Introduction
Obesity is a chronic condition characterized by excessive accumulation of body fat, which compromises the physical, emotional, and social health of individuals [1]. Considered one of the main public health problems in the contemporary world, its prevalence has increased significantly in recent decades, affecting different age groups and socioeconomic groups [2,3]. In addition to its association with comorbidities such as type 2 diabetes, high blood pressure, and cardiovascular disease, obesity has direct implications for psychological well-being and quality of life [4].
Epidemiological projections indicate that, by 2025, approximately 700 million adults globally may be affected by obesity. Notably, Brazil experienced a significant increase in the prevalence of obesity, with a growth of approximately 72% between 2006 and 2019, rising from 11.8% to 20.3% [5,6]. These data emphasize the urgency of implementing preventive measures and effective interventions to address this growing epidemic and mitigate its adverse implications for mental health. Mental health is often affected in individuals with obesity, although obesity is not categorized as a psychological disorder per se [7,8]. However, several emotional factors are closely related to the disease, including anxiety, depression, and stress, which play significant roles in both the development of obesity and its treatment [9,10]. In addition to promoting a healthy diet, it is crucial to pay attention to the mental health of patients undergoing treatment, as this is fundamental to therapeutic progress [11]. Indeed, mental health plays a central role in this process, assisting psychology professionals in understanding patients’ individual preferences and offering appropriate support [12].
Psychology plays a crucial role in helping individuals understand the relationship between their mental health and obesity, seeking strategies that promote healthier habits and maintain quality of life. Therefore, the use of psychological assessments is essential, both for data collection and for a comprehensive understanding of symptoms and the identification of possible mental disorders that require treatment [13]. The main goal of psychological treatment for obesity is to improve individuals’ thinking patterns, taking into account psychological challenges. In this context, the goal is to instigate changes in patients’ behavioral patterns, especially with regard to modifying their eating habits [14]. Furthermore, the psychological approach to obesity requires a multidisciplinary perspective that also assesses the physiological and biological aspects involved [14,15]. The focus of the psychology professional in the treatment of obesity lies in exploring the emotional causes underlying the dysfunctional behaviors that contribute to the maintenance of the condition. Therefore, the proposal of behavioral changes represents one of the central tools in this psychotherapeutic process [16].
Combating obesity requires a broader perspective that goes beyond exclusively biomedical approaches and recognizes the emotional and behavioral factors involved in its development and maintenance [17]. The interrelationship between psychological aspects and eating habits reinforces the importance of mental health professionals in monitoring patients with obesity [18]. Individualized psychological support contributes not only to weight loss but also to strengthening self-esteem, motivation, and the ability to cope with the challenges imposed by the condition [19]. In this sense, psychology not only helps with weight control but also plays an essential role in preventing relapses and building a more balanced lifestyle. Given the high prevalence of obesity and its association with harm to physical and mental health, the implementation of public policies that guarantee access to integrated health services with a preventive and therapeutic focus is urgently needed. The importance of psychology as an essential component in this process must be reinforced, as it contributes to more humane, effective, and individual-centered interventions. Thus, a psychological approach to combating obesity proves not only relevant but also essential for promoting quality of life and building a healthier society.
This study aimed to conduct an integrative review of the scientific literature on psychological procedures used in the assessment and treatment of obesity, with an emphasis on interventions that promote behavioral changes and enhance emotional control. The aim is to provide theoretical and practical support for healthcare professionals and to foster reflection on the importance of a psychological approach in combating obesity.
Methods
This study is an integrative review, classified as exploratory and descriptive. The research was conducted through bibliographical research in electronic databases on methods associated with SLR (Systematic Literature Review) and applications of SMARTER (Simple Multi-Attribute Rating Technique using Exploiting Rankings). The work is qualitative and quantitative in nature. Qualitative data analysis was performed intuitively and inductively during the theoretical framework survey. It is also quantitative through the use of the multicriteria method. Furthermore, a numerical experimental study was conducted to simulate an article selection situation based on the observed criteria.
The bibliographic research was conducted in the following databases: Web of Science; Science Direct; Wiley; Springer Link; Taylor and Francis; and PubMed. Additionally, searches were conducted using bibliographic references of studies that addressed the topic in a relevant manner on the Google Scholar search platform. The database search was conducted using terminology registered in the Health Sciences Descriptors created by the Virtual Health Library, based on the Medical Subject Headings of the US National Library of Medicine, which allows the use of common terminology in Portuguese, English, and Spanish. This study sought to investigate the literature on psychological procedures in the assessment and treatment of obesity. To this end, the descriptors “Obesity,” “Psychology,” “Behavioral Therapy,” “Obesity Treatment,” and “Psychological Assessment” were used, initially in English and subsequently in Spanish and Portuguese. As a tool to support decision- making in the selection and prioritization of articles, a set of criteria was considered essential to represent the state of the art on the research topic.
This method has the following characteristics:
(i) Rigorous logic allows for acceptance as a decision-support
tool
(ii) Simple to understand and apply, with easily interpretable results
References of selected papers were also searched for other documents of potential interest. Once eligible for full-text evaluation, articles were included in the qualitative review if they met the following inclusion criteria: a) addressed psychological interventions or assessments in individuals with obesity; b) were available in full. Articles were excluded if: a) duplicate articles; b) abstracts of scientific meetings, editorials, and letters to the reader; c) studies focused exclusively on pharmacological or surgical treatments, without a psychological approach; d) studies lacking a clear methodology.
The screening process was conducted in two stages: first, by reading the titles and abstracts; and then by reading the selected texts in full. To ensure the quality of the process, four independent reviewers performed the selection and data extraction, recording the information on a Microsoft Excel data extraction form. The extracted data included: author and year of publication, abstract, study type, population studied, psychological approach, main findings, and limitations, as demonstrated in (Table 1 & 2).
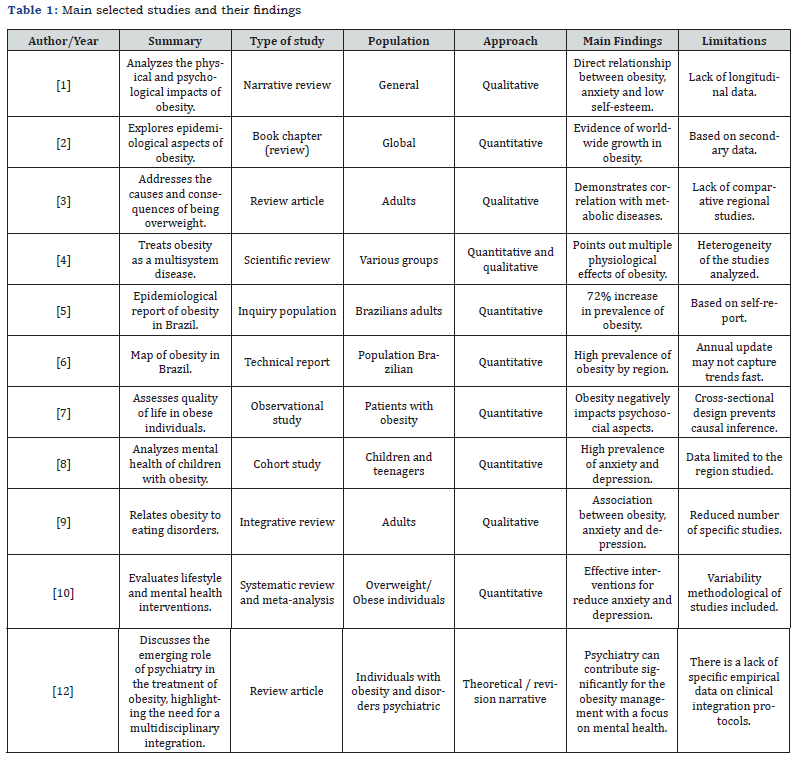
Source: Authors (2025)

Source: Authors (2025)
The selected data were organized and analyzed descriptively, presented in tables according to the categorization of emerging themes. Because this was an integrative review of published and public domain studies, without direct human involvement, submission to the Research Ethics Committee was not required, as per CNS Resolution No. 510/2016.
Results
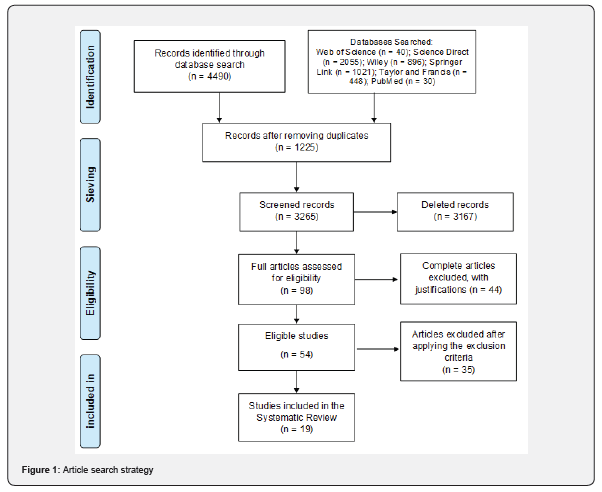
A systematic and comprehensive literature search yielded a total of 4,490 articles related to psychological procedures applied to the assessment and treatment of obesity. After the initial screening stage, 1,225 studies were excluded due to duplication.
To assist in the selection of the most relevant studies, the SMARTER (Simple Multi-Attribute Rating Technique using Exploiting Rankings) method was adopted, allowing for a thorough analysis of the previously established inclusion criteria. Based on this process, 98 articles were selected for full-text reading. After detailed analysis, 54 were deemed suitable for data extraction. However, 35 of these studies were subsequently excluded for not meeting the defined methodological and thematic criteria, resulting in a total of 19 eligible articles that comprised the final body of this integrative review. (Figure 1) presents the flowchart with the steps involved in the process of identifying, selecting, and including the analyzed studies.
Discussion
Obesity is a multifactorial condition characterized by complex interactions between genetic, behavioral, emotional, and environmental factors, which require integrated approaches for its understanding and management [2]. Studies indicate that the impacts of obesity go beyond metabolic and physiological changes, extending to relevant psychosocial dimensions, such as self-esteem, depression, and anxiety [1,7]. The increased prevalence of obesity observed in Brazil and worldwide highlights the need for interdisciplinary preventive and therapeutic strategies. Data from the Ministry of Health (2020) and ABESO (2023) show a sharp increase in the rates of the disease, with direct impacts on the population’s mental health. Studies indicate that psychological distress is both a cause and a consequence of excess weight [9]. Among the psychological impacts of obesity, low self-esteem, social stigma and isolation stand out, which can result in or be aggravated by anxiety, stress and depression [3,11]. Such comorbidities significantly interfere with treatment adherence and long-term clinical outcomes [7,10].
In this context, psychological interventions emerge as essen tial tools for a comprehensive approach to obesity. The literature highlights the effectiveness of cognitive behavioral therapy (CBT) in modifying dysfunctional thought and behavior patterns, promoting sustainable lifestyle changes. Furthermore, CBT helps reduce emotional eating and improve self-control [11]. The importance of psychological assessment in the early identification of psychiatric disorders associated with obesity is emphasized. The application of standardized instruments allows us to understand the motivations underlying eating behaviors and plan more effective interventions [12,13].
A multidisciplinary approach, which includes psychologists, nutritionists, physical educators and endocrinologists, is considered one of the most effective strategies for tackling obesity [15]. Studies indicate that programs that integrate psychosocial care achieve better results in terms of weight loss and long-term maintenance [19]. Additionally, the influence of sleep and stress on weight gain and difficulty in losing body fat has been widely documented [18]. The imbalance of the psych neuroendocrine axis compromises metabolism and favors compulsive behaviors, which reaffirms the need for integrated interventions that consider mental, physical and behavioral aspects [4].
Obesity in children and adolescents also represents a growing challenge, being associated with anxiety disorders, depression, and social isolation, which persist into adulthood [8]. Strategies aimed at promoting mental health from childhood are essential to reduce the impacts of obesity on biopsychosocial development.
Despite the relevance of psychological approaches, many health services still neglect this dimension in obesity treatment. Pearce, Rychetnik, and Wilson (2021) argue that health systems are still predominantly organized according to biomedical models, neglecting interventions based on promoting mental health and well-being.
Given this scenario, it is essential that public policies and clinical guidelines begin to incorporate psychological strategies as a structural part of obesity prevention and control programs. The psychologist’s work must be continuous and integrated into the health team to ensure support, qualified listening, and interventions based on psychological science [12].
Obesity must be understood as a complex phenomenon, and psychological interventions play an essential role in understanding and addressing it. The reviewed literature reinforces the urgency of interdisciplinary actions, with an emphasis on emotional and behavioral aspects, to ensure not only weight loss but also the promotion of comprehensive and sustainable health.
Final Consideration
Obesity is a multifactorial condition that demands integrated and interdisciplinary therapeutic approaches. The results of this integrative review reinforce the essential role of psychological approaches in both the assessment and treatment of obesity highlighting that emotional, behavioral, and cognitive aspects are directly associated with the development and maintenance of this chronic condition. Psychological interventions such as cognitive- behavioral therapy, psychoeducation, individualized psychotherapeutic monitoring, and lifestyle change programs mediated by psychologists have been found to be effective in controlling body weight, increasing treatment adherence, reducing binge eating, and improving the quality of life of obese individuals.
However, the literature analyzed still lacks methodological standardization, a significant number of longitudinal studies, and greater integration between quantitative and qualitative data. Therefore, we recommend developing more robust research that systematically evaluates the impact of different psychological strategies on obesity prevention and treatment. Furthermore, public health policies should consider mandatory inclusion of specialized psychology services in obesity care programs, promoting more humane, efficient, and comprehensive treatment.
References
- Rani D, Kohli N (2024) Physical and Psychological Consequences of Obesity: Implications for Interventions. IAHRW Int J Soc Sci Rev 12(1): 98
- Sørensen TIA, Martinez AR, Jørgensen TSH (2022) Epidemiology of Obesity. In: Epidemiology of Obesity 274: 3-27.
- Salam MM, Yousuf R, Salam MW, Haque M (2023) Obesity and Overweight. Adv Hum Biol 13(1): 154-156.
- Sarma S, Sockalingam S, Dash S (2021) Obesity as a multisystem disease: Trends in obesity rates and obesity-related complications. Diabetes Obes Metab 23(S1): 3-16.
- Brasil (2020) Ministry of Health. Secretariat of Health Surveillance. Department of Health Analysis and Surveillance, Communicable Diseases. of DN. Vigitel Brazil 2019: surveillance of risk and protective factors for chronic diseases by telephone survey: estimates on the frequency and sociodemographic distribution of risk and protective factors for chronic diseases in the capitals of the 26 states. Brasília: Ministry of Health Jul 16: 1-139.
- Associação Brasileira para o Estudo da Obesidade e da Síndrome Metabólica (ABESO) (2023). Mapa da obesidade.
- Jaison K I, Asharaf H, Thimothy G, George S, Jose J, et al (2024) Psychological impact of obesity: A comprehensive analysis of health-related quality of life and weight-related symptoms. Obes Med 45.
- Förster LJ, Vogel M, Stein R, Hilbert A, Breinker JL, et al. (2023) Mental health in children and adolescents with overweight or obesity. BMC Public Health 23(1): 1-11.
- Araújo RM de, Xavier GVDT, Maynard D da C (2025) Obesity and Eating Disorders: An Analysis of the relationship with depression and anxiety. Rev Eletrônica Multidiscip Investig Científica 4(20): 192-207.
- Amiri S, Mahmood N, Javaid SF, Khan MA (2024) The Effect of Lifestyle Interventions on Anxiety, Depression and Stress: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Healthcare 12(22): 2222-2263.
- Dakanalis A, Mentzelou M, Papadopoulou SK, Papandreou D, Spanoudaki M, et al. (2023) The Association of Emotional Eating with Overweight/Obesity, Depression, Anxiety/Stress, and Dietary Patterns: A Review of the Current Clinical Evidence. Nutrients 15(5): 1-18.
- Appolinario JC, Hay P, Coutinho W (2024) Bridging the gap: psychiatry’s role in the new era of obesity treatment. Rev Bras Psiquiatr 46: 1-3.
- Silva VG da, Santo FH do E, Ribeiro M de N de S, Pestana JLFM (2022) Instruments used in psychological assessment in the treatment of Obesity: an integrative review. Res Soc Dev (1): 1-14.
- Dandgey S, Patten E (2023) Psychological considerations for the holistic management of obesity. Clin Med (Northfield Il) 23(4): 318-322.
- Caranti DA, Inoue DS, Lira FS (2022) Editorial: Challenges for Obesity in the 21st Century: Psychology, Nutrition, Modern Lifestyle Behavior and Neuroendocrine Responses. Front Nutr 9: 1-3.
- Borges TVM, de Freitas TMM (2022) A terapia cognitiva comportamental como ferramenta auxiliar no combate an obesidade. Facit Bus Technol J 1(35): 1-21.
- Pearce C, Rychetnik L, Wilson A (2021) The obesity paradigm and the role of health services in obesity prevention: a grounded theory approach. BMC Health Serv Res 21(1): 1-10.
- Darku ED, Diyaolu CO (2025) The role of stress, sleep, and mental health in obesity and weight gain. Int Res J Mod Eng Technol Sci 31(6): 3216-3235.
- Tatlı Ç, Türker P (2024) The Roles of Psychosocial Factors and Nutritional Intervention on Eating Disorders. Süleyman Demirel Üniversitesi Sağlık Bilim Derg 15(2): 309-318.






























