pharmacists. Thus, pharmacists from all practice settings and the organizations that represent them must work cooperatively to develop a common agenda for the implementation of pharmaceutical care if this new mission is ever to be fully realized by the profession [60-64].
- Review Article
- Abstract
- Purpose of the Study
- Introduction
- Provision of Pharmacy Services
- Pharmacists-led Medication Reconciliation
- Patient Counseling and Education
- HMR
- Barriers to Pharmaceutical Care
- Practice-Setting Constraints
- Intra-Professional Barriers
- Compensation Benefits
- Medication Risk Management
- Outpatient Service Through Telemedicine
- Challenges of Chronic Health Management
- Epilogue
- References
Compensation Benefits
Expansion of scope of practice and diminishing revenues from dispensing are requiring pharmacists to increasingly adopt clinical care services into their practices. Pharmacists must be able to receive payment in order for provision of clinical care to be sustainable. However, the body of evidence supports the feeling that pharmaceutical care services add value to patient care by enhancing patient compliance, improving patient outcomes, and reducing healthcare costs. A Canadian strategy for improving the provision of patient-centered care by pharmacists, identifies obtaining remuneration for professional services as a key area of action to support such activities. The cost of the prescription then is based upon the cost to the pharmacy plus a handling charge. As the pharmacy practice literature reporting the clinical benefits of pharmacist cognitive services continues to grow and pharmacy revenues from dispensing alone decrease in light of generic drug price reductions and other factors, the profession is advocating for appropriate payment for clinical services. Pharmacists also, with some success, has billed insurance companies for pharmaceutical care services that were provided to his patients. Indeed, lack of remuneration for services has been cited by community pharmacists as a key barrier preventing the greater provision of clinical services [59], [65-67].
- Review Article
- Abstract
- Purpose of the Study
- Introduction
- Provision of Pharmacy Services
- Pharmacists-led Medication Reconciliation
- Patient Counseling and Education
- HMR
- Barriers to Pharmaceutical Care
- Practice-Setting Constraints
- Intra-Professional Barriers
- Compensation Benefits
- Medication Risk Management
- Outpatient Service Through Telemedicine
- Challenges of Chronic Health Management
- Epilogue
- References
Medication Risk Management
Different medication review procedures are internationally used in both outpatient and inpatient settings. The accurate medication history recording and the medication chart is the basis for safe pharmacotherapy and a starting point for medication reviews. strategies to prevent ADRs and drug-related hospital admissions are urgently needed, particularly for elderly patients. In addition to other medication safety initiatives, national and international organizations recommend including pharmacists on health care teams to improve medication safety [68-71]. For each DRP, a specific recommendation should be addressed to the health care team. Each recommendation should be discussed with the healthcare team, and the physician decided if he followed the recommendations. The medication should be checked again and registered, if the recommendation is partly or fully followed.
High prevalence of polypharmacy in older adults has been widely reported1. Multiple studies have mentioned that polypharmacy increases the risk of adverse drug reactions, hospitalization, falls, mortality, and other adverse health outcomes in elderly patients. Pharmacogenomics allow identify how hereditary profile affects an individual response to drugs. As a strategy for optimizing medication usage, pharmacogenomics became an important element of precision medicine. A recent study has demonstrated that precision medicine has significant potential in people with polypharmacy particularly in older adults with history of urgent care utilization [72].
Poor medication management during or immediately after hospital admission increased the risk of readmission in the next month by 28%. Hospital admissions and discharges, interdepartmental transfers, or care shared between a specialist and a GP, are often dangerous times for patients, especially those with longterm conditions or taking multiple medicines. Patients may take a number of medicines in complex regimens so there is a high potential for drug interactions, particularly given the substantial comorbidity and mortality rates in this population. There are significant discrepancies between the medicines people take at home, the medicines GPs think they are taking at home, medicines listed in GP referral letters, medicines people obtain from pharmacies, the medicines recorded when they are admitted to hospital, and when they leave hospital, and the medicines detailed in their official discharge summary.
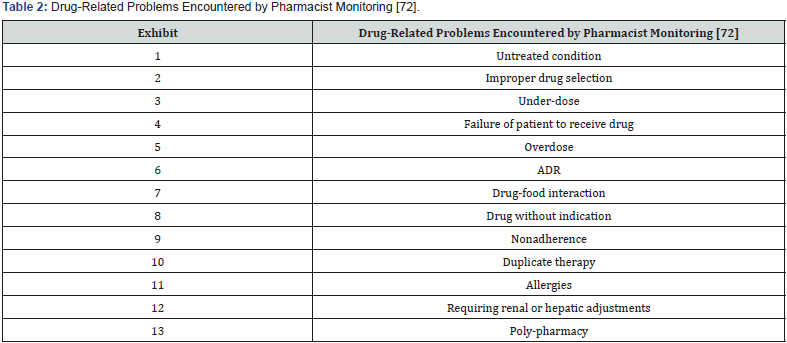
Pharmaceutical care focuses on activities that lead to positive patient outcomes and accepting end results of medication therapy remains important in providing such services. A pharmacist must be a scientific problem solver, a good communicator, educator and learner. Primary activities involved in pharmaceutical care include: obtaining a medication history, identifying real and potential DRPs, developing a pharmacy care plan to include implementing and monitoring parameters to resolve and prevent drug-related problems (Table 2), and evaluating the plan to determine if clinical outcomes have been achieved through documentation, patient consultation follow-up to determine if the desired clinical outcomes have been achieved. Future trends in drug development will increase the pharmacist’s role in drug selection, in an effort to ensure both safety and cost containment. All this is achievable through competent skills and knowledge gained to provide reliable coordinated services. There was a trend for the number of pharmacist-hours containing at least one potentially serious dispensing error to increase as the prescription-filling rate accelerated. Outpatient pharmacies with high volumes should set a limit to the number of prescriptions filled by their pharmacists and should experiment with quality assurance systems to reduce dispensing errors and subsequent legal liabilities [72-74].
- Review Article
- Abstract
- Purpose of the Study
- Introduction
- Provision of Pharmacy Services
- Pharmacists-led Medication Reconciliation
- Patient Counseling and Education
- HMR
- Barriers to Pharmaceutical Care
- Practice-Setting Constraints
- Intra-Professional Barriers
- Compensation Benefits
- Medication Risk Management
- Outpatient Service Through Telemedicine
- Challenges of Chronic Health Management
- Epilogue
- References
Outpatient Service Through Telemedicine
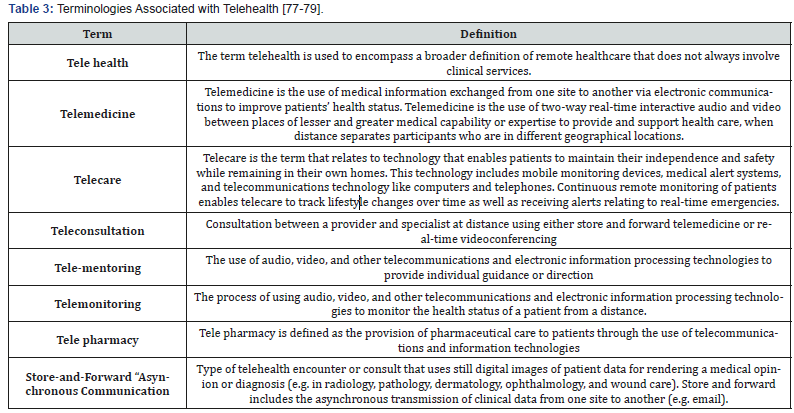
Telemedicine refers to the delivery of clinical services using technology that allows two-way, real time, interactive communication (including telemonitoring and video including follow-up telephone calls) between the patient and the pharmacist at a distant site. In the Unites States, the increasing shortage of primary care providers and specialists represents an opportunity for pharmacists to assume a more prominent role managing patients with chronic disease in the ambulatory care setting. However, lack of reimbursement may pose a barrier to the provision of care by pharmacists using telemedicine [75]. Generally, telemedicine modalities fall into one of two categories: synchronous or asynchronous. In synchronous telemedicine, a confidential, interactive, two-way audio and video connection replaces the in-person, faceto- face visit, using specialized equipment to perform an accurate and reliable history and physical exam. Synchronous telemedicine models are typically used to manage acute and chronic diseases that rely significantly on a real-time patient interaction or the physical exam, such as the management of chronic infectious diseases, pulmonary medicine, diabetes management and telepsychiatry [76-79] (Table 3).
In US 20% of the total people are rural based, only 9% of their physicians have posting there. It is estimated that as of 2016 at least 20% of the US population did not have equal access to health care. In addition to rural areas, telemedicine services have also expanded into prisons, military bases, and school systems. Among 110 million medical visits were conducted in 2015, 59 million were conducted on-line, over the internet, or by using mobile devices, accounting more than 50% of patient visits. Since pharmacists are not recognized by CMS as healthcare providers, they cannot be reimbursed for services rendered under most traditional fee-for-service arrangements. In conclusion, pharmacists have a unique opportunity to use telemedicine models as a means to improve access to care and chronic disease management in both rural and urban populations within the ambulatory setting. Electronic health (eHealth) tools incorporate many opportunities for patients to increase their engagement through focused disease- specific learning, options to receive regular feedback and frequent reinforcement (e.g., peripheral monitoring devices). Additional inbuilt support functions that assess progress, provide goal setting and problem solving, aim to increase the patient’s skill and confidence in managing their health problems. Supplementary motivational interviewing and cognitive behavioral components can also be provided via the internet, mobile device or telephone [80,81]. Micro-hospitals are 24-hour, small inpatient facilities with an average of 2 to 10 beds, designed to provide a diversity of healthcare services consistent with community demands. In addition, they seek to combine a cost-effective healthcare vehicle with potential time-dependent triage/transfer capabilities to a nearby large medical center. This smaller cost-effective entity represents an ideal vehicle for telemedicine, whereby specialists are always on hand for interpretation and consultation, with minimal patient waiting [82].
- Review Article
- Abstract
- Purpose of the Study
- Introduction
- Provision of Pharmacy Services
- Pharmacists-led Medication Reconciliation
- Patient Counseling and Education
- HMR
- Barriers to Pharmaceutical Care
- Practice-Setting Constraints
- Intra-Professional Barriers
- Compensation Benefits
- Medication Risk Management
- Outpatient Service Through Telemedicine
- Challenges of Chronic Health Management
- Epilogue
- References
Challenges of Chronic Health Management
There are significant differences between acute and chronic disease that require different approaches to care. The American health care system is built on an acute care paradigm; in general, acute care problems have a rapid onset, are short in duration, and result from a single cause. Chronic care problems are slower to develop, longer in duration, and have multiple causes, some of which occur years before the onset of symptoms. These differences limit the current system’s ability to deal effectively with a number of unique challenges in managing chronic disease:
a. The social, behavioral, and psychosocial elements associated with chronic disease (e.g., the often-unrecognized elements of self-image related to be a person with disease).,/
b. The need for continuing care, often throughout the remainder of the patient’s life.,/
c. The influence of chronic disease on the patient’s extended family and the very real need for the family’s ongoing support for long-term success.,/
d. The influence of lifestyle factors in both the causation and long-term management of chronic disease,/
Caring for the population of patients with chronic conditions requires a new paradigm-one that encompasses longitudinal care and unplanned episodes of care. To a large extent, the development and implementation of such a system will hinge on addressing 4 specific challenges17:,/
a. Realigned Reimbursement-In general, payment for health care services is triggered by acute care episodes. There must be a mechanism whereby providers are compensated to manage a broad range of chronic conditions that never resolve and that are not characterized by episodes of care.,/
b. Team-Based Care-An adequate number of nonphysician health care team members in disciplines such as nursing, social work, community health coaching, and pharmacy must be trained and available to coordinate proven team-based care.,/
c. Patient and Family Engagement-Expanded opportunities for patient and family engagement in self-management programs are essential for improving patients’ ability to manage their conditions and adhere to treatment plans.,/
d. Information Sharing-The current acute episode-focused medical record system must be redesigned to improve clinicians’ ability to share information regarding patients with chronic disease and facilitate the use of evidence-based decision support in their care [83].,/
- Review Article
- Abstract
- Purpose of the Study
- Introduction
- Provision of Pharmacy Services
- Pharmacists-led Medication Reconciliation
- Patient Counseling and Education
- HMR
- Barriers to Pharmaceutical Care
- Practice-Setting Constraints
- Intra-Professional Barriers
- Compensation Benefits
- Medication Risk Management
- Outpatient Service Through Telemedicine
- Challenges of Chronic Health Management
- Epilogue
- References
Epilogue
In most countries, existing health care systems do not optimize the practices of all health professionals and cost an increasing amount without comparable increases in quality and accessibility. Numerous proposals have been made on how to address these shortcomings. Achieving these goals require different health professionals to work in collaboration with each other to meet the health needs of patients. In order for that to happen, governments must work with all key professional groups to use all available resources of the system most effectively and, importantly, pharmacists must be recognized as the professional that coordinates drug therapy management. In addition, governments must put in place policies and a regulatory and funding environment that facilitates team-based care and acknowledges and supports the professional competencies of all health professions.
- Review Article
- Abstract
- Purpose of the Study
- Introduction
- Provision of Pharmacy Services
- Pharmacists-led Medication Reconciliation
- Patient Counseling and Education
- HMR
- Barriers to Pharmaceutical Care
- Practice-Setting Constraints
- Intra-Professional Barriers
- Compensation Benefits
- Medication Risk Management
- Outpatient Service Through Telemedicine
- Challenges of Chronic Health Management
- Epilogue
- References
References
- Rondinelli JL, Omery AK, Crawford CL, Johnson JA (2014) Self-reported activities and outcomes of ambulatory care staff registered nurses: an exploration. Perm J 18(1): e108-15.
- Walus AN, Woloschuk DMM (2017) Impact of Pharmacists in a Community-Based Home Care Service: A Pilot Program. Can J Hosp Pharm 70(6): 435-442.
- ASHP Foundation Trends Report. Pharmacy Forecast (2016) Strategic Planning Advice for Pharmacy Departments in Hospitals and Health Systems.
- Beans BE (2016) Experts Foresee a Major Shift from Inpatient to Ambulatory Care. PT 41(4): 231-237.
- Knoer SJ (2015) Healthcare delivery and financing: staying ahead of intense competition. In: Zellmer WA (Eds.), Pharmacy Forecast. Strategic Planning Advice for Pharmacy Departments in Hospitals and Health Systems. Bethesda, Maryland: ASHP Research and Education foundation p. 5-8
- Zellmer WA (2016) Pharmacy Forecast. Strategic Planning Advice for Pharmacy Departments in Hospitals and Health Systems. Bethesda, ASHP Research and Education Foundation, Maryland, USA.
- Williams C (2015) Pharmacy work force: market forces stimulate change in pharmacy practice models. In: Zellmer WA (Eds.), Pharmacy Forecast Strategic Planning Advice for Pharmacy Departments in Hospitals and Health Systems. Bethesda, Maryland: ASHP Research and Education Foundation p. 25-28.
- Greiner AC, Knebel E (2003) Institute of Medicine (US) Committee on the Health Professions Education Summit editors. Health Professions Education: A Bridge to Quality. National Academies Press (US); Chapter 3, The Core Competencies Needed for Health Care Professionals, Washington (DC), USA.
- Kehrer JP, Eberhart G, Wing M, Horon K (2013) Pharmacy's role in a modern health continuum Can Pharm J (Ott) 146(6): 321-324.
- Manolakis PG, Skelton JB (2010) Pharmacists' contributions to primary care in the United States collaborating to address unmet patient care needs: the emerging role for pharmacists to address the shortage of primary care providers. Am J Pharm Educ 74(10): S7.
- Kiel WJ, Phillips SW (2017) 0Impact of Pharmacist-Conducted Comprehensive Medication Reviews for Older Adult Patients to Reduce Medication Related Problems. Pharmacy (Basel) 6(1): 2.
- Reid PP, Compton WD, Grossman JH (2005) National Academy of Engineering (US) and Institute of Medicine (US) Committee on Engineering and the Health Care System. Building a Better Delivery System: A New Engineering/Health Care Partnership. National Academies Press (US) 2, A Framework for a Systems Approach to Health Care Delivery, Washington (DC), USA.
- Hata M, Klotz R, Sylvies R (2012) Medication therapy management services provided by student pharmacists. Am J Pharm Educ 76(3): 51.
- Murphy Menezes M (2015) Role of the Pharmacist in Medication Therapy Management Services in Patients with Osteoporosis. Clin Ther 37(7): 1573-1586.
- Hardavella G, Aamli-Gaagnat A, Saad N, Rousalova I, Sreter KB (2017) How to give and receive How to give and receive feedback effectively. Breathe (Sheff) 13(4): 327-333.
- Chevalier BAM, Watson BM, Barras MA, Cottrell WN (2017) Investigating strategies used by hospital pharmacists to effectively communicate with patients during medication counselling. Health Expect 20(5): 1121-1132.
- Blenkinsopp A, Bond C, Raynor DK (2012) Medication reviews. Br J Clin Pharmacol 74(4): 573-80.
- Vahdat S, Hamzehgardeshi L, Hessam S, Hamzehgardeshi Z (2014) Patient involvement in health care decision making: a review. Iran Red Crescent Med J 16(1): e12454.
- Dalton K, Byrne S (2017) Role of the pharmacist in reducing healthcare costs: current insights. Integr Pharm Res Pract 6: 37-46.
- Jimmy B, Jose J (2011) Patient medication adherence: measures in daily practice. Oman Med J 26(3): 155-159.
- Omboni S, Caserini M (2018) Effectiveness of pharmacist's intervention in the management of cardiovascular diseases. Open Heart. ;5(1): e000687.
- Keith C (2018) Automated adverse drug reaction detection. Aust Prescr 41(5): 138.
- American Pharmacists Association (APhA) Pharmacists’ Impact on Patient Safety. A Joint Project of the American Pharmacists Association Academy of Pharmacy Practice and Management and Academy of Pharmaceutical Research and Science.
- Gallagher HC (2010) New fitness-to-practice requirements for pharmacists in Ireland: implications for undergraduate pharmacy education. Med Teach 32(2): e71-e77.
- Haddad AM (2018) Reflections on the Pharmacist-Patient Covenant. Am J Pharm Educ 82(7): 6806.
- Wolters M, van Hulten R, Blom L, Bouvy ML (2017) Exploring the concept of patient centred communication for the pharmacy practice. Int J Clin Pharm 39(6): 1145-1156.
- Joint Commission of Pharmacy Practitioners. Pharmacists' patient care process.
- Bhimji SS, Scherbak Y (2018) Medication Errors. In: Stat Pearls [Internet]. Stat Pearls Publishing, Treasure Island (FL), USA.
- Veronin M (2011) Packaging and labeling of pharmaceutical products obtained from the internet. J Med Internet Res 13(1): e22.
- Pratt N, Roughead E (2018) Assessment of Medication Safety Using Only Dispensing Data. Curr Epidemiol Rep 5(4): 357-369.
- Scott DM (2016) United States Health Care System: A Pharmacy Perspective. Can J Hosp Pharm 69(4): 306-315.
- Hume AL, Kirwin J, Bieber HL, Couchenour RL, Hall Dl, et al. (2012) American College of Clinical Pharmacy. Improving care transitions: current practice and future opportunities for pharmacists. Pharmacotherapy 32(11): e326-e337.
- Sen S, Bowen JF, Ganetsky VS, (2014) Pharmacists implementing transitions of care in inpatient, ambulatory and community practice settings. Pharm Pract (Granada) 12(2): 439.
- Moore C, Wisnivesky J, Williams S, McGinn T (2003) Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med 18(8): 646-651.
- Redmond P, Grimes TC, McDonnell R, Boland F, Hughes C, et al (2018) Impact of medication reconciliation for improving transitions of care. Cochrane Database Syst Rev 8: CD010791.
- Digiantonio N, Lund J, Bastow S (2018) Impact of a Pharmacy-Led Medication Reconciliation Program. PT 43(2): 105-110.
- Abdulghani KH, Aseeri MA, Mahmoud A, Abulezz R (2017) The impact of pharmacist-led medication reconciliation during admission at tertiary care hospital. Int J Clin Pharm 40(1): 196-201.
- Mekonnen AB, McLachlan AJ, Brien JE, Mekonnen D, Abay Z (2018) Evaluation of the impact of pharmacist-led medication reconciliation intervention: a single centre pre-post study from Ethiopia. Int J Clin Pharm 40(5): 1209-1216.
- Cheema E, Alhomoud FK, Kinsara ASA (2018) The impact of pharmacists-led medicines reconciliation on healthcare outcomes in secondary care: A systematic review and meta-analysis of randomized controlled trials. Plosone13(3): e0193510.
- Bonetti AF, Reis WC, Lombardi NF, Mendes AM, Netto HP, et al. (2018) Pharmacist-led discharge medication counselling: A scoping review. J Eval Clin Pract 24(3): 570-579.
- Lampkin SJ, Gildon B, Benavides S, Walls K, Briars L (2018) Considerations for Providing Ambulatory Pharmacy Services for Pediatric Patients. J Pediatr Pharmacol Ther 23(1): 4-17.
- Hirko N, Edessa D, Sisay M (2018) Exit-Knowledge of Ambulatory Patients About Medications Dispensed in Government Hospital in Eastern Ethiopia: The Need for Focused Patient Counseling. Front Public Health 6: 254.
- Australian Pharmaceutical Advisory Council (APAC) (2005) Guiding Principles to Achieve Continuity in Medication Management. Camberra, ACT: Commonwealth of Australia p. 1-52.
- Utilization Review Accreditation Commission (URAC) (2011) Supporting Patient Medication Adherence: Ensuring Coordination, Quality and Outcomes. Columbia, USA, p. 1-22.
- Gu H, Sun L, Jin R, Li F, Wei Y, et al. (2016) Evaluation of counseling environmental alteration on pharmacy-patient communication qualifications: A case-control study. Medicine (Baltimore) 95(52): e5738.
- Ensing HT, Vervloet M, van Dooren AA, Bouvy ML, Koster ES (2018) Patient-pharmacist communication during a post-discharge pharmacist home visit. Int J Clin Pharm40(3): 712-720.
- Basheti IA, Qunaibi EA, AbuRuz S, Samara S, Bulatova NR (2013) Home medication reviews in a patient care experience for undergraduate pharmacy students. Am J Pharm Educ 77(8): 173.
- Ahn J, Park JE, Anthony C, Burke M (2015) Understanding, benefits and difficulties of home medicines review - patients' perspectives. Aust Fam Physician 44(4): 249-253.
- Dhillon AK, Hattingh HL, Stafford A, Hoti K (2015) General practitioners' perceptions on home medicines reviews: a qualitative analysis. BMC Fam Pract 16: 16.
- Swain L, Barclay L (2015) Medication reviews are useful, but the model needs to be changed: Perspectives of Aboriginal Health Service health professionals on Home Medicines Reviews. BMC Health Serv Res 15: 366.
- Chen TF (2016) Pharmacist-Led Home Medicines Review and Residential Medication Management Review: The Australian Model Drugs Aging 33(3): 199-204.
- El Hajj MS, Hammad AS, Afifi HM (2014) Pharmacy students' attitudes toward pharmaceutical care in Qatar. Ther Clin Risk Manag 10: 121-9.
- Okonta JM, Okonta EO, Ofoegbu TC (2012) Barriers to Implementation of Pharmaceutical Care by Pharmacists in Nsukka and Enugu metropolis of Enugu State. J Basic Clin Pharm 3(2): 295-8.
- Acheampong F, Anto BP (2015) Perceived barriers to pharmacist engagement in adverse drug event prevention activities in Ghana using semi-structured interview. BMC Health Serv Res 15: 361.
- Wick JY (2015) 5 Tips for Improving Communication in the Pharmacy. Pharmacy Times® June 18.
- Phokeo V, Hyman (2007) Provision of pharmaceutical care to patients with limited English proficiency. Am J Health Syst Pharm.;64(4): 423-9.
- Fakeye TO, Adisa R, Olukotun RT, Morawo PK (2017) Hospital and community pharmacists' perception of the scope, barriers and challenges of pharmacy practice-based research in Nigeria. Pharm Pract (Granada) 15(1): 881.
- Kaplan G, Lopez MH, McGinnis JM (2015) Committee on Optimizing Scheduling in Health Care; Institute of Medicine; editors. Transforming Health Care Scheduling and Access: Getting to Now. National Academies Press (US) 2, Issues in Access, Scheduling, and Wait Times, Washington (DC), USA.
- Newton GD (2006) Chapter 123. Ambulatory Patient Care. In: David B. Troy, Paul Beringer (Eds.), Remington The Science and Practice of Pharmacy (21st edn), Lippincott Williams & Wilkins.
- van Baal P, Morton A, Severens JL (2018) Health care input constraints and cost effectiveness analysis decision rules. Soc Sci Med 200: 59-64.
- Gobis B, Yu A, Reardon J, Nystrom M, Grindrod K, et al. (2018) Prioritizing interprofessional collaboration for optimal patient care: A call to action. Can Pharm J (Ott) 151(3): 170-175.
- Lyngsø AM, Godtfredsen NS, Frølich A (2016) Interorganisational Integration: Healthcare Professionals' Perspectives on Barriers and Facilitators within the Danish Healthcare System. Int J Integr Care 16(1): 4.
- Kaiser L, Bartz S, Neugebauer EAM, Pietsch B, Pieper D (2018) Interprofessional collaboration and patient-reported outcomes in inpatient care: protocol for a systematic review. Syst Rev 7(1): 126.
- Miller CJ, Kim B, Silverman A, Bauer MS (2018) A systematic review of team-building interventions in non-acute healthcare settings. BMC Health Serv Res 18(1): 146.
- Houle SK, Grindrod KA, Chatterley T, Tsuyuki RT (2014) Paying pharmacists for patient care: A systematic review of remunerated pharmacy clinical care services. Can Pharm J (Ott) 147(4): 209-232.
- Tannenbaum C, Tsuyuki RT (2013) The expanding scope of pharmacists' practice: implications for physicians. CMAJ 185(14): 1228-1232.
- Kliethermes MA. (2017) Understanding health care billing basics. Pharm Today 23(7): 57-68
- Schepel L, Lehtonen L, Airaksinen M, Ojala R, Ahonen J et al. (2018) Medication reconciliation and review for older emergency patients requires improvement in Finland. Int J Risk Saf Med 30(1): 19-31.
- Lenssen R, Schmitz K, Griesel C (2018) Comprehensive pharmaceutical care to prevent drug-related readmissions of dependent-living elderly patients: a randomized controlled trial. BMC Geriatr 18(1): 135.
- Earls G, Reinhold JA (2012) Chapter 1. Approach to the patient and patient centered care process. In: Jennifer A Reinhold (Eds.), Grace Earl. Clinical Therapeutics Primer: Link to the Evidence for the Ambulatory Care Pharmacist, published by Jones & Bartlett Publishers, p. 10.
- Problem identification and prioritization.
- Vadher D, Cannon BC (2006) Chapter 122. Development of a Pharmacy Care Plan and Patient Problem Solving. In: David B Troy, Paul Beringer (Eds.), of Remington The Science and Practice of Pharmacy (21st edn), Lippincott Williams & Wilkins.
- Wheeler AJ, Scahill S, Hopcroft D, Stapleton H (2018) Reducing medication errors at transitions of care is everyone's business. Aust Prescr 41(3): 73-77.
- Viswanathan M, Kahwati LC, Golin CE, (2014) Medication Therapy Management Interventions in Outpatient Settings [Internet]. Agency for Healthcare Research and Quality (US); (Comparative Effectiveness Reviews, No. 138.) Appendix A, Literature Search Strategies, Rockville (MD), USA.
- Littauer SL, Dixon DL, Mishra VK, Sisson EM, Salgado TM (2017) Pharmacists providing care in the outpatient setting through telemedicine models: a narrative review. Pharm Pract (Granada) 15(4): 1134.
- Telehealth (2017) Increasing Access to High Quality Care by Expanding the Role of Technology in Correctional Medicine. J Clin Med 6(2): 20.
- What is the difference between telemedicine, telecare and telehealth?
- American Telemedicine Association. Telemedicine Glossary.
- Center for Connected Health Policy at the National Telehealth Policy Resource Center. NC State Law Telemedicine/Telehealth Definition., USA.
- Vogenberg FR, Santilli J (2018) Healthcare Trends for Am Health Drug Benefits 11(1): 48-54.
- Parker S, Prince A, Thomas L (2018) Electronic, mobile and telehealth tools for vulnerable patients with chronic disease: a systematic review and realist synthesis. BMJ Open 8(8): e019192.
- Stefano GB, Kream RM (2018) The Micro-Hospital: 5G Telemedicine-Based Care. Med Sci Monit Basic Res 24: 103-104.
- Clarke JL, Bourn S, Skoufalos A, Beck EH, Castillo DJ (2017) An Innovative Approach to Health Care Delivery for Patients with Chronic Conditions. Popul Health Manag 20(1): 23-30






























