Anesthesia Management for a With Walker Warburg Syndrome: Are Optic Nerve Sheat Diameter and Magnetic Resonance Imaging Useful?
Ahmet Besir1*, ErsagunTugcugil1, SaylanSedat1, Akdoğan Ali1, Kaya SelUmut1 and Cömert Yalcın Hatice Sonay2
1Department of Anesthesiology and Critical Care, Turkey
2Department of Pediatric Surgery, Turkey
Submission: November 27, 2018;Published: December 18, 2018
*Corresponding author: Ahmet Besir, Department of Anesthesiology and Critical Care, Turkey
How to cite this article: Ahmet B, ErsagunT, Saylan S, Akdoğan A, Kaya S U, et all. Anesthesia Management for a With Walker Warburg Syndrome: Are Optic Nerve Sheat Diameter and Magnetic Resonance Imaging Useful?. J of Pharmacol & Clin Res. 2018; 6(4): 555695. DOI: 10.19080/JPCR.2018.06.555695
Abstract
Anesthetic management of children with Walker-Warburg Syndrome (WWS) is highly important since the airway management can be difficult due to hydrocephalus and orofacial anomalies, and the patients are at increased risk for intra- and post-operative complications due to the probability of malignant hyperthermia. 5-day-old male child weighing 3.2kg who had been born by cesarean section at the 37th week of gestation was planned for elective ventriculoperitoneal shunt placement due to the presentation of severe hydrocephalus. As WWS is a multisystem disorder, minimally invasive methods such as ultrasonographic measurement of optic nerve sheat diameter and MRI examination can be safely and effectively used in airway management, and evaluation of intracranial pressure changes during the anesthetic management of neonates. To present different methods of anesthesia management in newborns with WWS who expected difficult intubation and an increase in intracranial pressure.
Keywords: Walker-warburg syndrome; Optic nerve sheat Diameter; General anesthesia
Abbreviations: WWS: Walker Warburg Syndrome; CMD: congenital muscular dystrophy; MH: malignant hyperthermia; ICP: intracranial pressure; ONSD: optic nerve sheath diameter; VPS: ventriculoperitoneal shunt
Introduction
Walker-Warburg syndrome (WWS) is a rare, autosomal-recessive congenital muscular dystrophy (CMD) [1-2]. The diagnosis is often made based on the presence of four criteria: type II lissencephaly, cerebellar anomaly, retinal malformation, and CMD [3-5]. WWS is the most severe form of CMD, with the patients mostly dying before 3 years of age as a result of pneumonia, epileptic seizure, hyperthermia, or ventricular fibrillation. Clinical manifestations are present at birth or appear during early infancy, and the diagnosis is often established by prenatal ultrasonography. Typical laboratory findings include increased creatine kinase (CK) levels, myopathic/dystrophic muscle pathology, and altered α-dystroglycan [6]. In children with WWS, airway management can be difficult due to hydrocephalus and orofacial anomalies. As WWS is a neuromuscular disease, it can also be accompanied by malignant hyperthermia (MH); therefore, anesthetists should be alerted against serious intra- and post-operative complications. In the presence of hydrocephalus, intraoperative intracranial pressure (ICP) monitoring becomes necessary. In this report, we aimed to present our experience in the anesthetic management of a newborn diagnosed with WWS who was also present with malignant hyperthermia, difficult intubation, and increased ICP and underwent ultrasonographic measurement of the optic nerve sheath diameter (ONSD) and a magnetic resonance imaging (MRI) of the airway.
Case Presentation
A 5-day-old male child weighing 3.2 kg who had been born by cesarean section at the 37th week of gestation was admitted to the neonatal intensive care unit (ICU) immediately after birth due to severe hydrocephalus and respiratory distress. The patient initially received noninvasive positive-pressure ventilation and was planned for elective ventriculoperitoneal shunt (VPS) placement by the Neurosurgery department due to the presentation of hydrocephalus. The patient was also evident with CMD, and preoperative physical examination showed macrocephaly, microphthalmia, bilateral cataract and persistent pupillary membranes, retrognathia, and silundum atrial septal defect. Laboratory findings were normal except for creatine phosphokinase level of 37,553uL1 (normal range, 20-200uL-1). MRI of the brain and spine showed radiographic signs suggestive of WWS, including dilated ventricles, severe hydrocephalus, and hypoplasia of the cerebellar vermis and the corpus callosum. Additionally, hypoplasia of the brainstem, cerebellar polymicrogyria, and cervical syringomyelia were also detected (Figure 1).
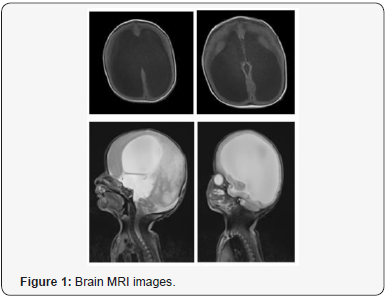
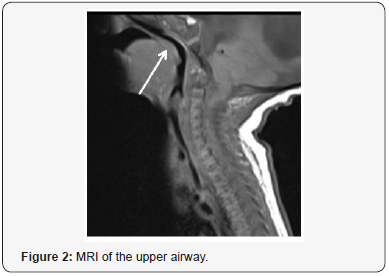
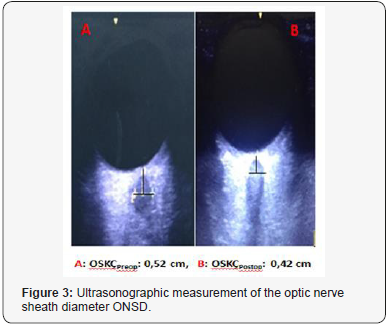
Prior to the surgery, a preoperative neurological examination revealed a risk of MH; therefore, the vaporizers were removed from the anesthesia machine and the machine was flushed with pure oxygen at 10L/min for 30 min using a carbon dioxide absorbent. After a 3-h fasting period, the patient was transferred to the operating room and standard monitorization (pulse oximetry, electrocardiography, non-invasive blood pressure, end-tidal carbon dioxide, temperature, and bispectral index) was performed. In addition, gas concentration of inhaled anesthetics was closely monitored throughout the surgery to monitor possible changes. For the probability of difficult intubation, oropharyngeal airways, laryngeal masks, and other essential equipment at varying sizes were prepared. For the probability of MH, dantrolene sulfate and cold intravenous fluids were maintained in the operating room throughout the surgery. Due to the presentation of hydrocephalus, a noninvasive method, ultrasonographic measurement of the ONSD, was used for monitoring the ICP changes throughout the surgery. After achieving mask ventilation, anesthesia was induced with iv atropine (0.01μg/kg-1), midazolam (0.2mg), remifentanil (1μg kg-1), and propofol (2mg kg-1). The larynx could not be visualized on laryngoscopy by conventional midline approach; therefore, the tip of the epiglottis was visualized by the aid of MRI images using the lateral approach with a Miller 1 straight blade, and endotracheal intubation (ETI) was successfully performed using a 3.5mm uncuffed (Figure 2). The endotracheal tube placement was confirmed by capnography and auscultation of lungs. Volume-controlled ventilation was performed, and the tidal volume was set at 6-8mg kg-1 to maintain normocapnia. Following intubation, anesthesia was maintained with remifentanil and propofol administered in intermittent bolus injection of 50:50 oxygen/air mixture titrated to BIS value 50-60. No muscle relaxant was used throughout the surgical procedure. Fluid management was performed by the administration of balanced electrolyte solution based on the calculation of the perioperative fluid eficits and basal fluid requirement of the patient. Due to the risk of MH, continuous temperature monitoring was performed using a rectal thermometer and the temperature was maintained between 35.5- 36.7 °C. The ONSD value decreased from the preoperative value of 0.52cm to the postoperative value of 0.42cm (Figure 3). The surgical procedure lasted for 45min and extubation was achieved uneventfully when the patient was full-awake. The patient was then transferred to the neonatal ICU.
Discussion
Walker-Warburg syndrome is a rare multisystem disorder affecting the musculoskeletal, central nervous, and urogenital systems, accompanied by orofacial anomalies. This multisystem involvement leads to increased risk of complications; therefore, a careful anesthetic management is of paramount importance. Moreover, prevention of complications in the pre-and postoperative periods and during anesthetic induction/maintenance can be life-saving during the anesthetic management of complex syndromes like WWS. Difficult intubation is a potentially important problem that can be encountered during the anesthetic induction of patients with WWS. Therefore, appropriate airway equipment should be prepared before the induction of general anesthesia. In our patient, we employed radiographic images for the management of difficult intubation since no video laryngoscopy was available in our clinic.
Moreover, an MRI examination of the upper airway was performed to evaluate the probable difficulties that could be encountered in the management of airway during intubation. On T1-weighted MRI images, the radix was seen as protruding towards the lingula posteriorly into the oral cavity, thereby leading to a risk of airway obstruction. However, apart from this obstruction, no other obstruction was detected in the oropharynx, laryngopharynx, or trachea (Figure 2). As a result of these conditions, the larynx could not be visualized on laryngoscopy via conventional midline approach. Therefore, the tip of the epiglottis was visualized using the lateral approach with a Miller 1 straight blade, which has been shown to be a beneficial approach in children with micrognathia, and ETI was achieved uneventfully. Additionally, this approach was also useful since it by passed soft tissues and the tongue.
The risk of MH is a major problem in WWS, as in other myopathies. In our patient, anesthetic agents such as halogenated anesthetics and succinylcholine were avoided considering that they could result in rhabdomyolysis or non-specific hypermetabolic response due to the increased risk of MH. Patients with WWS are at increased risk for renal dysfunction since WWS can be accompanied by cardiac and genitourinary anomalies. In our patient, adequate fluid management was maintained throughout the procedure to avoid renal dysfunction and to minimize cardiovascular depression. Children with WWS may have severe hydrocephalus that may cause ICP changes both before and after anesthetic induction. Accordingly, the primary aim in perioperative anesthetic management should be to maintain ICP within normal limits to provide adequate cerebral circulation. To achieve this, care should be taken to avoid drugs and applications that may cause increased ICP. Ultrasonographic measurement of the ONSD has recently emerged as a popular noninvasive method for monitoring ICP changes [7]. To our knowledge, there are very few studies that have used this method for monitoring the ICP changes and evaluating the effectivity of VPS placement in children undergoing VPS placement due to hydrocephalus [8].
Our patient was also present with severe hydrocephalus and the ICP changes were monitored using ultrasonographic measurement of ONSD both pre and post-operatively. Similarly, in a previous prospective study, Choi et al. also monitored the ICP changes using ultrasonographic measurement of ONSD in children aged 1-19 years and reported that there was a significant decrease between pre- and post-operative ONSD. The authors also suggested that this method is a rapid, noninvasive, and guiding method for the assessment of ICP changes and the evaluation of the effectivity of VPS placement. Although a number of ONSD values ranging between 0.5 and 0.59cm have been reported to indicate increased ICP in adults, there is limited data regarding the ONSD values for child patients, particularly for neonates [8]. In a previous study, Helmke et al. suggested that an ONSD of >0.4cm indicates increased ICP in children younger than 4 years of age [9]. In our patient, ONSD decreased from the preoperative value of 0.52cm to the postoperative value of 0.42cm, which could be associated with the effectivity of VPS placement. In conclusion, in the management of perioperative and postoperative anesthesia of children with WWS, which is a syndrome affecting many systems, we think that serial ONSD measurements with USG and MRI effective and safe.
References
- Walker AE (1942) Lissencephaly Arch Neurol Psychiatry 48(1): 13-29.
- Mostacciuolo ML, Miorin M, Martinello F, Angelini C, Perini P, et al. (1996) Genetic epidemiology of congenital muscular dystrophy in a sample from the North-East Italy. Hum Genet 97(3): 277-279.
- Dobyns WB, Kirkpatrick JB, Hittner HM, Roberts RM, Kretzer FL, et al. (1985) Syndromes with lissencephaly II: Walker-Warburg and cerebro oculo-muscular syndromes and a new syndrome with type II lissencephaly. Am J Med Genet 22(1): 157-195.
- Dobyns WB, Pagon RA, Amstrong D(1989) Diagnostic criteria for Walker-Warburg syndrome. Am J Med Genet 32(2): 195-210.
- Dogfight J, Sassani JW, Suzuki K, Ladda RL (1984) Cerebro-ocular Dysplasia-Muscular Dystrophy (COD-MD) syndrome. Acta Neuropathol 65(2): 110-123.
- Vajsar J, Schachter H (2006) Walker-Warburg syndrome. Orphanet J Rare Dis 1:
- Wang LJ, Chen LM, Chen Y, Bao LY, Zheng NN, et al. (2018) Ultrasonography Assessments of Optic Nerve Sheath Diameter as a Noninvasive and Dynamic Method of Detecting Changes in Intracranial Pressure. JAMA Ophthalmol 136(3): 250-256.
- Choi SH, Min KT, Park EK, Kim MS, Jung JH, et al. (2015) Ultrasonography of the optic nerve sheath to assess intracranial pressure changes after ventriculo-peritoneal shunt surgery in children with hydrocephalus: a prospective observational study. Anaesthesia 70: 1268-
- Helmke K, Hansen HC (1996) Fundamentals of transorbital sonographic evaluation of optic nerve sheath expansion under intracranial hypertension II. Patient study. Pediatr Radiol 26(10): 706-710.






























