- Review Article
- Abstract
- Introduction
- Background
- Armamentarium of Sedative Agents and Combinations for the Pediatric Patient
- Limitations of the Oral Route and Available Agents
- Alternatives to Chloral Hydrate
- Retrospective Data in support of the continued merit in using CH combinations and other commonly employed agents and combinations
- Summary and Final Remarks
- References
The Historical and Contemporary Use of Chloral Hydrate as a Sedative/Hypnotic and Alternatives for Management of Moderate to Severe Childhood Dental Anxiety and Uncooperative Behavior
*John E. Nathan
Diplomate, American Board of Pediatric Dentistry
Fellow and Master, American Society of Dentistry for Children
Adjunct Professor, Department of Pediatric Dentistry, University of Alabama, Birmingham,
Case Western Reserve University, Cleveland
Associate Clinical Professor, Department of Otolaryngology, Northwestern University, Feinberg
School of Medicine, Chicago
Editor in Chief, Journal of Pediatrics and Neonatal Nursing & Journal of Otolaryngology and Rhinology
Submission: August 05, 2016; Published: September 08, 2016
*Corresponding author: John E. Nathan, Diplomate, American Board of Pediatric Dentistry Fellow and Master, American Society of Dentistry for Children Adjunct Professor, Department of Pediatric Dentistry, University of Alabama, Birmingham Case Western Reserve University, Cleveland Associate Clinical Professor, Department of Otolaryngology, Northwestern University, Feinberg School of Medicine, Chicago Editor in Chief, Journal of Pediatrics and Neonatal Nursing & Journal of Otolaryngology and Rhinology” Tel:630574-7336; Fax: 6305749331; Email:jnathandds@gmail.com
How to cite this article: John E. N. The Historical and Contemporary Use of Chloral Hydrate as a Sedative/Hypnotic and Alternatives for Management of Moderate to Severe Childhood Dental Anxiety and Uncooperative Behavior. J of Pharmacol & Clin Res. 2016; 1(4): 555568. DOI: 10.19080/JPCR.2016.01.555568
- Review Article
- Abstract
- Introduction
- Background
- Armamentarium of Sedative Agents and Combinations for the Pediatric Patient
- Limitations of the Oral Route and Available Agents
- Alternatives to Chloral Hydrate
- Retrospective Data in support of the continued merit in using CH combinations and other commonly employed agents and combinations
- Summary and Final Remarks
- References
Abstract
Selected for its wide range of safety when using reasonable and responsible doses alone and in combination, Chloral Hydrate (CH) is an agent that has long been effective for pediatric dental management of challenging and disruptive behaviors. Misuse and abuse, however, has recently cast disfavor of this time honored and extensively tested regimen resulting in discontinuation in production of its oral formulation, leaving a void in the arsenal of mid-to-long duration regimens for in-office management. This article discusses the indications, merit, and limitations of this agent in the context of pediatric dental practice selected for young children with limited cooperative potential where moderate to extensive treatment demands exist and the option of utilizing general anesthesia is not viable. Considerable study of this agent and agents in current use are reviewed with respect to safe and appropriate dosing and case selection, along with contemporary constraints which have limited availability and use.
Keywords: Pediatric Sedation; Chloral Hydrate; Safety
- Review Article
- Abstract
- Introduction
- Background
- Armamentarium of Sedative Agents and Combinations for the Pediatric Patient
- Limitations of the Oral Route and Available Agents
- Alternatives to Chloral Hydrate
- Retrospective Data in support of the continued merit in using CH combinations and other commonly employed agents and combinations
- Summary and Final Remarks
- References
Introduction
Due to a paucity of well-designed research, sedation for the pediatric dental patient is best regarded in large part as more art than science. Its primary intent serves to permit completion of needed treatment where cooperative potential is lacking in an office setting while maintaining minimally depressed consciousness and avoiding need for physical restraint [1]. When and where successful, it can serve to circumvent need for unconscious techniques such as costly use of general anesthesia, hospital and surgical center admissions. Induction of inadvertent or unintended levels of (deep) sedation is to be avoided wherever possible [2]. For this purpose, the armamentarium of agents and combinations using dosages which insure consciousness and safety is, however, limited to about a few sedative agents. Achieving this objective necessitates astute clinician awareness and vigilance, knowledge and experience in selecting and dosing for the needs of a particular patient. The literature over the past several decades, while plentiful, has been plagued by numerous methodological design flaws, resulting in little consensus as to how to define and measure clinical success, and how to determine appropriate dosing for varying levels of childhood apprehension and interfering behavior. While emphasis has focused on establishment of guidelines to assure patient safety, non-compliance following such guidelines has unveiled numerous adverse events which appear to contribute to further shrinkage of an already limited armamentarium of agents, some of which have long proven safe and effective. This paper will elaborate on this aspect of pediatric sedation [3].
Among the sedative agents available for management of challenging young pediatric dental behaviors, chloral hydrate has enjoyed widespread use and an historically long and broad range of safety over the past half century [4-9]. Despite frequent if not abundant use and success, the manufacture of chloral hydrate in its oral elixir formulation has ceased. Across the U.S. several state regulatory bodies, some institutional settings, and numerous advanced training programs have removed this agent from its formularies and authorization for its use, either alone or in combination with other adjunctive agents. This manuscript attempts to examine its longstanding applications in the field of pediatric dental practice where its use has been helpful to permit thousands of young children on a daily basis to avoid need for hospitalization and general anesthesia for management of invasive and extensive dental disease. Instances of misuse, gross overdosing, and poor clinician judgment have resulted in morbidity and catastrophic outcomes. Production and advocacy of its continued use has become limited to pharmaceutically compounded preparation from its tablet form (still manufactured). The dilemma which remains, however, relates currently to limited pharmacists willing to compound medications. Most conventional proprietary pharmacies express they simply do not have time to permit formulations to be prepared.
Analysis of the origin of cases of morbidity and mortality are described below to illustrate that such occurrences are avoidable where compliance with existing guidelines for the safe and effective use of pediatric sedation is strictly enforced. Extensive retrospective case data accumulated over the past 35 years by this author is presented to illustrate the safety and track record of chloral hydrate and its continued potential as a sedative agent for the apprehensive child patient.
- Review Article
- Abstract
- Introduction
- Background
- Armamentarium of Sedative Agents and Combinations for the Pediatric Patient
- Limitations of the Oral Route and Available Agents
- Alternatives to Chloral Hydrate
- Retrospective Data in support of the continued merit in using CH combinations and other commonly employed agents and combinations
- Summary and Final Remarks
- References
Background
CH falls in the class of sedative- hypnotic agents which has the capacity to induce somnolence. Its ability to overcome significant behavioral resistance in children and long duration of action made it a logical choice to help many apprehensive young and pre-cooperative children cope with invasive and unpleasant aspects of dental treatment. Safe and effective dosage determination has long been somewhat challenging if not controversial. Gastrointestinal upset of this sedative agent has further complicated its use. Dosing has ranged from 25 mg/ kg (sedative dose) to 50 mg/kg (hypnotic dose) with higher dosing (75-100 mg/kg) reportedly advocated when this range proved ineffective by some disciplines in need of a quiescent non-moving subject for diagnostic or interventional procedures.
Since the mid 1980’s when attentions justifiably began to focus on issues of safety and levels of depression encountered, a plethora of studies emerged to provide insight and clarification of efficacious dosing [9,11,12].
As early as 1967, Robbins [5] reported a two- fold improvement in the quality of pediatric dental sedations when Chloral Hydrate (CH) was combined with an anti-emetic to enable difficult apprehensive young children to accept invasive treatment. The addition of promethazine, an antiemetic with anthistaminic and sedative qualities, enabled use of half the CH sedative dosing, reduced the incidence of somnolence, and virtually eliminated nausea and emesis. This study was predicated on the concept of “balanced medication” a conceptualization of Lampshire (1959) [10] that combinations might best offset the downside (in the case of CH’s GI upsetting nature) of the primary agent.
In one of the few pediatric dental textbook recommendations available, Trapp (1982) [6] reported significant failure of the hypnotic dosage of CH (50 mg/kg) to produce satisfactory or predictable CH dosing for challenging young children. His textbook recommendation for dosing of CH alone extended dosing from 50 to 70 mg/kg despite concerns of protracted somnolence and increased potential for induction of deeper planes of sedation.
Studies reported by Houpt et al. [13,14] and other researchers, [15-18] explored comparisons of 50 vs 75 mg/ kg CH with antiemetic, revealing increased incidence of somnolence and emesis, and unpredictable levels of sedation. Replicating Houpt’s methodologies these studies included limited behavioral selection criteria, confounded use of fixed 50% adjunctive nitrous oxide, and mandatory physical restraint for all subjects. Based on this repetitious form of concatenated authority, conclusions regarding efficacy of CH were at best compromised due to the perplexing inclusion of confounding variables that likely contributed to subject anger/ frustration from being bound coupled with nausea/emesis from excessive nitrous oxide concentrations.
Extrapolating from the concept of balanced sedation offered by Lampshire [10], Nathan & West [11] in a retrospective study of 135 cases, first reported the effect of the addition of narcotic (meperidine) to the sedative combination of CH and anti-emetic. Comparisons were made of 50 and 70 mg/kg CH, with antiemetic, and the addition of 1-2 mg/kg meperidine, with and without variable concentrations of nitrous oxide for difficult subjects 4-6 years of age. The addition of meperidine providing analgesia enabled significantly improved sedation efficacy and lower dosing of the chloral hydrate. It was concluded that higher dosing of CH produced prolonged somnolence and therefore was found unproductive if not inappropriate. Similarly, emesis occurred significantly less. Replication in a prospective manner of this study was conducted Hasty et al. [12] Comparing 50 vs 75 mg/kg CH with and without meperidine, Hasty et al reported significantly improved efficacy, predictability, and safety when narcotic was included, consistent with the findings of Nathan & West [11].
These latter findings served to identify this “triple combination” as the regimen of choice for the next two decades on a national level, taught and advocated at most advanced training programs in pediatric dentistry in the U.S. for managing moderately to severely apprehensive young children under age 6 (or 60 pounds) when long duration of action was required [3,11,12,18-20,22-23]. This regimen is reported to be in continued use.
- Review Article
- Abstract
- Introduction
- Background
- Armamentarium of Sedative Agents and Combinations for the Pediatric Patient
- Limitations of the Oral Route and Available Agents
- Alternatives to Chloral Hydrate
- Retrospective Data in support of the continued merit in using CH combinations and other commonly employed agents and combinations
- Summary and Final Remarks
- References
Armamentarium of Sedative Agents and Combinations for the Pediatric Patient
In addition to CH combinations, the list of available agents for the pediatric patient includes benzodiazepine (diazepam, midazolam, lorazepam), antihistamines, (promethazine, hydroxyzine, Diphenhydramine), analgesics (acetaminophen, meperidine, morphine, sublimaze); an adjunctive inhalation agent such as nitrous oxide is often used to supplement the oral and nasal route of administration with the inherent advantages of titration characterized by rapid onset and elimination.
While parenteral administration of sedative agents, recognized for enhanced potency and predictability exists, intravenous and intramuscular routes are believed of limited practicality for the young pediatric patient or viable from a liability insurance perspective. As such, discussion will be limited to the use of orally administered agents and dosing. Recognition of the disadvantages of the oral route of administration is well known. Despite the below described limitations of the oral route, it nevertheless remains the most commonly used approach by pediatric dentists for their clientele.
- Review Article
- Abstract
- Introduction
- Background
- Armamentarium of Sedative Agents and Combinations for the Pediatric Patient
- Limitations of the Oral Route and Available Agents
- Alternatives to Chloral Hydrate
- Retrospective Data in support of the continued merit in using CH combinations and other commonly employed agents and combinations
- Summary and Final Remarks
- References
Limitations of the Oral Route and Available Agents
- Variable and unpredictable absorption from GI tract
- Dependence on patient compliance for ingestion
- First pass metabolism
- Ineffectiveness of gastric lavage in the event of over dosage
- Diminished GI motility in the presence of anxiety
- Prolonged latency required
- Unpredictable efficacy and prolonged duration of action
- Limited availability of reversal agents
- Review Article
- Abstract
- Introduction
- Background
- Armamentarium of Sedative Agents and Combinations for the Pediatric Patient
- Limitations of the Oral Route and Available Agents
- Alternatives to Chloral Hydrate
- Retrospective Data in support of the continued merit in using CH combinations and other commonly employed agents and combinations
- Summary and Final Remarks
- References
Alternatives to Chloral Hydrate
Use of Midazolam for the Pediatric Patient:
The manufacturer’s maximum single dosing recommendation for CH is 1000 mg. Morbidity and mortalities have been reported when dosing has exceeded 1500 mg. Subjects weighing greater than 25 kg exceed the MRD when hypnotic dosing is selected. Either dosing in the sedative range (25 mg/kg), or alternative agents need be considered. Midazolam has emerged as a popular alternative to CH, and as described below, possesses both distinct advantages and limitations.
With the discontinuation of the oral elixir formulation of CH, Midazolam (administered in an oral preparation, or intranasally using its injectable formulation) currently is the most frequently used sedative in pediatric dentistry [23-25]. Unlike CH, this benzodiazepine carries a distinct advantage of having an available reversal agent; while possessing capacity for more rapid onset, its distinct disadvantages overshadow its positive features manifesting variable and unpredictable efficacy and short if not ultra short duration of action (unlike CH) which renders it of limited value when visits of longer duration are needed.
In an effort to enhance sedation efficacy and predictability and expand the working time of midazolam, Nathan & Vargas [24] suggested the addition of meperidine. They reported significantly improved quality of sedations using 0.7 and 1.0 mg/kg midazolam in combination with meperidine compared to 0.5 and 0.7mg/kg midazolam alone. When combined with 1-2 mg/kg narcotic, sedations proved more effective and virtually no incidence of somnolence occurred. Working times lengthened from 10 to 40 minutes to enable longer cooperation and more extensive treatment to be accomplished.
Over the past five years, surveys of program directors [3,4] of advanced pediatric dental training programs have identified trends which have substantially curbed or withdrawn the use of agents such as chloral hydrate and meperidine. Several factors contribute to the abandonment of these agents. Background and training of many with minimal experience with these agents using therapeutic dosage ranges appears to have become the norm rather than exception. Generalized acceptance to make use of sub- therapeutic dosing to avoid even remote possibilities of adverse reactions, at the expense of necessitating greater need for physical restraint or use of general anesthesia likely account for these trends. Incidents resulting in high profile media attention from overdosing, poor clinician judgment, use of local anesthetic grossly in excess of maximum recommended dosing, have served to support trending in the direction of using belowtherapeutic sedative dosing with enhanced willingness to accept the use of aversive measures to accomplish treatment.
Diazepam has been somewhat useful as an alternative to CH owing to its wide range of safety, pleasant taste, and relatively rapid absorption when administered orally. [6,8,21] Its duration of action exceed midazolam one side, while its active metabolites and prolonged action offer disadvantages to its use in older subjects.
Recent study has begun to explore parental attitudes and preferences for sedation over restraint [27,28]. Parental preferences appear in the direction that the use of sedation is currently on an increase. Parents acknowledge clear preference that restraint be avoided wherever possible. Some have expressed disappointment when asked to pay sedation fees in lieu of ineffective sedation and enhanced need for deploying restraints to manage their child. The fact of the matter remains that wide variation amongst clinicians exists with respect to sedation training and experience.
Clinicians less skilled in selecting and safely using therapeutic dosing to permit avoidance of aversive methods find themselves with greater need to resort to general anesthesia [3]. Experienced clinicians, on the other hand, proficient and competent in their ability to make prudent dosing decisions, able to intercept, recognize, and manage a developing untoward reaction in fully equipped facilities, do not find this problematic. Literally thousands of safe and effective pediatric sedations occur on a daily basis. Conversely, under circumstances where non-compliance following existing safety guidelines occurs, inadequate patient monitoring falls short of patient need, illequipped facilities and inadequately trained support staff exists, this has potential to become highly problematic.
Illustration of these deficiencies are notably apparent from several papers that have emerged in the last decade describing the most frequently encountered etiologies of sedation mishaps. [29-34]. Summary of causes of mishaps include:
- Over dosage and gross unfamiliarity with agents and potential drug interactions;
- Failures to adequately assess patient risk factors and tolerance;
- Use of local anesthetic in gross excess of the maximum recommended dosing;
- Inadequate patient monitoring for the needs of the patient and level of sedation induced intra-operatively and post-operatively;
- Failure to satisfy discharge criteria;
- Inadequately equipped facilities, emergency supplies, and trained support staff; and
- Lack of preparedness to recognize a developing problem and/or competency in managing a medical emergency associated with sedation use.
- Review Article
- Abstract
- Introduction
- Background
- Armamentarium of Sedative Agents and Combinations for the Pediatric Patient
- Limitations of the Oral Route and Available Agents
- Alternatives to Chloral Hydrate
- Retrospective Data in support of the continued merit in using CH combinations and other commonly employed agents and combinations
- Summary and Final Remarks
- References
Retrospective Data in support of the continued merit in using CH combinations and other commonly employed agents and combinations
The below data in (Tables 1-3) is provided as preliminary retrospective study of the relative safety and efficacy of Chloral hydrate in combination with hydroxyzine and meperidine used in a clinical setting over the past 35 years of this author. Data is included for alternative agents used in combination for comparisons of safety and efficacy. The study serves to review sedation logs of patients receiving various dosing with institutional review board approval from the University of Alabama, Birmingham.
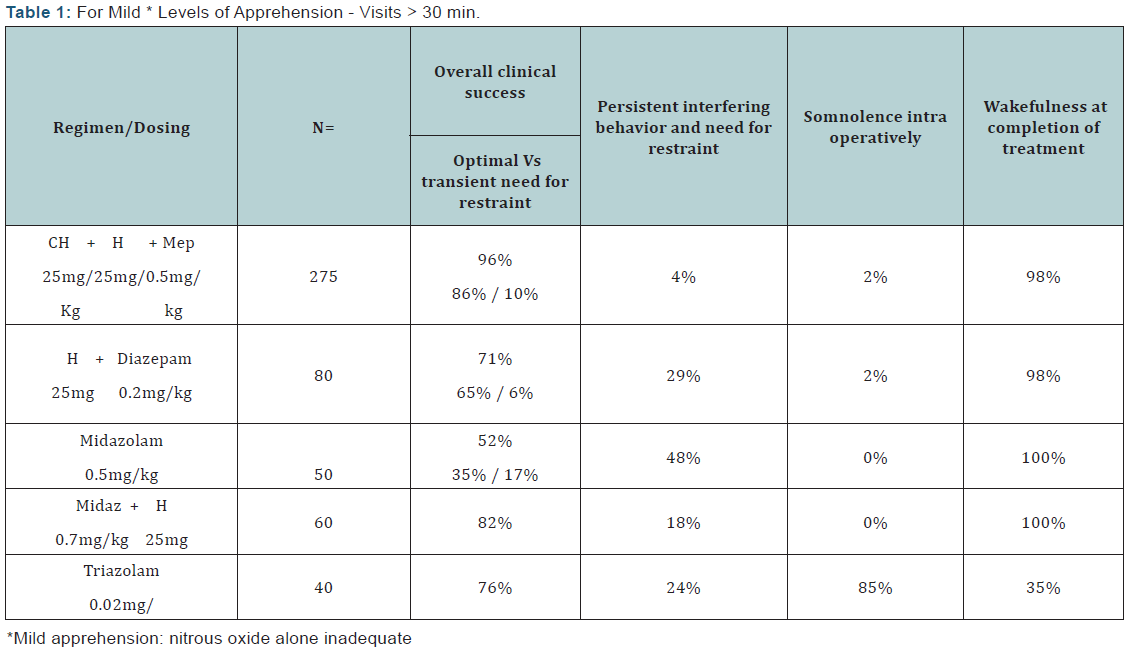
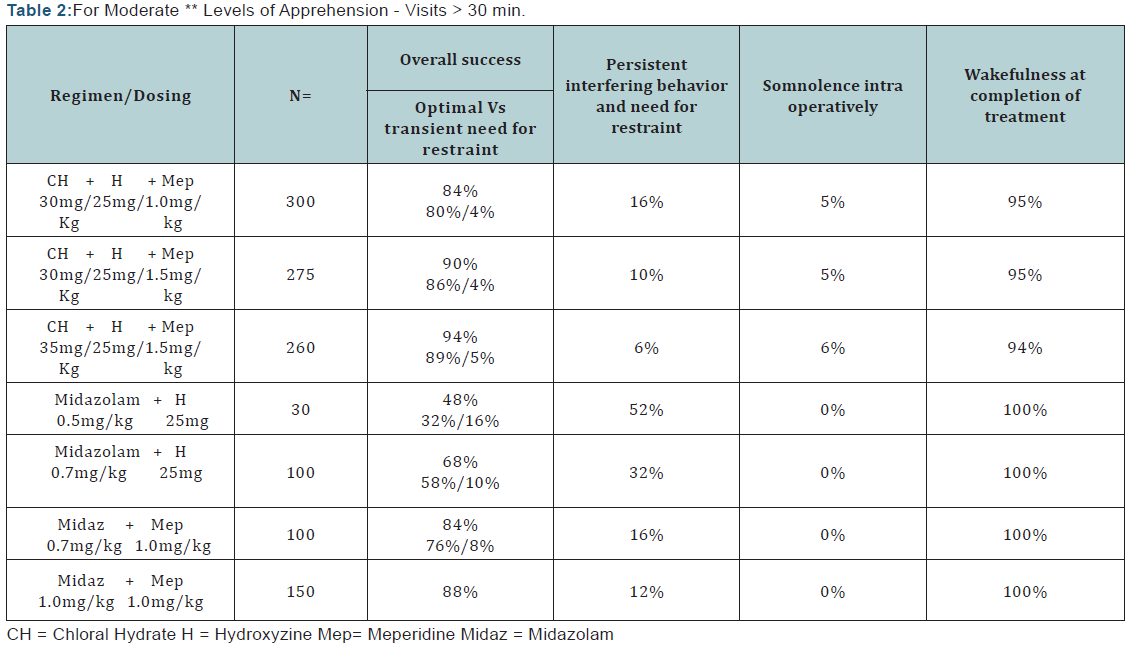
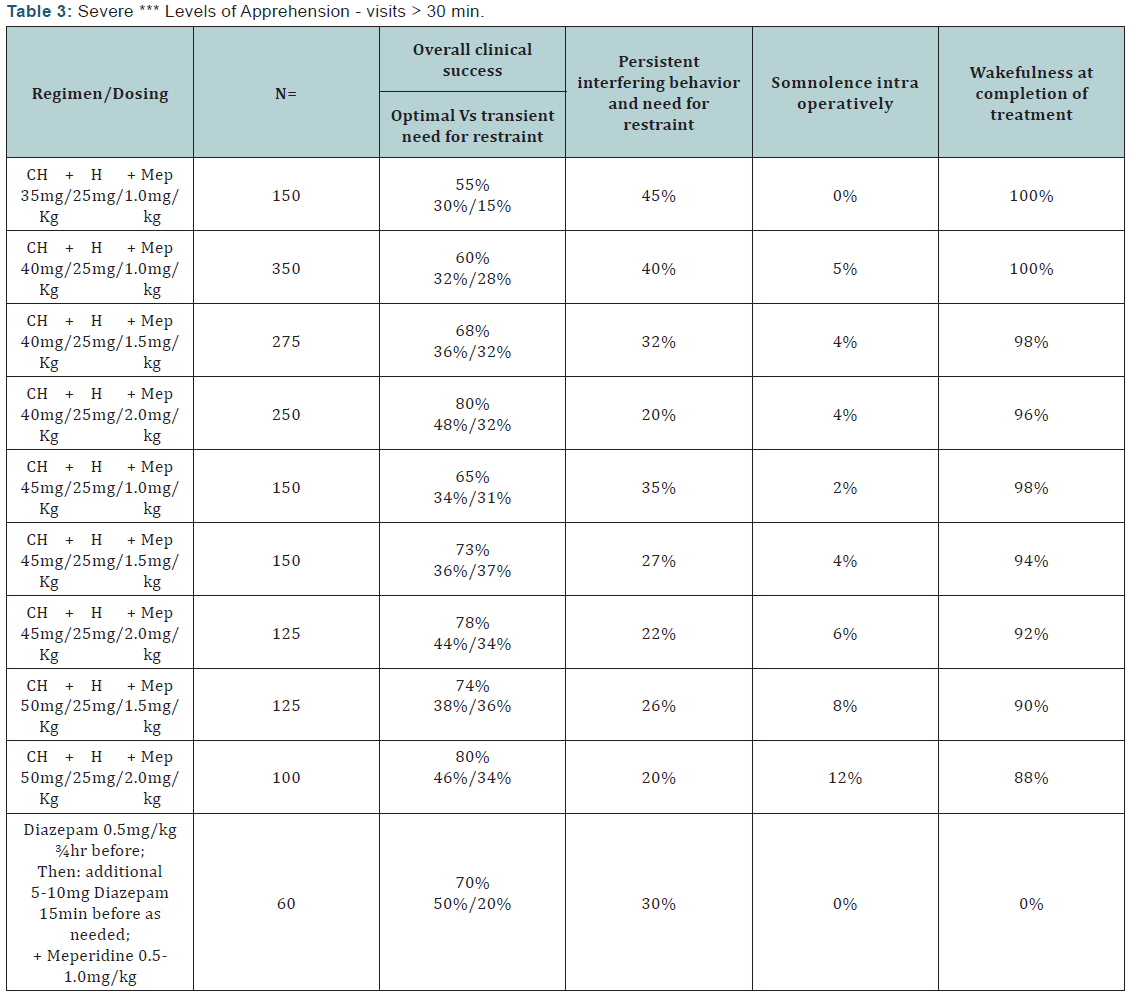
Data illustrated in the above tables demonstrate the relative success rates obtained from various regimens defined as theoverall ability to complete treatment objectives either without need for physical restraint of interfering patient movement vs transient need for restraint for varying levels of apprehension and uncooperative behaviors. Needing transient application of restraint is not considered as a major detraction from success in contrast to the persistent need for restraint. Induction of somnolence during and following completion of treatment is suggestive of inadvertent induction of deeper planes of sedation than optimally desired.
Operator skill in both differentiation of the depth of sedation achieved, i.e. moderate vs deep sedation and the ability to manage patient airway and ventilatory status is essential for safe use of these regimens.
- Review Article
- Abstract
- Introduction
- Background
- Armamentarium of Sedative Agents and Combinations for the Pediatric Patient
- Limitations of the Oral Route and Available Agents
- Alternatives to Chloral Hydrate
- Retrospective Data in support of the continued merit in using CH combinations and other commonly employed agents and combinations
- Summary and Final Remarks
- References
Summary and Final Remarks
Much remains to be learned from future retrospective and prospective study of sedative modalities. Research methodologies need to define patient selection criteria, identify valid measures of the impact of various agents and dosing on child responses from behavioral and physiological parameters. Additional agents need be studied, capacities for reversal expanded, and assurances that practitioner competency and compliance with contemporary safety guidelines be enacted. Innovative measures to enhance ingestion through compounding formulation can be expected to facilitate palatability, absorption, and more predictable patient responses. It is noted that the data presented above is preliminary in nature; despite such, some general conclusions seem warranted.
What constitutes clinical success remains subjective and will vary based upon expectations of clinician and parent alike. Acceptability of restraint as perceived by parent and clinician will also differ. Percentages of success, defined as the ability to maintain light to moderate levels of sedation, in the range of 70-80 percent where either no restraint or transient need might reasonably be considered desirable. Greater than 80% success as found with combinations of CH, antiemetic, and narcotic might be considered optimal under circumstances where consciousness and ease of arousal are maintained. Lastly, under circumstances where anxiety and resistance levels prove profound and refractory to moderate sedation levels of depression, abandonment of sedation modalities for the use of unconscious techniques, administered in surgical center and hospital centers would seem appropriate.
- Review Article
- Abstract
- Introduction
- Background
- Armamentarium of Sedative Agents and Combinations for the Pediatric Patient
- Limitations of the Oral Route and Available Agents
- Alternatives to Chloral Hydrate
- Retrospective Data in support of the continued merit in using CH combinations and other commonly employed agents and combinations
- Summary and Final Remarks
- References
References
- Nathan JE (2015) The Subtleties and Nuances of Pediatric Sedation: A Disappearing Art for Managing the Apprehensive Child Patient. Journal of Otolaryngology and Rhinology 1: 1.
- Nathan JE (2015) The Direction of Pediatric Sedation: A Contemporary and Historical Look at its Science, Art, Strengths, and Shortcomings. Int J of Otolaryngology 2(1): 8-15.
- Wilson S, Nathan JE (2011) A Survey Study in Sedation Training in Advanced Pediatric Dental Residencies. Ped Dent 33(4): 353-360.
- Weinstein P, Nathan JE (1988) Management of the Dentally-Phobic Child. Dent Cl NA 32(4): 667-692.
- Robbins MB (1967) Chloral hydrate and promethazine as premedicants for the apprehensive child. J Dent Child 34: 327-331.
- Trapp L Pharmacologic management of pain and anxiety, In: Pediatric Dentistry, Stewart, Barber, Troutman, and Wei, eds, St.Louis: Mosby, 1982, p 810-832.
- Nathan J (1987) Management of the refractory young child with chloral hydrate: dosage selection. J Dent Child 54(2): 93-100.
- Nathan JE (1995) Managing behavior of pre-cooperative children. Dental Cl NA 39: 789-816.
- Wilson S, Houpt MI Project USAP (2016) Use of Sedative Agents in pediatric dentistry- a 25 year follow-up study. Ped Dent 38(2): 116- 121.
- Lampshire ED (1959) Balanced medication. J Dent Child 26: 25-31.
- Nathan JE, West MS (1987) Comparison of chloral hydrate-hydroxyzine with and without meperidine for management of the difficult pediatric dental patient. J Dent Child 54(6): 437-444.
- Hasty MF, Vann WmF, Dilley DC, Anderson JA (1991) Conscious sedation of pediatric dental patients: An investigation of chloral hydrate-hydroxyzine with and without meperidine. Ped Dent 13(1): 10-19.
- Houpt MI, Koenigsberg S, Weiss N (1984) A comparison of chloral hydrate with and without promethazine in the premedication of young children. Ped Dent 6: 176.
- Houpt MI, Sheskin RB (1985) Assessing chloral hydrate dosage for young children. J Dent Child 52(5): 364-369.
- Moore PA, Mickey E, Hargreaves J, Needleman HL (1984) Sedation in pediatric dentistry: a practical assessment procedure. JADA 109(4): 564-569.
- Moody EH, Mourino AP (1986) The therapeutic effectiveness of nitrous oxide and chloral hydrate administered orally, rectally and combined with hydroxyzine. J Dent Child 53(6): 425-429.
- Meyer ML, Mourino AP, Farrington FH (1990) Comparison of Triazolam to chloral hydrate, hydroxyzine combinations in the sedation of pediatric dental patients. Ped Dent 12(5): 283-287.
- Poorman T, Farrington FH, Mourino AP (1990) Comparison of chloral hydrate-hydroxyzine combination with and without meperidine in the sedation of pediatric dental patients. Ped Dent 12: 288-291.
- Wilson S (1992) Chloral hydrate and its effects on multiple physiologic parameters in children: a dose response study, Ped Dent 14(3): 171- 177.
- Needleman HL, Joshi A, Griffith DG (1995) Conscious sedation of pediatric dental patients using chloral hydrate, hydroxyzine, and nitrous oxide – a retrospective study of 382 sedations. Ped Dent 17(7): 424-431.
- Nathan JE (2003) Pediatric Dental Sedation: When non-pharmacologic approaches prove inadequate or inappropriate. J Pediatric Dental Care 9: 8-9.
- Vargas KG, Nathan JE, Kupietsky A (2007) Use of Restraint and management style as parameters for determining sedation success: a survey of pediatric dentists. Ped Dent 29(3): 220-227.
- Sheroan MM, Dilley DC, Lucas WJ, Vann WmF (2006) A prospective study of two sedation regimens in children: chloral hydrate-hydroxyzine and meperidine vs midazolam, meperidine, and hydroxyzine. Anesth Progress 53(3): 83-90.
- Nathan JE, Vargas (2002) KG Oral Midazolam with and without meperidine for management of difficult young pediatric dental patients: a retrospective study. Ped Dent 24: 129-138.
- McCormack L, Chen JW, Trapp L, Job A (2014) A comparison of sedation related events for two multi-agent sedation regimens in pediatric dental patients. Ped Dent 36: 302-308.
- Peretz, B Kharouba, J, Somri, M (2014) A comparison of two different dosages of midazolam, Ped Dent 36: 228-232.
- Patel, M, McTigue, DJ, Thikkurissy,S, Fields, HW (2016) Parental Attitudes toward advanced behavior guidance in pediatric dentistry, Ped Dent 38(1): 30-36.
- White J, Wells M (2016) A Questionnaire of parental perceptions of conscious sedation in pediatric dentistry. Ped Dent 38(2): 116-121.
- ACote CJ (1994) Sedation for the pediatric patient: a review. Pediatric Cl NA 41(1): 31-58.
- Persad J, Palmisano P, Nichols M (1999) Chloral hydrate: The Good and the Bad. Ped Emerg Care 15(6): 432-435.
- Cote CJ, Karl HW (2000) Adverse Sedation Events in Pediatrics: Analysis of medications used in sedation. Pediatrics 106(4): 633-644.
- Dionne RA, Yagiela JA, Cote CJ (2006) Balancing efficacy and safety in the use of oral sedation in dental out-patients. J Am Dent Assn137(4):502-513.
- Cravero JP, Blike GT (2006) Incidence and nature of adverse events during pediatric sedation/anesthesia for procedures outside the operating room, Report from the Pediatric Sedation Research Consortium. Pediatrics 118(3): 1087-1096.
- Nathan JE (2016) Morbidity and Mortality involving pediatric sedation: Non-Compliance following Sedation Guidelines. J of Surgery May.







