Prevalence of Associated Risk Factors of Hypertension In Libyan Patients
Yousef A Taher and Fathi M Sherif*
Department of Pharmacology and Clinical Pharmacy, University of Tripoli, Libya
Submission: October 24, 2017;Published: November 08, 2017
*Corresponding author: Fathi Mohamed Sherif, Department of Pharmacology and Clinical Pharmacy, University of Tripoli, Libya, Tel: 218 91 211 7258; Email: Fmosherif@yahoo.com
How to cite this article: Taher Y A, Sherif F M. Prevalence of Associated Risk Factors of Hypertensionv In Libyan Patients. J of Pharmacol & Clin Res. 2017; 4(1): 555629. DOI: 10.19080/JPCR.2017.04.555629.
Abstract
Hypertension is a chronic disease which is challenge for public health professionals and it has been recognized as a leading and important modifiable risk factor for cardiovascular disease. This study was aimed to explore the prevalence of associated risk factors of hypertension in Libyan patients. 200 patients (M: F, 1: 1) from different areas of Tripoli, Libya diagnosed with hypertension and receiving treatment from Tripoli Medical Center were included in this study. The major findings demonstrate that about 50% of the patients are obese (BMI > 30 kg/m2) (Male: 30% and female 58%). A significant sex prevalence of BMI and smoking was detected. A trend in prevalence of diastolic with regard to age of men and women was found. No prevalence of family history, physical inactivity, smoking and BMI among all the patients was assessed. Risk factors as physical inactivity, smoking and obesity are common among the Libyan patients. In conclusion, knowing the common causes allows a more operative approach in hypertension prevention and therapy in Libya.
Keywords: Hypertension; Cardiovascular disease; Risk Factor; Obesity; Physical Inactivity; Libya
Introduction
Universally, more than one billion persons are affected with hypertension. It is a chronic disease in which systemic arterial blood pressure is increased to the level that causes cardiovascular damage [1]. Hypertension is a serious medical and expensive public health problem and a challenge for community health care professionals. It is continuous to be the leading risk factor for death. Untreated and uncontrolled hypertensions usually lead to various complications [2]. 90% of the cases are primary hypertension with no obvious underlying medical cause and tends to run in families, age, sex and race can influence risk for the disease. Other life-style choices behaviors like smoking cigarettes, eating an unhealthy diet are very possible to play a role in hypertension [3,4]. Thus, associated risk factors known to be connected with hypertension are obesity, diabetes, high sodium intake, stress and physical inactivity [2]. Hypertension is the most significant avoidable risk factor for premature death [5,6]. While, therapy of hypertension reduces the excess risk of associated diseases, the risk remains greater in matched normotensive controls. The remaining cases (10%) are linked with identified diseases (known as secondary hypertension).When the identified disease is treated, blood pressure returns to normal or significantly lowered [4,7].
Treatment of hypertension in patients with diabetes and chronic kidney problems is important to reduce the risk of cardiovascular disease (CVD) by 25-50% [1,3]. Life-style changes such as loss of weight, quit tobacco use, reduce alcohol drinking, eat a healthy diet and get enough physical activity are behaviors that decrease risk for CVD [8], plus the pharmacological therapy [9,10]. Hypertension is a risk factor for development and worsening of diabetes mellitus (DM) complications and the coexistence of hypertension in diabetic patients deeply enhances developing CVD and kidney diseases [3,11]. Common risk factors for DM are age (over 40 years), unhealthy diet, excess body fat, physical inactivity, genetics and family history [12,13]. The ratio of people with DM rises with age and is more in black and minority ethnic groups. Obesity, impaired glucose tolerance and DM are associated with increased incidence of hypertension, CVD and chronic kidney diseases [2,14,15]. The prevalence of hypertension in patients with type-II DM is 3-fold higher than in patients without DM [16]. Studies conducted in Framingham population with DM showed that the presence of hypertension was a resulting risk factor for the presence of CVD suggesting 2-fold increased risk of CVD events and deaths in diabetic with hypertension [17].
The association between hypertension and DM can in part be explained by the presence of a maladaptive interaction of factors as excessive caloric intake, decreased activity and linked insulin resistance, chronic activation of rennin-angiotensin-aldosterone system, sympathetic nervous system and oxidative stress [18]. The epidemics of obesity, inactive lifestyle and aging have added to the current high incidence of DM and hypertension. To the best of our knowledge, no previous studies of hypertension and modifiable risk factors in Libya have been reported. Thus, this study was aimed to explore the distribution of associated risk factors of hypertension in Libya and to characterize the modifiable risk factors among the patients.
Materials and Methods
Study design: A prepared questionnaire contains data about patients with known history of hypertension was used in this study. The questionnaire was designed and validated by the staff-teaching members of Pharmacology and Clinical Pharmacy, Faculty of Pharmacy, University of Tripoli, Tripoli, Libya. All data included in this study were obtained from patients registered and treated at Tripoli Medical Center, Tripoli, Libya. The questionnaire interviews were conducted face-to-face by investigators between February and May, 2015. This survey was approved by the Ethics Committees of University of Tripoli (UOT, 2015) and Tripoli Medical Center (TMC, 2015). All procedures were in accordance with the ethical standards of Helsinki Declaration and all participants provided written informed consent before contributing the investigation.
Study Participants: a total of 200 adult known hypertensive Libyan patients with an average age of 64.3 13.5 years (mean SD) and had lived in Tripoli or near for more than six months were included in this study. Patients with serious diseases and pregnant women were excluded.
Survey: the structured questionnaire was about prevalence and risk factors related to hypertensive patients and cover three parts with specific different variables related to hypertensive. Socio-demographic information including sex, age, education level and marital status, diet, physical activity, tobacco consumption, personal and family health history, medication profile and coronary risk factors. Current smoking was defined as having smoked more than 10 cigarettes per day for the last six months and still smoking during the study. Physical activity was divided into three types according to the frequency of activity in the past 30 days: less or twice a week, more than a twice a week. Diet status was also divided into three types, vegetable-consumption diet, meat-consumption diet, and fruitconsumption diet. Vegetable, meat and fruit consumption were defined as item intake per day.
Statistical analysis: data are expressed as percentages or mean SD. In all the statistical data, P value of < 0.05 was taken as a significant. Logistic regression was used to assess the strength of association between the dependent and independent variables under the study. The odds ratio (OR) and 95% confidence interval (CI) were calculated in logistic regression analysis. Statistical comparisons were done by the use of statistical program Graph Pad Prism (Graph Pad Software Inc., USA).
Results
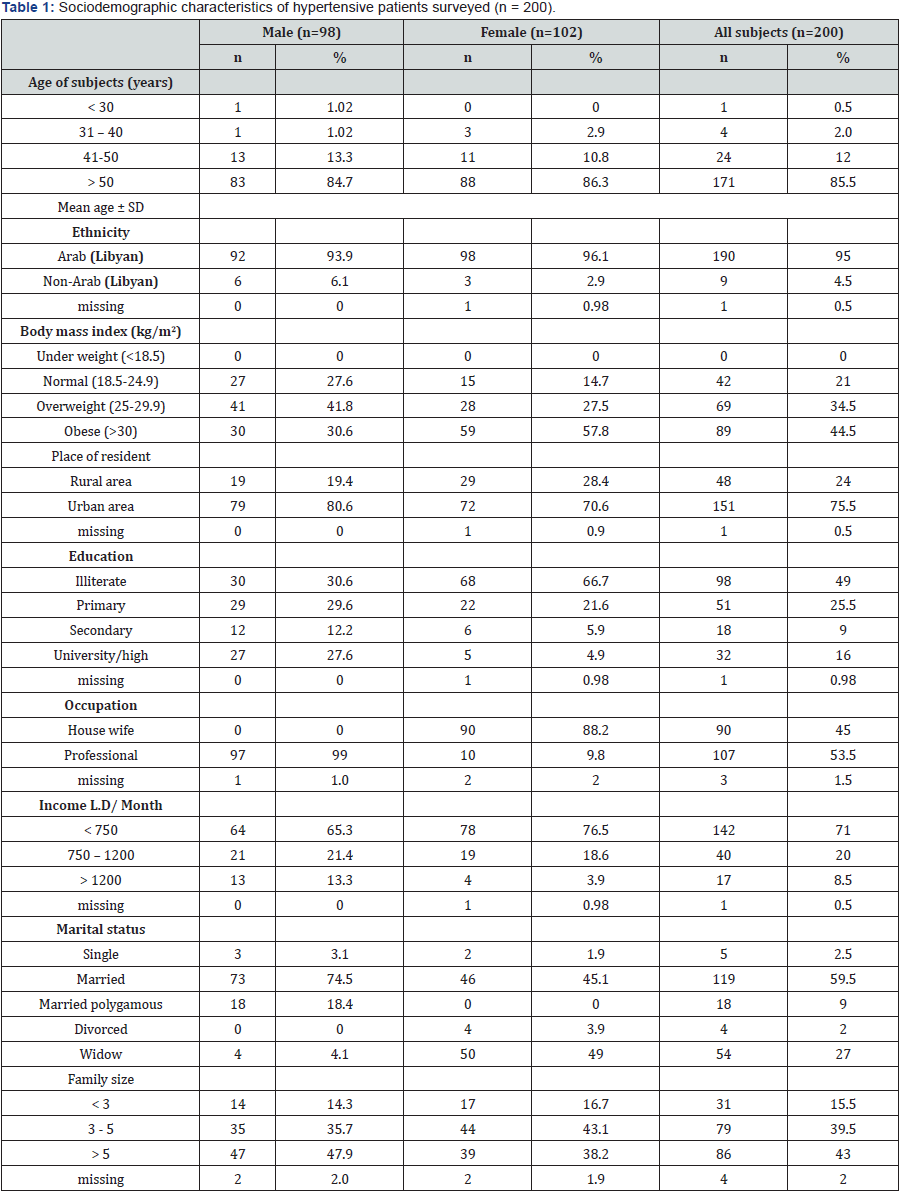
Among the 200 questionnaires distributed 200 participant living in both urban (75%) and rural (24%) areas agreed to participate (100%) and responded to the study. The distribution of reported age was as follows: under 30 years, 0.5%; 30- 40 years, 2%; 41-50 years, 12% and above 50 years, 85.5%. The frequency distributions of age among men and women participating in this study are depicted in Table 1. Displays the sociodemographic descriptions of the hypertensive patients with regard to ethnicity, body mass index, skin color, education level, occupation, marital status, monthly income and family size in the population surveyed. Of the researched group, 49% were illiterate and 16% were literate, 44.5 were obese (BMI >30 Kg/ m2), 2.5% never married and 43% belongs to of more than 5 persons per family (Table 1).
In addition, the present study investigated the pattern of some diseases among the participating family history, revealing that the most common disease associated with hypertension was diabetes mellitus (60.5%, 121 case), followed by CVD (34.5%, 69 case), renal diseases (12.5%, 25 case) and thyroid problems (6.5%, 13 case). Only 28.5% of the total number of subjects their family history had no specific disease (data not shown).
The prevalence of risk factors of hypertension according to sex with 95% CI is illustrated in Table 2. The prevalence of obesity of BMI 25 Kg/m2 and BMI 30 Kg/m2 were statistically significantly higher among women. While, men reported significantly higher regarding the prevalence of smoking among subjects. In addition, there was no significant tendency for all risk factors with respect to sex in selected subjects. Prevalence of risk factors for hypertension according to age in men and women are shown in Table 3. Family history, BMI ≥ 25 Kg/m2, BMI 30 Kg/m2 and smoking as risk factors for hypertension were found low in 50 years and above age group in case of men. Prevalence of physical inactivity was low in 41-50 years of age group in case of men. However there was a significant linear trend for BMI 30 Kg/m2 (P<0.01) and physical inactivity (not significant, P=0.08) among men with respect to age. Physical inactivity, smoking, BMI ≥ 25 Kg/m2 and BMI 30 Kg/m2 were found more in above 50 years of age group in case of women. While, family history of hypertension was found low in case of women in 41-50 years of age group. In addition, data indicated that there was no significant linear trend for all risk factors with respect to age group over all subjects.
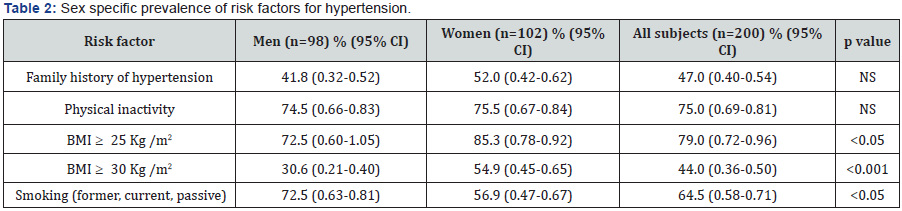
Data are prevalence expressed as percentages. Values in parenthesis are 95 % CI, BMI= body mass index. A p value indicates the significance of comparison of prevalence between men and women. NS= not significant.
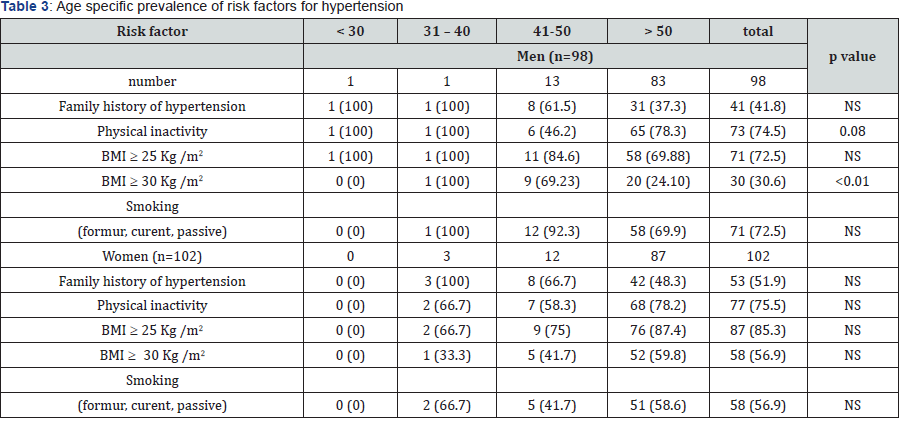
Values in parenthesis are percentages, BMI= body mass index. A p value indicates trend in prevalence with respect to age, NS= not significant.
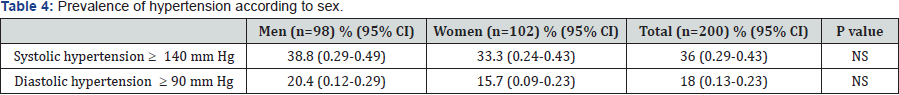
Data in parenthesis indicate 95% CI. p value indicates the comparison between men and women. NS= not significant.
p value indicates trend in prevalence with respect to age; NS= not significant.
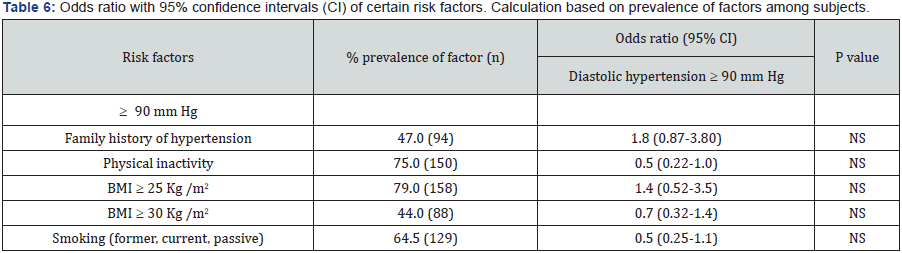
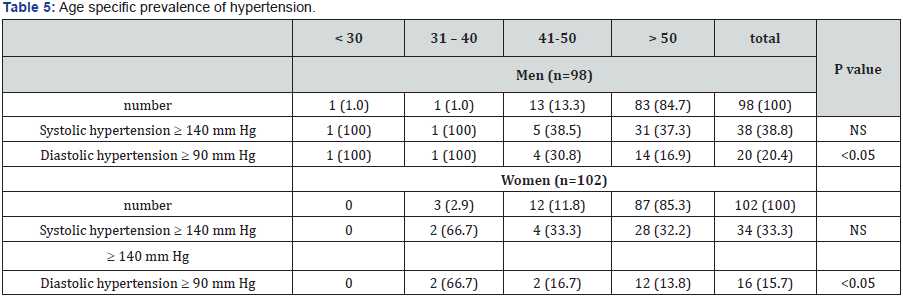
Prevalence of systolic and diastolic hypertension according to sex is shown in Table 4. The differences in prevalence of systolic and diastolic hypertension between men and women were not statistically significant. Prevalence of systolic and diastolic hypertension according to age is shown in Table 5. Prevalence of systolic and diastolic hypertension was lower in age group of 50 years and above in case of men and women. There was significant linear trend in prevalence of diastolic hypertension with respect to age group in men and women, whereas systolic hypertension was not. Data regarding prevalence of risk factors including odds ratio with 95% CI in diastolic hypertensive are shown in Table 6. Prevalence of risk factors was significantly low and poor in subjects having diastolic hypertension. Logistic regression analysis showed that presence of hypertension within the family “family history of hypertension” was approximately twice as likely to develop diastolic hypertension of 90 mmHg. With the exception of BMI 25 Kg/m2 patients were approximately half as likely to develop diastolic hypertension of 90 mmHg (physical inactivity: OR 0.5, 95% CI 0.22-1.0; BMI 30 Kg/m2: OR 0.7, 95% CI 0.32-1.4; and smoking: OR 0.5, 95% CI 0.25-1.1) compared to their respective counterparts (Table 6).
Discussion
A high percentage of hypertensive patients live in lowor middle-income countries. Patients with hypertension are at a high risk for developing different cardiovascular complications. The prevalence of hypertension has increased in some developing countries due to some risk factor associated with pre-hypertension [18-20]. Control of blood pressure and reduction of cardiovascular risk factors are both needed in patients with hypertension. However, in some patients, adequate blood pressure control for a long period cannot usually be achieved and more effective management of hypertension is required [21]. Previous studies have mentioned that multiple risk factors are related to hypertension such as increased age, overweight, obesity, diabetes, and dyslipidemia [2,14,15,22]. In Libya, no previous epidemiological studies had reported the risk factors for hypertension in any region of the country. In this study, most of the patients are older than 50 years and retired people (advanced age or a lesser physical activity), which means hypertension is strongly correlated to the progresses in age. No particular evidence shows that younger patients suffer from primary hypertension, only one patient did suffer from secondary hypertension due to renal artery stenos is. Risk factors such as age (> 45), family history, sex (> 65, F > M) and race are all related to who you are and nothing can do. A greater risk of developing diabetes or hypertension is common in Libya (see below).
The incidence of female patients suffering from hypertension is higher than of the male patients. It is noted that as the family size is increased, the risk of developing the disease is increased (developing gestational hypertension in females) and increasing the financial demands in the family (males responsibility speaking in the mentality of a married person in our domestic population). Strong links between finance and chances of having hypertension and diabetes, the more the income the lesser the chance of developing the diseases. Patients with hypertension have a risk of developing DM (type 2) and are commonly occurring together [23, 24]. Obesity is a substantial overlap between hypertension and DM in mechanisms and etiology [23]. Family history of diabetes is also a risk factor and as previously mentioned females that developed gestational hypertension are at a risk of developing hypertension, as the increasing number of child delivery; the chance of developing hypertension is more. Risk factors related to how you live as lack of physical activity, unhealthy diet (as sodium), being overweight or obese were all considered in the present study. 80% of the patients are overweight or obese which consider as a common risk factor of high blood pressure. A direct relation of obesity and physical activity has also been revealed.
A daily physical activity is needed. However, the possible benefit of physical activity in prevention and therapy of high blood pressure is known but regular exercise is difficult in real life. A potential contributing risk factors as smoking (tobacco use) and stress that raise blood pressure and heart rate, narrows arteries and hardens their walls were evaluated. Thus, a large number of smokers (former, current, passive) among our patients was noted which is in line with a previous Libyan study of high huge heavy smokers in Libyan society [25]. Other common risks factors may also be attributed to hypertension are CVD, migraine and obstructive sleep apneas are among the studied patients. Taking paracetamol or NSAIDs was common in our patients and intake of CNS stimulants such as coffee, tea or energy drinks were highly present among the hypertensive individuals who participated in this study.
A considerable number of patients denied any history of smoking but the summation of passive, former, and current smokers was about two-folds more than the non-smokers (whereas most of the cases were females) this does not mean that they are smoker but does not exclude that they were passive smokers. Increased animal protein consumption is a major risk factor in developing hyperlipidemia which is one of the hazards that leads to hypertension and DM [22,26]. For lipid profile, most patients had cholesterol, triglycerides, and low density lipoproteins (LDL) levels of optimal range in those individuals due to treatment control. However, few patients were not in desirable high density lipoproteins (HDL) range which might need some critical modification in their lifestyle such as physical activity that plays a major protective role in hypertension and related diseases and/or pharmacotherapy.
Conclusion
A high prevalence of associated risk factors of hypertension in Libyan patients. Thus, changes in lifestyle could significantly reduce hypertension related diseases.
Conflict of Interest
The authors declare that the research was conducted in the absence of any financial affairs that could be taken as a conflict of interest.
References
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, et al. (2003) Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 42(6): 1206-1252.
- An SJ, Kim TJ , Yoon BW (2017) Epidemiology, Risk Factors, and Clinical Features of Intracerebral Hemorrhage: An Update. J Stroke 19(1): 3-10.
- Carretero OA, Oparil S (2000) Essential hypertension Part I: definition and etiology. Circulation 101: 329-335.
- Rossier BC, Bochud M and Devuyst O (2017) The Hypertension Pandemic: An Evolutionary Perspective. Physiology (Bethesda) 32(2): 112-125.
- Lewington S, Clarke R, Qizilbash N, Peto R, Collins R (2002) Age-specific relevance of usual blood pressure to vascular mortality: a metaanalysis of individual data for one million adults in 61 prospective studies Lancet 360: 1903-1913.
- Singer DR and Kite A (2008) Management of hypertension in peripheral arterial disease: does the choice of drugs matter? Eur J Vasc Endovasc Surg 35(6): 701-708.
- O Brien E, Beevers DG, Lip Gregory YH (2007) ABC of hypertension. London: BMJ Books, Canada.
- Egan BM (2017) Physical Activity and Hypertension: Knowing Is Not Enough We Must Apply Willing Is Not Enough We Must Do-von Goethe. Hypertension 69(3): 404-406.
- Garjon J, Saiz LC, Azparren A, Elizondo JJ, Gaminde I, et al. (2017) Firstline combination therapy versus first-line monotherapy for primary hypertension. Cochrane Database Syst Rev 1: CD010316.
- Wiysonge CS, Bradley HA, Volmink J, Mayosi BM , Opie LH (2017) Betablockers for hypertension. Cochrane Database Syst Rev 1: CD002003.
- Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A (2003) Acarbose treatment and the risk of cardiovascular disease and hypertension in patients with impaired glucose tolerance: the STOP-NIDDM trial. JAMA 290(4): 486-494.
- De Greef K, Van Dyck D, Deforche B, De Bourdeaudhuij I (2011) Physical environmental correlates of self-reported and objectively assessed physical activity in Belgian type 2 diabetes patients. Health Soc Care Community 19(2): 178-188.
- Murano I, Asakawa Y, Mizukami M, Takihara J, Shimizu K, et al. (2014) Factors increasing physical activity levels in diabetes mellitus: a survey of patients after an inpatient diabetes education program. J Phys Ther Sci 26(5): 695-699.
- Psaltopoulou T, Hatzis G, Papageorgiou N, Androulakis E, Briasoulis A, et al. (2017) Socioeconomic status and risk factors for cardiovascular disease: impact of dietary mediators. Hellenic J Cardiol 58(1): 32-42.
- Sherif FM and Ahmed SS (1997) Diabetes and hypertension. International Diabetes Digest 8: 1-5.
- Ramlo-Halsted BA and Edelman SV (1999) The natural history of type 2 diabetes. Implications for clinical practice. Prim Care 26(4): 771-789.
- Chen G, McAlister FA, Walker RL, Hemmelgarn BR , Campbell NR (2011) Cardiovascular outcomes in framingham participants with diabetes: the importance of blood pressure. Hypertension 57(5): 891-897.
- Sowers JR, Whaley-Connell A and Epstein M (2009) Narrative review: the emerging clinical implications of the role of aldosterone in the metabolic syndrome and resistant hypertension. Ann Intern Med 150(11): 776-783.
- Collier SR and Landram MJ (2012) Treatment of prehypertension: lifestyle and/or medication. Vasc Health Risk Manag 8: 613-619.
- Lauzurica LZ, Izquierdo JQ, Vinuesa JM, Mas JR (2016) Awareness, treatment and control of hypertension in population aged 16 to 90 years old in the Valencia, Spain, 2010 . Rev Esp Salud Publica 90: e1- e12.
- Alami M, El Hattaoui M, Seqat M, Sadik J, Aouad A, et al. (2017) Control of blood pressure and cardiovascular risk in Moroccan patients with newly diagnosed hypertension: a 3-month observational study in primary care. Ther Adv Cardiovasc Dis 11(2): 49-56.
- Nelson RH (2013) Hyperlipidemia as a risk factor for cardiovascular disease. Prim Care 40(1): 195-211.
- Chenung BM and Li C (2012) Diabetes and hypertension: is there a common metabolic pathway? Curr Atherosculer Rep 14(2): 160-166.
- Mengesha AY (2007) Hypertension and related risk factors in type 2 diabetes mellitus (DM) patients in Gaborone City Council (GCC) clinics, Gaborone, Botswana. Afr Health Sci 7(4): 244-245.
- Sherif FM (2017) Nicotine dependence and role of pharmacist in nicotine addiction control. LIMUJ 2(1): 3-11.
- Ruixing Y, Jinzhen W, Weixiong L, Yuming C, Dezhai Y, et al. (2009) The environmental and genetic evidence for the association of hyperlipidemia and hypertension. J Hypertens 27(2): 251-258.






























