A Hospital based Study on Prevalence and Clinical Presentation of Cataract in Northern India
Ragni Kumari1, Salal Khan2, Sunil Kumar Gupta3, Rajiv Janardhanan4, Jamshed Ali5 and Vishwdeep Mishra6
1,2,3,5,6Department of Optometry (E.I.A.H.S & R), Era University, Lucknow (U.P), India
4Professor, Faculty of Medical & Health Sciences, SRM Institute of Science & Technology, Kattankulathur, Tamil Nadu, India
Submission: March 05, 2024; Published: March 22, 2024
*Corresponding author: Salal Khan, Assistant Professor, Department of Optometry, Era University, Lucknow, U.P, India
How to cite this article: Ragni K, Salal K, Sunil Kumar G, Rajiv J, Jamshed A, et al. A Hospital based Study on Prevalence and Clinical Presentation of Cataract in Northern India. JOJ Ophthalmol. 2024; 10(5): 555797. DOI: 10.19080/JOJO.2024.10.555797
Abstract
Purpose: The major goal of this study was to investigate and compare the prevalence of cataract and its associated factors among the rural and urban population.
Material & Methods: An Observational cross-sectional study was conducted to estimate the prevalence of cataract among the rural and urban population. A total of 9023 (mean age: 55±2.51 years) patients (male=4848 & female=4175) were enrolled in this study. The subjects underwent a comprehensive eye examination. Information on the patient’s lifestyle, habits, indoor & outdoor activities, socioeconomic status and systemic diseases were collected using a self-structured questionnaire. The collected data were analyzed to explore the factors associated with cataract using the Pearson Chi-square test for each factor through SPSS version 17.0.
Results: Out of the total 9023 enrolled in the study, only 3348 (37.1%) were from rural while 5675 (62.9%) were from urban backgrounds. The majority of the participants (80%) did not have any history of addiction. Only 12% consumed smokeless tobacco (nonsmokers) products, 7% were habitual smokers, and 1% to alcohol. Amongst those having cataracts, the majority of patients had cortical cataracts (66.2%), followed by nuclear (27.1%) and a small number (6.6%) of posterior subcapsular cataracts. As per the study's findings, the overall prevalence of cataracts in the rural population is much higher, 93.5%, compared to the urban population, where it is only 57.1%. All parameters were found to be statistically significant with the Pearson Chi-square test. A p-value of < 0.05 was considered as significant.
Conclusion: Amongst the general population prevalence of senile cataracts is relatively high, and cortical cataract is the commonest type of senile cataract. The prevalence of cataracts is higher in the outdoor workers, and patients with lower socioeconomic status. Patients addicted to the tobacco, alcohol and cigarette smoking is also affected from the cataract conditions in rural population greater than the urban population.
Keywords: Cataract; Public health; Smokers; Diabetes mellitus; Optometry
Introduction
According to World Health Organization (WHO) cataract is clouding of the lens of the eye, which initially prevents clear vision and eventually progresses to blindness if left untreated [1]. It causes increased light sensitivity, decreased vision at night, seeing double images and leads to total blindness [2]. The term cataract was introduced by Constantinus African. He translated the Arabic "suffusion" into Latin "Cataracta," meaning "something poured underneath something," the "waterfall." It possesses all the characteristics of a biconvex lens physically. The eye's lens performs similar functions to a camera's lens. The Lens directs light rays entering the eye to the Retina's sensitive layers. Senile cataract, the most prevalent form of acquired cataract, also known as an "age-related cataract," affects people of both sexes equally and typically develops after age 50. More than 90% of people experience senile cataracts by age 70. Although one eye is almost always afflicted before the other, the disorder is typically bilateral.
Morphologically, the senile cataract occurs in two forms, the cortical (soft cataract) and the nuclear (hard cataract). Generally, the predominant form is cortical or cuneiform 70 percent, nuclear 25 percent, and cupuliform or posterior or subcapsular 5 percent. Specialized proteins (referred to as crystallins) are present in the lens, and their optical characteristics are based on the precise arrangement of their three-dimensional structure and hydration. Osmotic and ionic equilibrium is maintained throughout the lens by membrane protein channels. In contrast, the lens cytoskeleton, particularly the fiber cells of the nucleus, contributes to the distinctive form of the lens cells. High levels of reduced glutathione, known as the "mother of all antioxidants," shield the protein-bound sulfhydryl (SH)-groups of crystallins against oxidation and cross-linking. The larger crystallins, which can absorb radiation energy (shortwave visible light, ultraviolet, and infrared radiation) over longer times without essentially changing their optical properties, give these materials high spatial and temporal stability (heat-shock proteins). This also provides a substantial protective function for the activity of various enzymes of carbohydrate metabolism [3]. It is commonly acknowledged that oxidative stress plays a significant role in the onset of senile cataracts.
Due to their inability to extrude, faulty cells either undergo apoptosis or necrosis-based degradation or are relocated to the posterior capsular region, where they aid in developing posterior subcapsular cataracts [4]. Additionally, nutritional and trace metal shortages, smoking, toxic chemicals like drug misuse, alcoholism, etc., and radiation (ultraviolet, electromagnetic waves, etc.) can cause oxidative stress and osmotic imbalance. It is causing the development of cataracts. However, it is obvious that the precise pathophysiology of the risk mentioned above factors needs to be understood [4].
Methodology
The study was conducted at Era Lucknow Medical College and Hospital, Lucknow, Uttar Pradesh, from January 2019 to July 2022 after obtaining prior institutional ethical clearance from Era University and advertising informed consent forms to the participants enrolled in the study. The study design was an Observational cross-sectional study, and it was included the sample random sampling methods to collect the data by following the protocol of the study. A standard pre-test questionnaire on the patient’s demographic profile and degree of visual handicap was administered and sample size calculation methods were used to decide the sample size for this study.
Inclusion Criteria:
All the patients diagnosed with cataracts in the age group of more than 50 years were included in the study.
Exclusion Criteria:
It excluded pre-clinical stage of cataract and patients who did not agree to participate in this study. Also excluded patients’ age group less than 50 years of age and if patients having any pathological conditions of the eye.
Data Analysis:
In this study, measurable dissects were performed utilizing SPSS Version 23.0, All analyses were tested using two-sided hypothesis tests, and a p value of less than 0.05 was assumed to indicate significance. The statistical hypothesis was tested using the Pearson chi-square test.
Results
All the subjects enrolled in the study were adults the age of 50 years or above, regardless of gender and demographic settings. Out of the total 9023 enrolled in the study, only 3348 (37.1%) were from rural while 5675 (62.9%) were from urban backgrounds. The urban population outnumbered the rural population, probably because of the urban setting of the place of study. Overall gender distribution showed male (4848) subjects outnumbered female (4175) subjects enrolled in the study. A similar pattern of gender distribution is reflected in both rural and urban participant populations individually (Table 1).
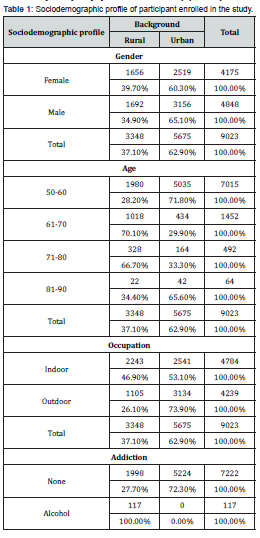

The majority of the participants were aged 50-60 years (7015), and as the age group advanced number of participants was reciprocally proportional. The majority of subjects enrolled in the study from urban areas reported comparatively at a younger age in contrast to those from rural backgrounds. Most of the subjects from the urban areas were aged between the ages 50-60 years, while the subjects from the rural areas were between age 60-80 (Table 1).
The working background of the 9023 individuals was almost evenly distributed; 4784 (53%) worked indoors, while 4239 (47%) worked outdoors. Working hours of eight hours or more per day in a particular environment were taken as criteria for labeling an individual as an indoor and outdoor worker. Analysis revealed that a smaller number of indoor workers (46.9%) were from rural areas compared to those from urban areas (53.1%). Among those subjects working outdoors, 26.1% were from rural areas, and 73.9% were from urban areas (Table 1). The majority of the participants (80%) did not have any history of addiction. Only 12% consumed smokeless tobacco (nonsmokers) products, 7% were habitual smokers, and 1% to alcohol (Table 1). Addiction was more common in the participants from rural backgrounds. All the alcoholics and smokers were from rural areas, along with the tobacco chewers (57.4%) (Table 1).
Most of the participants enrolled in the study belonged to the upper socioeconomic class (72%), followed by the lower (18%) and middle class (10%). When the urban and rural background was further elaborated, it revealed that in the upper socioeconomic group, the majority of the patients were from urban areas (87.3%), while all the participants from rural backgrounds were from middle and lower socioeconomic classes (100%) (Table 1). The majority of the participants were free of any associated systemic disease (80.7%), and only a small percentage of them had Diabetes Mellitus (DM) (8.8%), hypertension (HTN) (8.4%), DM with HTN (0.6%) and others (1.6%). Patients with systemic diseases were mainly from rural backgrounds (Table 1). The majority of participants were free of any other ocular diseases (90.9%). Associated ocular diseases among participants included diabetic retinopathy (DR) (6%), hypertensive retinopathy (HTR) (1.5%), and others (1.6%) (Table 1).
Prevalence and Clinical Presentation of Cataract
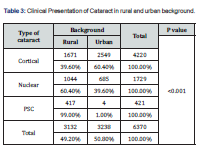
Out of the 9023 participants enrolled for the study, 6370 (70.6%) had cataracts. Amongst those having cataracts, the majority of patients had cortical cataracts (66.2%), followed by nuclear (27.1%) and a small number (6.6%) of posterior subcapsular cataracts. As per the study's findings, the overall prevalence of cataracts in the rural population is much higher, 93.5%, compared to the urban population, where it is only 57.1%. This may be explained because cataract gives early blurring of vision, and people in urban settings are more conscious of clarity of vision. So, people seek medical advice while villagers work with even decreased vision (Table 2). In rural populations, Posterior Subcapsular Cataract (PSC) was the more common type of cataract (99%), followed by nuclear cataract (60.4%). While in the urban population, cortical cataract was more common (60.4%). This result was statistically significant (p<0.001) (Table 3). However, no specific reason can be assigned for this variation.

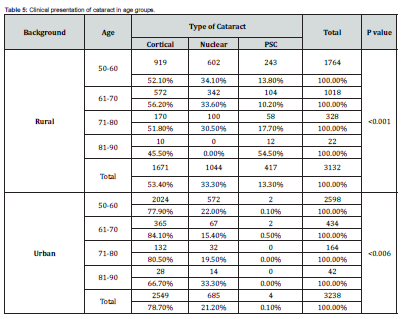
Prevalence and Clinical Presentation of Cataract According to Age

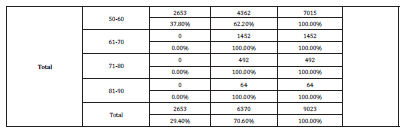
With increasing age (60 years beyond) presence of cataracts, in their varying grades differing from individual to individual was universal. In the rural population (89.1% age 50-60 years), cataract seems to start developing at a comparatively early age compared to the urban population (51.6% age 50-60 years). This result was statistically significant (p<0.001) (Table 4). Cortical cataract was more common in an urban population in every age group except in the case of nuclear cataract, which was found to be predominant in subjects belonging to the advanced age of 81-90 years in the urban population as compared to the rural population. The majority of the patients had PSC in the rural population, and this result was statistically significant (p<0.001) (Table 5).

Prevalence and Clinical Presentation of Cataract Vs. Gender
Overall prevalence of cataract amongst males (87.7%), outnumbered females (50.7%) (Table 6).
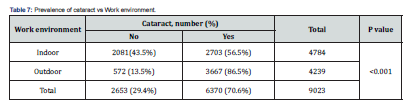
Prevalence and Clinical Presentation of Cataract in Work Environment
Work environment of participants was classified on the basis of their nature of work and the time spent in that environment. Individual working or staying for 8 hours or more in particular working condition was labelled as indoor or outdoor workers. We included housewife, teachers, computer operators, office workers and retired professionals under the category of indoor workers; whereas laborer’s, farmers, drivers and traffic police etc. were included under the category of outdoor workers. Amongst outdoor workers (86.5) cataract was more common in comparison to the indoor workers (56.5%), and this finding is statistically significant (p <0.001) (Table 7).

Correlation with Prevalence and Clinical Presentation of Cataract with Socioeconomic Status of the subjects enrolled in the Study
Further analysis revealed that cataract cases in the rural population are evenly distributed regardless of socioeconomic status. The majority of the individuals (93.2%) diagnosed as having cataracts belonged to the lower socioeconomic status, followed by the middle (91.5%) and upper class (61.1%). In contrast, in the urban population, there were no participants from the lower and middle classes, and in the upper class, only 57.1% of patients were found to have a cataract. This finding is statistically significant (p <0.001) (Table 8).
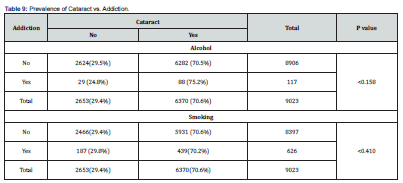
Prevalence and Clinical Presentation of Cataract in Addicts
Prevalence of cataract amongst tobacco users is significantly higher in comparison to the patients who did not consume tobacco products. Tobacco consumption seems to have statistically significant effect on the development of cataract (p <0.001). Consumption of alcohol and smoking tobacco products didn’t have a statistically significant effect on development of cataract (p = 0.158 and 0.410, respectively) (Table 9).

Prevalence and Clinical Presentation of Cataract in Participants with Comorbidities
Comorbid conditions do not seem to influence the development of senile cataracts. In participants from the rural populations, the prevalence of cataracts was 95.4% without any comorbidities, while those with associated systemic comorbidities had an equal prevalence of cataracts (91.8%). In the urban population, only 57% reported cataracts without any comorbidities. Since the number of cases with associated comorbidity from the urban population was too small (only 12 cases), the data cannot be taken as representative. This result was statistically significant (rural <0.001, urban <0.029) (Table 10).


Discussion
A higher proportion of the male population may prevail due to social structure of society. However, a study conducted in India recorded 41% men and 59% women, which is contrary to the present study's findings. This may be because of the differences in the setting of the study [5]. Participants work environment was classified based on their nature of work and the time spent in that environment. Individuals working or staying for 8 hours or more in particular working conditions were labeled as indoor or outdoor workers. As indoor workers, we included housewives, teachers, computer operators, office workers, and retired professionals. In outdoor workers, we included laborers, farmers, drivers, traffic police & others.
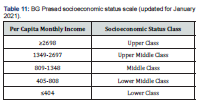
Socioeconomic status (SES) is a major risk factor affecting the health status of a person or a family. Participants in the study were from varied socioeconomic strata, upper class (72%), lower class (18%), and middle class (10%). In the present study, BG Prasad's socioeconomic status scale was adopted to grade the SES of participants enrolled in the study (Table 11). Considering the associated comorbidities, the majority of participants were free of any associated systemic diseases (80.7%), only a small proportion of them had Diabetes Mellitus (D.M.) (8.8%), hypertension (HTN) (8.4%), D.M. with HTN (0.6%), and others (1.6%). Patients with systemic diseases were mainly from rural backgrounds (Table 1). The overall prevalence of cataracts was 71% in the present study. A similar prevalence has been reported in southern India (61.4%) [6]. various other studies in the Indian subcontinent have found a higher prevalence of cataracts in northern India (58%) and in southern India (53%) [7,8]. The differences in cataract prevalence reported in different studies could be due to several reasons, including differences in ethnicity, clinical and epidemiological features of the population, and age group of the population. [9,10] In the present study, population living background is a risk factor for developing cataracts; in the rural population (OR 10.9, CI 9.4-12.6, p<0.001), the risk of developing cataracts was 10.9 times higher than in the urban population.
Amongst those having cataracts, the majority of them had cortical cataracts (66.2%), followed by nuclear (27.1%) and a small number of posterior subcapsular cataracts (6.6%). In the Tanjong-Pagar survey in 2003, cortical cataracts (62%) were high, and reports were akin to the present study [11]. Previous studies [12] have shown that nuclear cataract was more common in northern India (48%) than in southern India (38%). In contrast, the present study conducted in Northern India showed cortical cataract was more common. Oxidative stress plays a different role in the development of nuclear cataract than in cortical cataract. The work of Neale et al. (2003)[13] suggests that the majority of UV-induced lens damage occurs before age 30 in the cortical lens fibers, which gradually shift to the centre of the nucleus as the lens ages, supporting the role of a cumulative effect of occupational hazards, including sun exposure, especially when it begins at a young age.
The prevalence of PSC in the present study is broadly in accord with some previous studies in India and Asia, although the prevalence rates in the Shih-Pai [14,15] studies appeared to be somewhat lower. Prevalence rates of PSC opacities are consistently lower in the Western population, with rates of approximately 5% to 8% [16-20].
The evidence published in the literature that ultraviolet radiation is a risk factor for cataracts is strongest for cortical cataracts [21]. Exposure to ultraviolet radiation depends on latitude, occupation, and behavioral factors; genetic factors have also been strongly correlated with the development of cortical cataracts [22], although only a few genes have been identified. In the rural population (89.1% age 50-60 years), cataract seems to start developing at a comparatively early age as compared to the urban population (51.6% age 50-60 years). This observation is consistent with a study conducted on the rural population in Pondicherry, which showed a steep increase (75.1%) in cataract cases in subjects over 50 years of age [23,24]. Age is an important predisposing factor for the development of senile cataract, which was clearly established in this study. The increasing risk trend with age is most significant in nuclear cataract, and this finding is consistent with the results of other studies [25-28] and suggesting a natural aging process of the nucleus and possibly a cumulative effect of certain risk exposures throughout life.
Present study found a higher prevalence of cataracts in males compared with females, and this finding is contrary to observations made by Nirmalan P.K Krishnaiah et al.; (2003) & S Lewallen et al.; (1995) [29,30]. Exposure to indoor smoke has been implicated as one of the causes; toxins from biomass fuel smoke are systematically absorbed and accumulate in the lens, leading to the appearance of the cataract [31]. Two separate studies conducted in Aligarh (U.P.) by Khan et al.; 2017[32] in Aligarh Maroof et al. 2017[33], did not find any gender bias in the prevalence of cataracts. In the present study, there was gender bias whilst estimating the risk factor for developing a cataract (OR, 6.9 CI 7.31-7.74, p<0.001). Men were found to develop cataracts 6.9 times more than women.
Regardless of the work environment, indoor and outdoor PSC was seen more commonly seen in the rural population (indoor and outdoor workers, 14.1% and 11.5%, respectively) as compared to in the urban population (indoor and outdoor workers, 0.7% and 0% respectively. In the rural population, domestic workers were also similarly affected (95.2% and 90.1%, respectively), possibly due to household air pollution from burning solid fuels for cooking, including coal and biomass fuels (wood, crop residues, and manure). This form of energy use has been shown to be associated with high levels of indoor air pollution and an increase in the incidence of cataracts in adults and children [34]. According to research by D. G. Fullerton et al. [34], this type of energy used in daily activities is associated with high indoor air pollution and an increase in the prevalence of cataracts in adults. There are numerous reports in the literature that kerosene use is associated with nuclear and posterior subcapsular cataracts, particularly in women who have been exposed to biomass gas cookstoves for prolonged periods of time [35-36].
Jones et al. [37] & Kakkar et al. [38] have examined the relationship between DM and cataracts and have unanimously found that D.M. patients are at significant risk for cataracts. In a review article by Drinkwater et al. [39] the authors have maintained that age (year) and blood glucose levels were associated with a higher risk of cataract formation. However, another study Khan et al. [32] found that the duration of D.M. is the main risk factor for the occurrence of cataracts. Associated systemic conditions can further increase your risk of developing cataracts. Analysing the study's results reveals that individuals with diabetes mellitus have a four-fold increased risk of developing cataracts compared to those without the disease, whereas hypertensives and those with other combination illnesses had a ten-fold increased risk. According to Kiziltoprak H et al. [40] excessive levels of glucose in aqueous humour in diabetes mellitus initially diffuse into the lens before being converted to advanced glycation end products, which build up in the lens and are crucial for the development of cataracts.
Conclusion
Amongst the general population prevalence of senile cataracts is relatively high, and cortical cataract is the commonest type of senile cataract. The prevalence of cataracts is higher in the outdoor workers, and patients with lower socioeconomic status. Patients addicted with the tobacco, alcohol and cigarette smoking is also affected from the cataract conditions in rural population greater than the urban population.
References
- Lim SA, Park Y, Cheong YJ, Na KS, Joo CK (2016) Factors affecting long-term myopic regression after laser in situ keratomileusis and laser-assisted subepithelial keratectomy for moderate myopia. Korean J Opthalmol 30(2): 92-100.
- Moshirfar M, Shah TJ, Skanchy DF, Linn SH, Durrie DS (2017) Meta-analysis of the FDA reports on patient-reported outcomes using the three latest platforms for LASIK. J Refract Surg 33(6): 362-368.
- Roberts CJ (2000) The cornea is not a piece of plastic. J Refract Surg 16(4): 407-413.
- Roberts CJ (2005) Biomechanical customization: The next generation of laser refractive surgery. J Cataract Refract Surg 31(1): 2-5.
- Roberts CJ, Dupps WJ (2014) Biomechanics of corneal ectasia and biomechanical treatments. J Cataract Refract Surg 40(6): 991-998.
- Ikeda T, Shimizu K, Igarashi A, Kasahara AS, Kamiya K (2017) Twelve-Year Follow-Up of Laser In Situ Keratomileusis for Moderate to High Myopia. Biomed Res Int p. 7.
- Agudo JAR, Park J, Park J, Lee S, Park K (2019) Laser asymmetric corneal ablation to improve corneal shape. Lasers Med Sci 34: 1763-1779.
- Min JS, Min BM (2020) Comparison between surgical outcomes of LASIK with and without laser asymmetric keratectomy to avoid conventional laser refractive surgery adverse effects. Scientific Reports 10: 10446.
- Min JS, Min BM (2021) Comparison of outcomes of laser refractive surgery (LRS) alone and LRS with laser asymmetric keratectomy in patients with myopia: A retrospective study. Medicine (Baltimore) 100(14): e25366.
- Min JS, Min BM, Lee DC (2021) Laser asymmetric keratectomy using a semi-cylindrical ablation pattern to avoid adverse effects of laser refractive surgery. Austin J Clin Ophthalmol 8(2): 1120.
- Min JS, Min BM (2021) A novel approach to enhancement linked laser asymmetric keratectomy using semi-cylindrical ablation pattern in patients with myopic regression after laser refractive surgery. Clin Ophthalmol 15: 1751-1758.
- Min JS, Min BM (2021) Clinical outcomes of laser asymmetric keratectomy to management postoperative adverse effects-A retrospective clinical trial. The Open Opthalmol J 15: 171-177.
- Min JS, Jin LY, Min BM (2020) Early postoperative changes after laser asymmetric keratectomy for the management of adverse effects after photorefractive keratectomy. J ophthalmol Open Access 1: 1-7.
- Min BM (2023) Corneal remodeling of laser asymmetric keratectomy combined with collagen cross linking in patients with keratoconus suspect. J Ophthalmol Open Access 7: 1-10.
- Min JS, Lee DC, Lee SS, Min BM (2024) A Novel approach for corneal remodeling of laser asymmetric keratectomy with collagen cross linking in patients with keratoconus suspect. The Open Ophthalmol J 18: 1-9.






























