Role of Cardiovascular Magnetic Resonance Imaging in Early Detection of Myocarditis in Patients Recovered from COVID-19
Hany Hassan Ahmed Ebaid1, khaled Y Elnady2, Ahmed Abdel Moniem1, Mohamed Ibrahim Awadeen1* and Mohamed Mahrous Ali1
1Department of Cardiology, Faculty of Medicine, Benha University, Benha, Egypt
2Department Cardiology, Military Medical Academy, Cairo, Egypt
Submission: September 11, 2023;Published: September 20, 2023
*Corresponding author: Mohamed Ibrahim Awadeen, Faculty of Medicine, Benha University, Benha, Benha, Al-qalyubia governorate, Egypt
How to cite this article:Hany Hassan A E, khaled Y E, Ahmed A M, Mohamed I A, Mohamed M A. Lipoprotein-A vs. Role of Cardiovascular Magnetic Resonance Imaging in Early Detection of Myocarditis in Patients Recovered from COVID-19. J Cardiol & Cardiovasc Ther. 2023; 18(5): 555997. DOI: 10.19080/JOCCT.2023.18.555997
Abstract
Objective: To assess cardiac involvement in patients recovered from COVID-19 with no clinical evidence of myocarditis, using various non-invasive parameters including Transthoracic Two-dimensional Speckle Tracking Echocardiography (STE) and cardiac magnetic resonance imaging (CMR).
Methods: This prospective study was conducted in the Cardiology Departments of Maadi Military Hospital and Benha University Hospitals. A total of 74 patients were initially enrolled during their hospital stay, but only 50 of them met the inclusion and exclusion criteria. The CMR examination was performed in conjunction with echocardiography, ECG, and laboratory investigations on the same day, which occurred 2-12 weeks after recovering from confirmed COVID-19 infection. Patient scheduling for CMR and other examinations depended on the availability of the CMR machine.
Results: According to CMR diagnosis, 23 (46%) patients were diagnosed to have myocarditis by CMR, the patients were categorized into two groups based on these results: normal group (27 patients) & myocarditis group (23 patients). According to GLS, 21 (42%) patients were diagnosed to have myocarditis by STE (diagnosis of Myocarditis with Global longitudinal strain was considered with cut-off point of >-21.33 with Sensitivity of 91.30% and Specificity of 92.59% (P <0.0001). 2D STE showed 87.50% sensitivity, 92.31% specificity and 90.00% accuracy to diagnose myocarditis, while CMR showed a 95.83% sensitivity, 96.15% specificity of and 96.00% accuracy.
Conclusion: Myocarditis was found in 46% of asymptomatic COVID-19-recovered patients. CMR is a valuable tool for early myocarditis detection when combined with 2D STE, offering high accuracy. Significant differences were observed between suspected myocarditis patients and those with normal results on both 2D STE and CMR.
Keywords:CMR; 2D STE; Myocarditis; Post COVID-19
Introduction
COVID-19 is a contagious illness caused by the SARS-CoV-2 virus, which was initially identified in Wuhan, China, in December 2019 and subsequently spread worldwide [1].
The COVID-19 pandemic has had far-reaching effects on global health, society, and economies [2]. The primary target of COVID-19 is the lungs, as the SARS-CoV-2 virus invades pulmonary tissue through the angiotensin-converting enzyme 2 (ACE2) receptor [3].
ACE2 is not limited to the pulmonary system but is also found in various other organs, including the cardiovascular system [4]. There is evidence linking COVID-19 to various cardiovascular complications, such as arrhythmias, myocarditis, acute coronary syndrome, acute onset heart failure, and cardiac arrest. Additionally, a strong association has been observed between acute cardiac injury and increased mortality rates among COVID-19 patients [3].
Previous research has indicated that a significant proportion of COVID-19 patients, ranging from 12% to 15%, exhibit elevated levels of high-sensitive cardiac troponin I (hs-cTnI) during their hospitalization, indicating myocardial injury. Furthermore, severe cases of COVID-19 may have cardiac involvement in as many as 31% of patients, but it remains uncertain how long this cardiac involvement persists after recovery [5,6].
SARS-CoV-2 has the potential to induce the release of chemokines and cytokines, which can lead to vascular inflammation, destabilization of atherosclerotic plaques, and myocardial inflammation. Consequently, elevated troponin levels in these patients could be attributed to stress cardiomyopathy, microvascular thrombosis, demand ischemia, and the secondary effects of systemic inflammation. Another possible cause of myocardial damage associated with COVID-19 is direct viral infection of the myocardium, potentially indicating viral myocarditis. While myocarditis-like clinical presentations have been reported in a small number of COVID- 19 patients, suggesting that fulminant myocarditis is uncommon [7].
Cardiovascular magnetic resonance (CMR) has emerged as the preferred non-invasive imaging technique for assessing heart volume, function, and myocardial tissue characteristics in cardiovascular medicine. Abnormalities in cardiac magnetic resonance (CMR) related to COVID-19 have been identified in 78% of predominantly ambulatory adults [8].
The main aim of our investigation was to evaluate the degree of cardiac engagement in individuals who have recuperated from COVID-19. We achieved this by employing cardiac CMR as a highly sensitive imaging method and comparing it to Transthoracic Echocardiography with 2D STE.
Patients and Methods
This prospective study was done in cardiology department of Maadi Military hospital & Benha University hospitals over 74 patients who were enrolled for this study during their hospital stay. Only 50 patients were fulfilling the inclusion and exclusion criteria and were enrolled in the study after 2-12 weeks after discharge from hospital with diagnosis of (SARS-CoV-2) by PCR on swab test of the upper respiratory tract.
The Banha Faculty of Medicine Human Research Ethics Committee approved the study protocol, and informed consent were obtained from Benha University prior starting data collection. This study was conducted over a 1-year duration, spanning from January 2021 to January 2022.
Inclusion criteria
Patients who previously confirmed with SARS-CoV-2 infection using (RT-PCR) swab test (who needs hospital admission due to significant lung affection or decreased oxygen saturation > 90%) and considered recovered by the discharging criteria ( resolved respiratory symptoms, normal temperature lasting longer than 3 days, 2 consecutive negative RT-PCR test results separated by at least 24 h and substantially improved exudative lesions on chest CT images) and were isolated for two weeks and have no any cardiac symptoms. All patients agreed to participate and sign informed consent.
Exclusion criteria were active Covid-19 infection. Previous myocardial infarction or coronary artery disease (evidence of coronary artery stenosis > 50%) , history of ischemic heart disease, previous myocarditis or heart failure, or known cardiomyopathy, uncontrolled hypertension, extremely irregular heart rates or previous atrial fibrillation, moderate to severe valvular heart disease, inability to effectively take part in breath-holding procedures and is thus unsuitable for undergoing CMR assessment, intra-cardiac devices non-MRI compatible (ICDs– Pacemakers), significant renal impairment ((CrCl rate < 30 mL/min/1.73 m2), contraindications to gadolinium contrast, disagree to participate or sign informed consent and insufficient CMR image quality for analysis.
All cases underwent a full history taking, complete physical examination, 12 leads Electrocardiogram, laboratory investigations (Creatinine, Troponin I & CBC), trans-Thoracic Echocardiography which was done for all patients according to EACVI Echocardiography guidelines [9] (Conventional study & 2D Speckle tracking), and CMR.
Protocol for CMR scanning included the following
conventional sequences: long-axis and short-axis cine, late gadolinium enhancement (LGE) and T2- weighted imaging (T2WI).
Quantitative mapping sequences: post-contrast T1 mapping and native T1/T2 mapping.
The diagnosis of myocarditis was confirmed by Updated Lake Louis criteria (2018) for diagnosis of Myocarditis which consist of two main criteria (T1-based criterion and T2-based criterion). The T1-based criteria is regarded as positive when there are increases in native T1 relaxation durations, increases in extracellular volume (ECV), or the presence of positive LGE.
The T2-based criterion is positive when there is an increase in T2 relaxation times, regionally high T2 signal intensities on T2- weighted images, or an elevation in the global T2-signal intensity ratio.
Supportive Criteria: pericardial effusion, pericardial signal abnormality, systolic LV dysfunction. All CMR images were evaluated by consultant cardiologist with 6 years of CMR diagnosis experience.
Sample size
Using PASS software, the minimum sample size required for specificity and sensitivity tests was calculated (PASS 11 citation: Hintze J (2011). PASS 11. NCSS, LLC. Kaysville, Utah, USA). The required sample size for the study is determined to be 50 patients without accounting for dropout rate.
Statistical Analysis
We conducted the statistical analyses using SPSS software (Statistical Package for the Social Sciences, version 24, SSPS Inc, Chicago, IL, USA). Categorical variables were presented in frequency tables with corresponding percentages, whereas descriptive statistics like standard deviation and mean were used to describe numerical data. Data entry, processing, and statistical analysis were performed using MedCalc ver. 20 (MedCalc, Ostend, Belgium). We employed various tests of significance, including logistic multiple regression analysis and ROC Curve analysis. The choice of analysis method was based on the nature of the data, whether it was parametric or non-parametric. We considered p-values less than 0.05 (5%) to be indicative of statistical significance [10].
Results
Table 1 shows demographic data, risk factors and vital signs in all studied group. Table 2 shows ECG data, lab investigations, 2D speckle tracking Echocardiographic parameters and diagnosed myocarditis by CMR in all studied group.
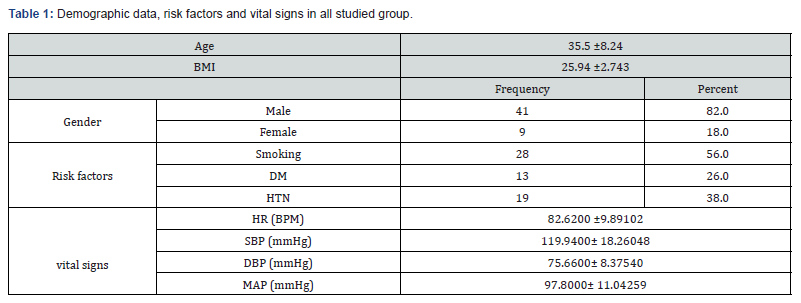
BMI: body mass index, HTN: hypertension, DM: diabetes mellitus, HR: heart rate, SBP: systolic blood pressure, DBP: diastolic blood pressure, MAP: Mean Arterial pressure.
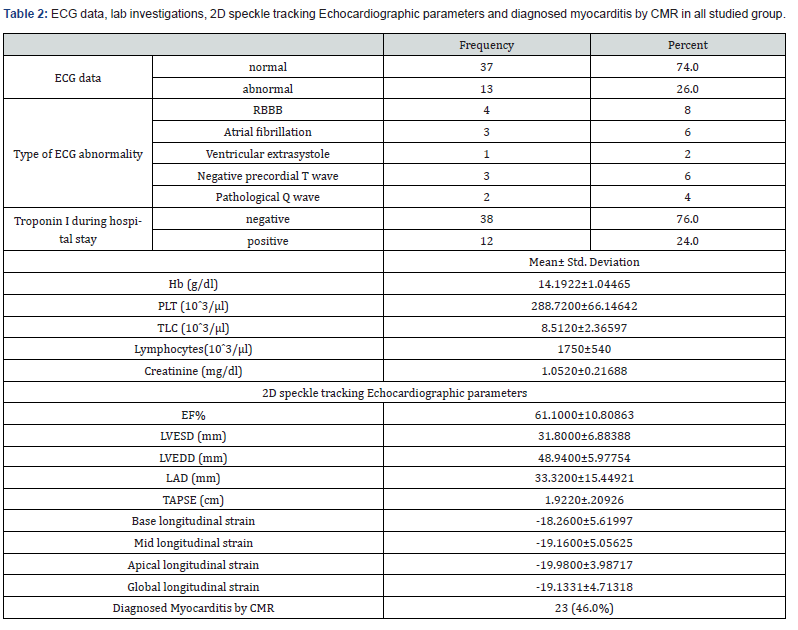
EF: Ejection Fraction, LVESD: Left Ventricular End-Systolic Dimension, LVEDD: Left Ventricular End-Diastolic Dimension, LAD: Left Atrial Dimension, TAPSE: Tricuspid Annular Plane Systolic Excursion.
According to CMR diagnosis, 23 (46%) patient was diagnosed to have Myocarditis by CMR using Updated Lake Louis criteria (2018) and patients were categorized into two groups based on these observations: normal group (27) patients & myocarditis group (23) patients.
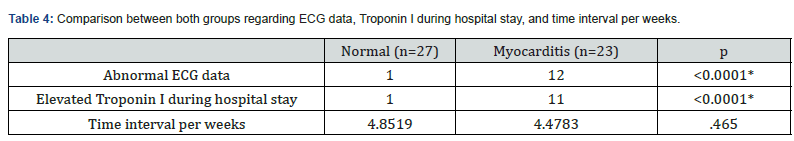
There was no statistically significant difference between both groups regarding age, sex, BMI, SBP and MAP. While the HR, DBP & TLC were higher in myocarditis group than in normal group with statistically significant difference (P=0.008, p=0.006 & p= 0.001 respectively). The lymphocytic count was lower in myocarditis group with statistically significant difference (p<0.001). Table 3 A statistically significant difference was seen between the two groups regarding ECG data and Troponin I during hospital stay with higher incidence of abnormal ECG & elevated Troponin I in myocarditis group than the other group. (P<0.0001). Time interval per weeks was about 4.5 weeks between hospital discharge & CMR & Echocardiographic examination with no significant difference between both groups. Table 4 Average left ventricular (LV) systolic function in myocarditis group was significantly lower than the normal group (P <0.001). Differences between the two groups were statistically significant concerning the LVESV (P = 0.012) & the LVEDV (P = 0.002). The average right ventricular ejection fraction (RVEF) was no significant difference between both groups. Global native T1, T2 values showed significant elevation in myocarditis group compared with the normal group (P. <0.001). Global Native T2 was significant high in the myocarditis group than in the normal group (P.<0.001). Pericardial enhancement and pericardial effusion were found in 14 patients (60.8%) of myocarditis group and was absent in normal group (P. <0.001). According to 2D STE parameters, there was a statistically significant difference between both groups regarding EF (P<0.0001), LVESD (P=0.014) TAPSE (P=0.028) and LAD (P <0.0001).
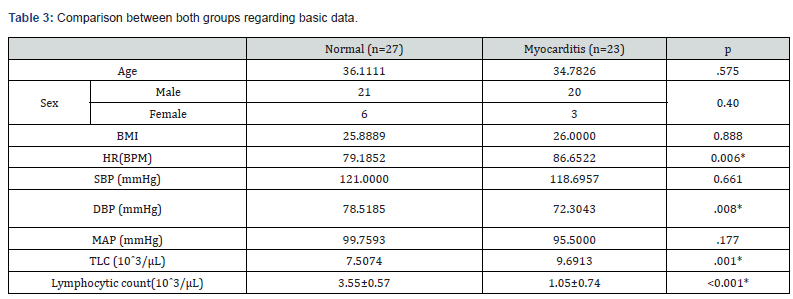
*: significant P value, BMI: Body Mass Index, DM: Diabetes Mellitus, HTN: Hypertension, HR: Heart Rate, SBP: Systolic Blood Pressure, DBP: Diastolic Blood Pressure, MAP: Mean Arterial Pressure.
Global longitudinal strain was significantly lower in myocarditis group (-16.34% vs -23.07%). Also, base longitudinal strain, mid longitudinal strain and apical longitudinal strain were lower in myocarditis group (P<0.0001) (Table 5).
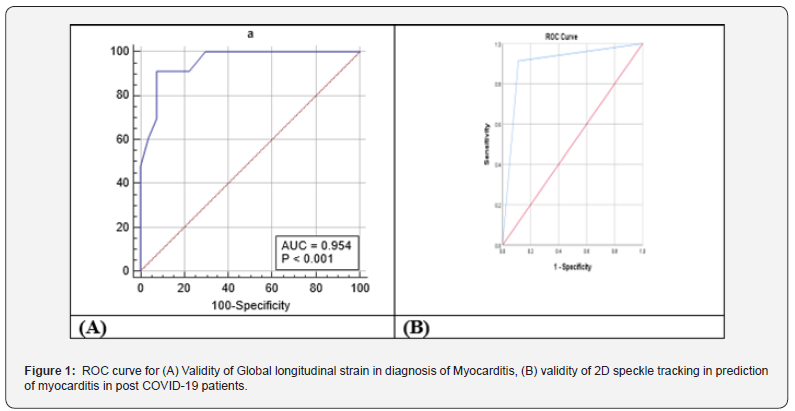
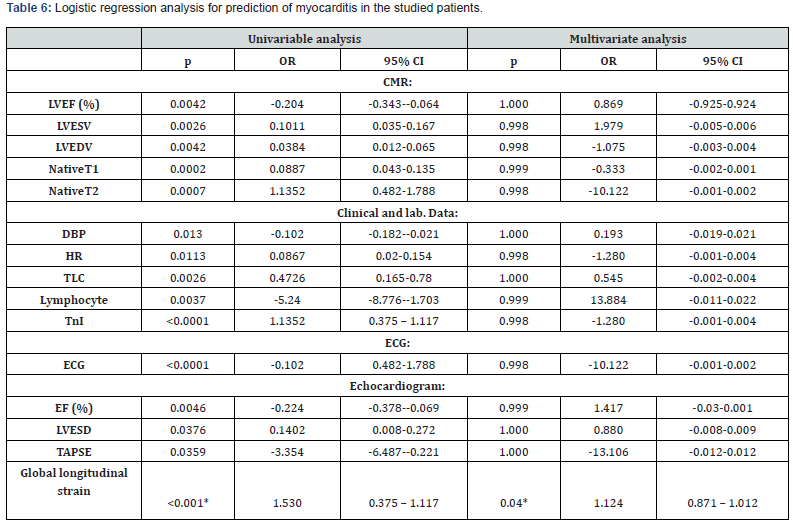
2D speckle tracking Echo parameters were used for diagnosis of myocarditis with global longitudinal strain cut-off point of >-21.33 with Sensitivity of 91.30% and Specificity of 92.59% (P <0.0001). 2D STE showed a Sensitivity of 87.50%, Specificity of 92.31% and Accuracy 90.00% for detection of myocarditis, while CMR showed a Sensitivity of 95.83%, Specificity of 96.15% and Accuracy 96.00%. Figure 1 Logistic regression analysis was conducted for the prediction of myocarditis in the studied patients. Global longitudinal strain, LVEF, LVESV, LVEDV, NativeT1, NativeT2, DBP, HR, TLC, Lymphocyte, troponin I, ECG abnormality, EF, LVESD & TAPSE were associated with the risk of myocarditis in univariate analysis. Only global longitudinal strain was associated with risk of myocarditis in both univariate and multivariate analysis Table 6.
*: significant as P-value.
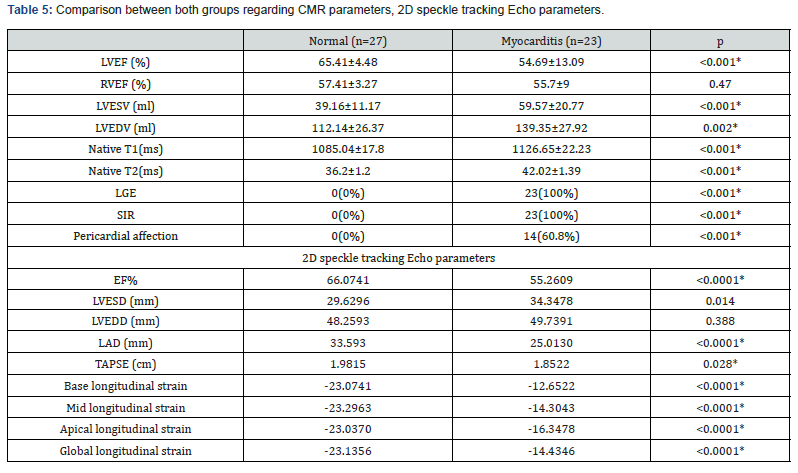
*: significant as P-value, LVEF: Left Ventricular Ejection Fraction, RVEF: Right Ventricular Ejection Fraction, LVESV: Left Ventricular End-Systolic Volume, LVEDV: Left Ventricular End-Diastolic Volume, LGE: Late Gadolinium Enhancement, SIR: Signal Intensity Ratio.
Discussion
Myocarditis is a condition that results from inflammation of the heart muscle, usually caused by a viral infection or an autoimmune disease. With the outbreak of COVID-19, reports of myocarditis cases in patients who have recovered from the virus have emerged. Given the severity of the pandemic, the early detection and treatment of myocarditis are crucial to prevent longterm cardiac damage and potential complications.
The mean age in our study group was 35.5 ± 8.24 years, this was concordant with Huang et al. [11], who studied 26 patients who recovered from covid-19 and stated that patients with a mean age of 38. In contrast Wang et al. [12], who investigated cardiac consequences of COVID-19 in 47 recovered patients using CMR, reported higher mean age as they stated that mean age of their patients was 47.6 ± 13.3 years, In our study 41(82%) were males which was consistent with Ulloa et al. [13] Who studied 57 recovered patients searching for myocardial affection in recovered patients from covid-19 with male predominance with 80% of study group were males. In contrast, Huang et al. [11] showed female predominance as only 38% of study group were males.
In our study, 28 (56%) of all studied group were smokers, 13 (26%) patients had DM and 19 (38%) had hypertension. This was comparable with Wang et al. [12] Who reported that 18% of their patients had DM and 25% of them had hypertension. In contrast Huang et al. [11] in which only 8% of patients were hypertensive and none had DM..
According to CMR parameters, 23 (46%) patients were diagnosed to have myocarditis by CMR, and patients were categorized into two groups based on these results: normal group (27 patients) & myocarditis group (23 patients).
There was no statistically significant difference between both groups regarding age, sex, BMI, SBP and MAP. Differences between the two groups were statistically significant regarding DBP, HR, TLC and lymphocytic count. In contrast, Huang et al. [11] reported that there was no statistically significant difference between patients with normal and abnormal CMR finding regarding age, sex, SBP, DBP, HR, TLC and lymphocytic count.
Our study showed statistically significant difference between both groups regarding level of Tn I as we found 11 (47%) patients with elevated Tn I in myocarditis group versus only 1 (3.7%) patient in the normal group. This was in line with Wojtowicz et al. [14] who reported statistically significant difference between the two groups of patients with and without non- ischemic cardiac injury using CMR regarding Tn I level. In the current study, there was a statistically significant difference between both groups regarding ECG abnormality as we found 12 (52%) patients with ECG abnormality in myocarditis group versus only 1 (3.7%) patient in the normal group. This was supported by a study by Ulloa et al. [13] which was conducted in Spain and studied myocardial affection in post covid-19 patient over 57 patients and showed statistically significant ECG abnormality which was found in 24 post covid patients (42%) inform of RBBB (15.8%), Atrial fibrillation (5.3%), Ventricular extrasystole (1.8%), Negative precordial T wave (12.3%) and Pathological Q wave (7%).
In our study, Echocardiographic examination showed statistically significant difference between both groups regarding EF, LVESD, TAPSE and LAD. In comparison, Özer et al. [15] who studied 74 patients with previous Covid-19 infection after 1 month from recovery reported also statistically significant difference between patients with elevated troponin group and the other group without elevated troponin regarding LAD, LVEF but no statistically significant difference between both groups regarding LVESD & LVEDD.
Our study found 21 (42%) recovered Covid-19 patients of all studied group had reduced GLS. This was in line with Mahajan et al. [16] who found reduced GLS in 40 (29.9%) recovered Covid-19 patients of his study group.
In our study, Global longitudinal strain was significantly lower in myocarditis group. Also, Base longitudinal strain, mid longitudinal strain and apical longitudinal strain. In line with our study, Mahajan et al. [16] showed statistically significant difference between reduced LV GLS group and Normal LV GLS group regarding LV GLS.
In contrast, Özer et al. [15] reported no statistically significant difference between group with myocardial injury and the other group without myocardial injury regarding LV GLS (-17.7 ± 2.6 Vs -18.9 ± 1.8, P=0.051). In our study we found 23 out of 50 (46%) patients had abnormal CMR parameters including myocardial oedema and LGE and diagnosed as myocarditis by updated Lake Louise criteria with mean time between hospital discharge and CMR examination of 34 days. This was in line with Huang et al. [5] who found median (IQR) time between COVID-19 diagnosis and CMR was 47 (36-58) days, and 15 of 26 patients (58%) reported abnormal CMR results on conventional CMR sequences.
In our study, myocarditis group were significantly different from healthy one in CMR examination regarding LVEF, LVESV, and LVEDV. But no statistically significant difference regarding RVEF. It was in concordance with Wojtowicz et al. [14] who reported statistically significant difference between the two groups of patients with and without Non-Ischemic Cardiac Injury regarding LVEF (57% vs 61%, P<.001), but no statistically significant difference regarding LVEDV and RVEF.
Our study showed increased myocardial oedema parameters with statistically significant difference between myocarditis and normal groups in form of increased T2 signal intensity ratio (T2 SIR), increased T2 relaxation time and increased native T1 respectively. In concordance to our study, Huang et al. [5] revealed that global native T1, T2, and ECV values were significantly greater in recovered COVID-19 patients with positive conventional CMR findings than in patients without positive findings (native T1 1,271 ms versus 1,237 ms, P=0.002), (T2 42.7± 3.1 ms vs 38.1± 2.4 ms, P=0.005), (ECV 28.2% vs 24.8%, P=0.001).
Also, Kunal et al. [17] reported significantly elevated native T1 (1301ms Vs 1264 ms, P =0.022) and native T2 (55.62 vs 45.25 ms, P =0.004) in post Covid-19 patients with abnormal CMR group compared to the other one with normal CMR.
In our study, non-ischemic pattern of LGE was found in 23 patients (46%) mainly sub- epicardial and mid wall enhancement affecting the apical and mid cardiac muscle segments with P value <0.001, denoting presence of myocardial fibrosis and/or necrosis. Wang et al. [12] reported non-ischemic sub-epicardial and mid wall LGE in 13 of 44 (30%) of the post-COVID- 19 patients’ group (a finding similar to our cohort results). Then they performed a strain study revealing that patients with LGE exhibited poorer LV and RV Performance.
In our study, Pericardial involvement in form of pericardial effusion and pericardial LGE which develops as a consequence of myocardial damage, was also found in 14 patients (28%) of all studied patients and was found in 60% of myocarditis group. In concordance, Huang et al. [5] reported that 7 (28%) of 26 patients were positive for pericardial LGE and have a minor pericardial effusion.
Regarding the validity of 2D speckle tracking Echocardiography (STE) and CMR in final diagnosis of myocarditis, In previous study by Luetkens et al. [18] found that the diagnosis of myocarditis using Updated Lake Louise Criteria yielded a sensitivity of 87.5% and a specificity of 96.2%.
In our study, speckle tracking echocardiography showed a sensitivity of 87.5% and specificity of 92.3 %. A study by Sharifkazemi et al. [19] compared the diagnostic performance of CMR and 2D STE in 57 patients with suspected acute myocarditis. They found that CMR had a higher sensitivity (96.8%) and specificity (93.5%) compared to 2D speckle tracking Echo (78.4% and 77.4%, respectively) in the diagnosis of acute myocarditis. In our study logistic regression analysis showed that only global longitudinal strain was associated with risk of myocarditis in both univariate and multivariate analysis.
Finally, this study had some limitations, as study did not include long-term follow-up to assess the outcomes of patients with myocarditis. Also, the study did not provide detailed information on the severity of COVID-19 in the patients, which may have influenced the development of myocarditis.
Case Presentations
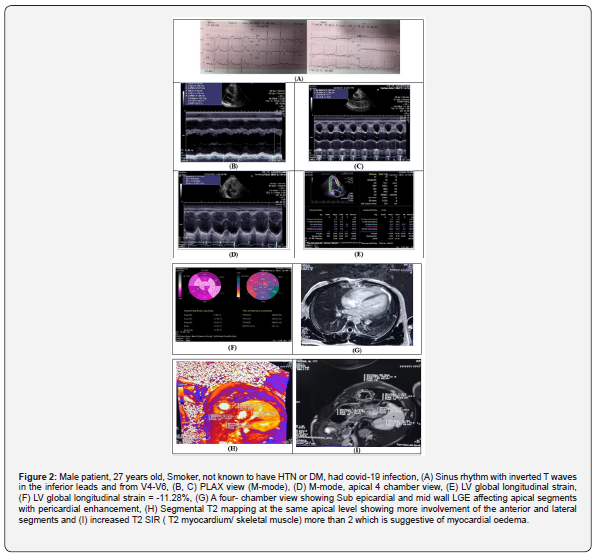
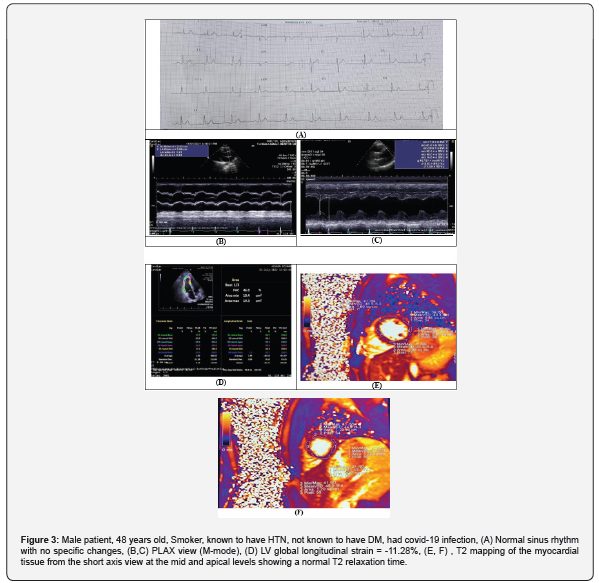
Case 1: Figure 2. Case 2: Figure 3.
Conclusion
Evidence of myocarditis in asymptomatic patient recovered from COVID-19 was present in 46% of patients. Non-invasive predictors of myocarditis are Global longitudinal strain, LVEF, LVESV, LVEDV, NativeT1, NativeT2, DBP, HR, TLC, Lymphocyte, TnI, ECG abnormality, EF, LVESD and TAPSE while Global longitudinal strain was the only independent predictor. According to this research’s findings, it can be concluded that CMR is a valuable tool in the early detection of myocarditis in those who have achieved recovery from COVID-19. The use of CMR in combination with 2D STE has shown a notable level of accuracy in the detection and assessment of myocarditis. The findings of this study showed that there were significant differences between patients with suspected myocarditis and those with normal results on both 2D STE and CMR. The results also showed that CMR had higher sensitivity, specificity, and accuracy compared to 2D STE in the diagnosis of myocarditis. Further studies with larger sample sizes and multi-center cooperation are needed to validate the diagnostic accuracy of CMR and 2D STE in the early detection of myocarditis in patients recovered from COVID- 19.
References
- Castiello T, Georgiopoulos G, Finocchiaro G, Claudia M, Gianatti A, et al. (2022) COVID-19 and myocarditis: a systematic review and overview of current challenges. Heart Fail Rev 27(1): 251-261.
- Baloch S, Baloch MA, Zheng T, Pei X (2020) The Coronavirus Disease 2019 (COVID-19) Pandemic. Tohoku J Exp Med 250(4): 271-278.
- Shi Y, Wang Y, Shao C, Huang J, Gan J, Huang X, et al. (2020) COVID-19 infection: the perspectives on immune responses. Cell Death Differ 27(5): 1451-1454.
- Patel VB, Basu R, Oudit GY (2016) ACE2/Ang 1-7 axis: A critical regulator of epicardial adipose tissue inflammation and cardiac dysfunction in obesity. Adipocyte 5(3): 306-311.
- Huang C, Wang Y, Li X, Ren L, Zhao J, et al. (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, Lancet 395(10223): 497-506.
- Wang G, Zhang Y, Zhao J, Zhang J, Jiang F (2020) Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet 395(10228): 945-947.
- Guzik TJ, Mohiddin SA, Dimarco A, Patel V, Savvatis K, et al. (2020) COVID- 19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res 116(10): 1666-1687.
- Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, et al. (2020) Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol 5(11): 1265-1273.
- Nchimi A (2017) The EACVI Echo Handbook. European Heart Journal 38(1): p. 13.
- Peacock J, Peacock P (2010) Oxford Handbook of Medical Statistics: Oxford University Press 01 Jun
- Huang S, Wang J, Liu F, Liu J, Cao G, Yang C, et (2020) COVID-19 patients with hypertension have more severe disease: a multicenter retrospective observational study. Hypertens Res 43(8): 824-831.
- Wang H, Li R, Zhou Z, Jiang H, Yan Z, et al. (2021) Cardiac involvement in COVID-19 patients: mid-term follow up by cardiovascular magnetic J Cardiovasc Magn Reason 23(1): 14.
- Urmeneta Ulloa J, Martínez de Vega V, Salvador Montañés O, Álvarez Vázquez A, Sánchez-Enrique C, et al. (2021) Cardiac magnetic resonance in recovering COVID-19 patients. Feature tracking and mapping analysis to detect persistent myocardial involvement. Int J Cardiol Heart Vasc 36: 100854.
- Wojtowicz D, Dorniak K, Ławrynowicz M, Wąż P, Fijałkowska J, et al. (2022) Cardiac Magnetic Resonance Findings in Patients Recovered from COVID-19 Pneumonia and Presenting with Persistent Cardiac Symptoms: The TRICITY-CMR Biology (Basel) 11(12): 1848.
- Özer S, Candan L, Özyıldız AG, Turan OE (2021) Evaluation of left ventricular global functions with speckle tracking echocardiography in patients recovered from COVID-19. Int J Cardiovasc Imaging 37(7): 2227-2233.
- Mahajan S, Kunal S, Shah B, Garg S, Palleda GM, et al. (2021) Left ventricular global longitudinal strain in COVID-19 recovered patients. Echocardiography 38(10): 1722-1730.
- Kunal S, Bagarhatta P, Palleda GM, Bansal A, Batra V, et al. (2022) Role of cardiovascular magnetic resonance imaging in COVID-19 recovered patients: A short-term follow-up Echocardiography 39(11): 1401-1411.
- Luetkens JA, Faron A, Isaak A, Dabir D, Kuetting D, et (2019) Comparison of Original and 2018 Lake Louise Criteria for Diagnosis of Acute Myocarditis: Results of a Validation Cohort. Radiol Cardiothorac Imaging 1(3): e190010.
- Sharifkazemi M, Rezaian G, Lotfi M (2023) Evaluation of myocardial performance by serial speckle tracking echocardiography in diagnosis and follow-up of a patient with eosinophilic myocarditis. Echo Res Pract 10: 1.






























