Comparing The Correlation of Determined Dental Age with Chronological Age in Orthodontic Patients Between 2018-2022 Among 5-16 Year Old Patients
Sahar Haghighat*
Department of I.M. Sechenov First Moscow State Medical University (MSMU), Moscow, Russia
Submission: January 23, 2023;Published: May 02, 2023
*Corresponding author: Sahar Haghighat, Department of I.M. Sechenov First Moscow State Medical University (MSMU), Moscow, Russia
How to cite this article: Sahar H. Comparing The Correlation of Determined Dental Age with Chronological Age in Orthodontic Patients Between 2018-2022 Among 5-16 Year Old Patients. JOJ scin. 2023; 3(3): 555615. DOI: 10.19080/JOJS.2023.03.555615
Abstract
Dental age assessment is very useful in the daily work of pediatric dentists and orthodontists. The final lack of correlation between dental age, skeletal maturity and chronological age could influence further treatment methods regarding when to apply them. The present study was planned to assess and compare chronological age with dental age (Demirjian’s method and Willem’s method) and skeletal age (Fishman’s method). Materials and Methods: The present study was done on a sample of 200 children in Iran. (Sistan and Baluchistan) the age group of 5–16 years. It can be concluded from the present study that the dental age estimation evaluated by the digital OPG by both the methods, that is, Demirjian’s method and Willem’s method, has shown high accuracy when applied to the children of Faridabad. Skeletal maturation evaluated by Fishman’s method using hand-wrist radiographs was found to overestimate the age when compared to chronological age in both sexes.
Keywords: Orthodontic; Age Determination by Teeth; Willem’s method; Dental age; Fishman’s method
Abbreviations: CVM: Cervical Vertebra Maturation; WM: Willem’s Method; OPG: Orthopantomogram; SMIs: Skeletal Maturational Indicators; DM: Demirjian’s Technique
Introduction
The diagnosis, planning, objectives, and final result of orthodontic treatment can all be significantly influenced by determining the adolescent child’s level of development. Both pedodontics and orthodontic daily practice depend on knowing when a youngster is experiencing active growth [1]. The idea of biological or physiological age was first developed due to significant differences in developmental trajectory among kids of the same chronological age [2].
The development of the craniofacial complex and height are clearly correlated. Because morphological indications may only be used after the serial recording of height, height has little significance in the instant clinical judgment of a child’s maturity stage. Radiographs of the hand, wrist, and cervical vertebrae are frequently used in orthodontics to evaluate skeletal development [3]. According to Lamparski, there is a significant correlation between hand-wrist maturity and cervical vertebral maturity [4]. In order to avoid needless radiation exposure, our study examines the cervical vertebrae’s maturity. Based on the morphology of the second, third, and fourth vertebrae on a lateral cephalogram, Hassel and Farman proposed six stages of categorized formation of cervical vertebrae [5]. Dental maturity, which may be assessed using two different event approaches, is another factor in assessing adolescent development. The first is based on the tooth under examination’s eruption age. The “dental eruption age” could be applied to this period. The second method, also known as Demirjian’s method, enables us to examine the degree of lower first bicuspid mineralization on the panoramic radiograph. First lower premolar development starts between the ages of 21 and 24 months and lasts until the age of 12 to 13 years.
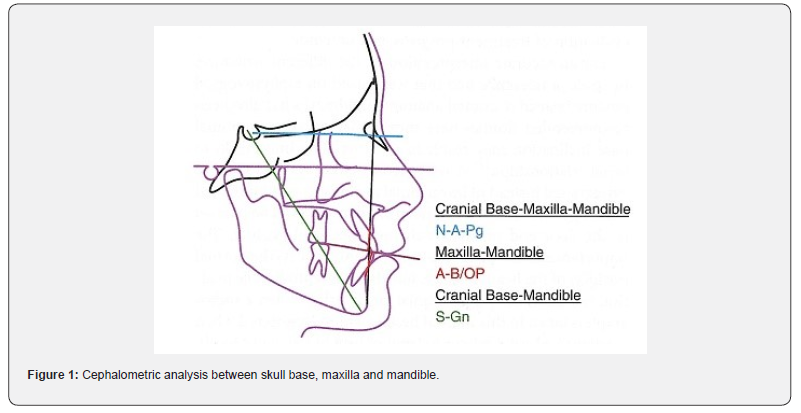
Skeletal maturation describes the stage of ossification development in bones. Size and maturation can differ independently of one another. Biological maturity is determined by radiographic evaluation of one or more body regions, and skeletal maturation is well understood and often employed for this purpose. A new investigation used hand-wrist radiographs to evaluate the stages of skeletal maturity. The cervical vertebra maturation (CVM) approach, which was recently established, reduces the need for extra radiographic exposure while measuring growth and allocating skeletal age (Figure 1) [6-10].
As forensic dentistry is a relatively new discipline, there are few published studies on the various techniques for estimating a child’s age in Iran, Sistan. As a result, an effort has been undertaken to evaluate and compare the chronological, dental, and skeletal ages of Iranian children (Sistan). Additionally, the goal of the current study was to evaluate two approaches to estimating dental age (Demirjian’s technique [DM] and Willem’s method [WM]) and one approach to estimating skeletal age (Fishman’s method) with respect to chronological age [11].
Materials and Methods
The study group comprised 200 children, of which 100 were males and 100 females, in the age group 6–16 years who visited the Department of Paediatric and Preventive Dentistry and the Department of Orthodontics, Iranian College of Dental Sciences and Research, Sistan and Baluchistan.
Inclusion standards
i. Absence of any past or existing sickness.
ii. No history of an illness that would have affected the existence or growth of mandibular teeth, either medically or surgically.
iii. Except for the third tooth, the individual had a fully developed mandibular permanent dentition (both clinically and radio graphically).
iv. An orthopantomogram (OPG) was recommended as part of the patient’s orthodontic treatment since they needed it.
v. The parents’ informed written consent had been acquired.
Exclusion standards
i. Severely decayed tooth or teeth are present in the lower left quadrant.
ii. children who have chronic illnesses or who need longterm drugs
iii. Any associated skeletal and dental anomaly.
iv. Either extensive pathology or hypodontia.
v. Teeth agenesis.
vi. Sickness that could impact how teeth erupt in the body.
Skeletal age was calculated from digital hand-wrist radiograph by the following method:
Fishman’s method [12]: The left-hand-wrist radiograph of the subject was taken to observe the six anatomical sites located on the thumb (adductor sesamoid), third finger (proximal, middle, and distal phalanx), fifth finger (middle phalanx), and the radius. After that, eleven discrete adolescent skeletal maturational indicators (SMIs) covering the entire period of adolescent development were observed on these six anatomical sites. Now, the stages of bone maturation were observed starting with ossification of adductor sesamoid of thumb to note the SMIs. If the ossification had not taken place, then epiphyseal widening on selected phalanges was checked. But if the ossification had taken place, then fusion of distal phalanx of the third finger was checked. If the fusion had not taken place, then capping of selected epiphyses over their diaphysis was checked. But if the fusion had taken place, then further fusion of selected epiphyses and diaphysis and the fusion of radius were continued for assessment.
Sequence of four ossification stages are as follows:
i. Epiphyseal widening on selected phalanges.
ii. Ossification of adductor sesamoid of thumb.
iii. “Capping” of selected epiphyses over their diaphysis.
iv. Fusion of selected epiphyses and diaphysis.
Once all the stages of maturation had been observed in the hand-wrist radiograph and accordingly SMI numbers had been noted, the final SMI number recorded was checked for the assessment of age from the given table by Fishman for boys and girls individually. Paired t-test was used to analyze the differences between the estimated dental age (DM and WM), chronological age, and skeletal age (Fishman’s method) at a significance level of P < 0.01. Age estimation was done in a standardized way by second evaluator on 25 OPGs and kappa value was determined to assess the inter-examiner reliability.
Results and Discussion
200 kids between the ages of 5 and 16 made up the study group in the current study. The age ranges of 9–10–11 years are crucial because they are usually employed as a clinical window for early orthodontic therapy focused at growth modification. Orthodontists evaluate children for starting therapy during this age group even when they are not already receiving active treatment, therefore it is crucial to understand the distinctions in skeletal age and chronologic age in typically developing children in the 9-, 10-, and 11-year age groups. When treating various types of malocclusions in connection to maxillofacial growth, pedodontics and orthodontists are especially interested in dental age assessment. Since genes rather than environmental variables influence how quickly teeth calcify, dental age assessment may be more accurate than other age estimation techniques. Different techniques for determining dental maturity reveal different levels of development (Table 1).
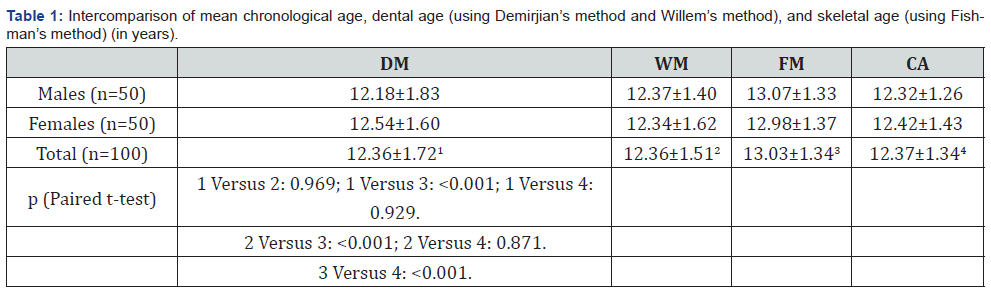
DM: Demirjian’s method; WM: Willem’s method; FM: Fishman’s method; CA: Chronological age
The most popular techniques are based on how OPGs depict the stages of tooth development. Some of the techniques used to determine dental age are DM, Nolla’s, Haavikko’s, WM, Kvaal’s, and Cameriere’s. [13,14]. Radiographs are used to evaluate dental development, and several radiograph types are employed in dental age evaluations. The majority of authors use panoramic radiographs because they are easily accessible and allow for the visualization of all teeth [15-18]. Additionally, OPG requires less radiation exposure than full mouth radiography and is simpler to perform on young or anxious children. It might be challenging to take intraoral radiographs without introducing image distortion, which makes age assessment results less accurate. As a result, two alternative methods—DM and WM—that employ the panoramic radiographic approach were used in this investigation to determine the dental age using panoramic radiographs. Although the left side of the jaw seems to be 3–10% larger on the panoramic radiographs [19], this is not a significant flaw because the Demirjian’s system and WM base their ratings on shape criteria and relative values rather than on absolute length.
The Fishman’s technique provides a methodical and generally easy way to assess maturity. The method only makes use of 11 anatomical locations, all of which show constancy in the timing of ossification. These sites are on the phalanges, the adductor sesamoid, and the radius. Additionally, as irregularity in the onset order of ossification occurs more commonly in the carpals than in the metacarpal or phalangeal epiphysis, it is advantageous to omit the carpals from the system.
In addition, it can be utilized without the presence of any Atlas More Details and thus can be easily used in clinics [20,21]. In the present study, Fishman’s method was the only method that showed significant differences with other pairs of mean age and also the low values of Pearson’s correlation. The overestimation of age by Fishman’s method in the present study is in contrast to the study done by [21] which found it to be quite accurate in Iranian children. The limitation of the present study was that the sample size was relatively smaller. It could be recommended that larger sample size should be used to establish better accuracy in age determination for children of Iran (Sistan city of Iran).
A larger sample size would have reduced the differences in the estimation of the various biological ages. Consideration of the cultural habits, dwelling conditions, maternal influence, environmental factors, and genetic endowment was beyond the scope of the study. The methods used for dental age assessment were based on foreign population standards. Although various methods of age estimation have been used, the applicability can vary due to the wide ethnic differences between the populations. It is therefore mandatory that maturity standards should be based on the same population for which they are going to be used. Ethnic differences and racial variations suggest that new criteria and new grading scores should be formulated and published exclusively for that particular population.
Conclusion
From the current study, it can be inferred that the dental age estimation assessed by the digital OPG by both approaches, DM and WM, has demonstrated great accuracy when applied to Iranian youngsters (Sistan. Iran). When compared to chronological age in both sexes, skeletal maturation assessed by the digital hand-wrist radiograph using Fishman’s approach was found to be overstated.
Acknowledgment
This study was conducted as a case study in Russia (2021- 2022) and was presented at the International Conference on Dentistry and Medical Sciences Kuala Lumpur, Malaysia 2022.
References
- Ghaeminia H, Nienhuijs ME, Toedtling V, Perry J, Tummers M, et al. (2020) Surgical removal versus retention for the management of asymptomatic disease‐free impacted wisdom teeth. Cochrane Database of Systematic Reviews 4: 5(5).
- Dodson TB, Susarla SM (2010) Impacted wisdom teeth. BMJ clinical evidence.
- Eroglu CN, Durmus E, Kiresi D (2014) Effect of low-dose dexketoprofen trometamol and paracetamol on postoperative complications after impacted third molar surgery on healthy volunteers: A pilot study. Medicina Oral, Patología Oral y Cirugía Bucal 19(6): e622.
- Dodson TB, Susarla SM (2014) Impacted wisdom teeth. BMJ Clinical Evidence.
- Farhadi F, Eslami H, Majidi A, Fakhrzadeh V, Ghanizadeh M, et al. (2017) Evaluation of adjunctive effect of low-level laser Therapy on pain, swelling and trismus after surgical removal of impacted lower third molar: A double blind randomized clinical trial. Laser therapy 26(3): 181-187.
- Jaroń A, Preuss O, Grzywacz E, Trybek G (2021) The impact of using kinesio tape on non-infectious complications after impacted mandibular third molar surgery. International Journal of Environmental Research and Public Health 18(2): 399.
- Mohammed IA, Deleme ZH (2020) Kinesiology Tape in Comparison with Submucosal Injection of Dexamethasone in Reducing Pain and Swelling After Surgical Removal of Impacted Lower Wisdom Teeth. Al-Rafidain Dental Journal 20(1): 18-24.
- Qassab AHM, Kumar N (2020) Effects of hyaluronic acid gel application in reduction of post-surgical complications after lower wisdom teeth removal–a prospective study. Plant Archives 20(1): 2796-800.
- Liu S, You Z, Ma C, Wang Y, Zhao H (2018) Effectiveness of drainage in mandibular third molar surgery: A systematic review and meta-analysis. Journal of Oral and Maxillofacial Surgery 76(8): 1640-1650.
- Zhu J, Yuan X, Yan L, Li T, Guang M (2020) Comparison of postoperative outcomes between envelope and triangular flaps after mandibular third molar surgery: a systematic review and meta-analysis. Journal of Oral and Maxillofacial Surgery 78(4): 515-527.
- Badiee M, Jafari N, Fatemi S, Ameli N, Kasraei S (2020) Comparison of the effects of toothpastes containing nanohydroxyapatite and fluoride on white spot lesions in orthodontic patients: A randomized clinical trial. Dental Research Journal 17(5): 354-359.
- Yousef N, Niloufar M, Elena P (2019) Antipathogenic effects of emulsion and nanoemulsion of cinnamon essential oil against Rhizopus rot and grey mold on strawberry fruits. Foods and Raw materials 7(1): 210-6.
- Duarte-Rodrigues L, Miranda EFP, Souza TO, de Paiva HN, Falci SGM (2018) Third molar removal and its impact on quality of life: systematic review and meta-analysis. Quality of Life Research 27(10): 2477-2489.
- Cervino G, Cicciù M, Biondi A, Bocchieri S, Herford AS et al. (2019) Antibiotic prophylaxis on third molar extraction: Systematic review of recent data. Antibiotics 8(2): 53.
- Hounsome J, Pilkington G, Mahon J, Boland A, Beale S et al. (2020) Prophylactic removal of impacted mandibular third molars: a systematic review and economic evaluation. Health Technology Assessment (Winchester, England) 24(30): 1-116.
- Leung YY (2019) Management and prevention of third molar surgery-related trigeminal nerve injury: time for a rethink. Journal of the Korean Association of Oral and Maxillofacial Surgeons 45(5): 233-240.
- De Poortere A, Van Der Cruyssen F, Politis C (2021) The benefit of surgical management in post-traumatic trigeminal neuropathy: a retrospective analysis. International Journal of Oral and Maxillofacial Surgery 50(1): 132-138.
- Naserzadeh Y, Mahmoudi N, Nafchi AM, Hashim AF, Ahmed FK (2022) Antipathogenic effects of plant essential oil nanoemulsions. Bio-Based Nanoemulsions for Agri-Food Applications: Elsevier pp: 245-57.
- Naserzadeh Y, Mahmoudi N (2018) Chelating effect of black tea extract compared to citric acid in the process of the oxidation of sunflower, canola, olive, and tallow oils. International Journal of Agricultural and Biosystems Engineering 12(5): 5.
- Bouloux GF, Steed MB, Perciaccante VJ (2007) Complications of third molar surgery. Oral and Maxillofacial Surgery Clinics 19(1): 117-128.
- Chiapasco M, De Cicco L, Marrone G (1993) Side effects and complications associated with third molar surgery. Oral surgery, oral medicine, oral pathology 76(4): 412-420.