A Challenging Case of Mitral Stenosis in an Octogenarian Treated by Balloon Valvuloplasty
Akshay Ashok Bafna* and Kuldeep Totawar
Department of Cardiology, RCSM, CPRH, GMC, Kolhapur, India
Submission: December 08, 2022; Published: February 06, 2023
*Corresponding author: Akshay Ashok Bafna, Cardiologist, Department of Cardiology, RCSM, CPRH, GMC, Kolhapur, Maharashtra, India
How to cite this article: Akshay Ashok Bafna, Kuldeep Totawar. A Challenging Case of Mitral Stenosis in an Octogenarian Treated by Balloon Valvuloplasty. J Cardiol & Cardiovasc Ther. 2023; 18(2): 555984. DOI: 10.19080/JOCCT.2023.18.555984
Abstract
Balloon Mitral Valvuloplasty (BMV) has been the primary treatment for severe and or hemodynamically significant mitral stenosis. It was first introduced in 1984 and has become an accepted method for treating mitral stenosis. It produces excellent results in patients with noncalcified mitral valves. BMV is the best procedure to treat these patients including the elderly and those with pulmonary hypertension. This case report highlights the sequential changes in the trans mitral gradient before and after a successful BMV in an octogenarian.
Keywords: Balloon Mitral Valvuloplasty; Mitral Valve; Mitral Stenosis; Chronic Rheumatic Valve Disease; Elderly
Introduction
Mitral Valve is the most commonly affected valve in rheumatic heart disease. Mitral stenosis is a commonly seen problem as sequelae of rheumatic fever. It typically manifests in the second to fourth decades of life [1]. Even though the severity and incidence of this disease have significantly come down in developed nations, the disease is still seen frequently in developing countries of the world making it a major public health issue [2]. Elderly patients who have had a surgical valvotomy when presenting again with restenosis pose an additional challenge. These patients often have additional co-morbidities which makes them high risk for repeat cardiac surgery. Balloon Mitral Valvoplasty done percutaneously (PBMV) is an accepted method to treat it in symptomatic patients with severe mitral stenosis (MS) [2]. This case report highlights the echocardiographic and clinical results of BMV in an octogenarian.
Case Report
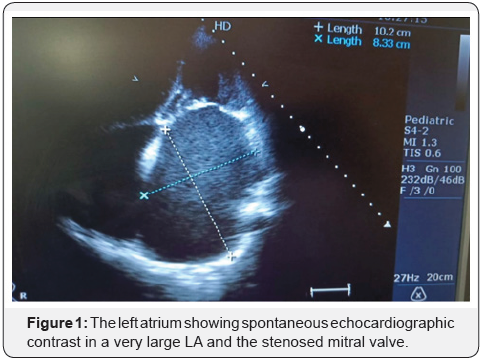
A female aged 86 years with a weight of 30 kgs and a height of 141cm (BMI =15.1) was diagnosed with severe MS (MVA =1.0/1.1cm2, MVG 20/14 mmhg) and (MVS/Wilkins) 3/2/2/3 score with mild mitral regurgitation (MR), with a very large (10.3 cms) left atrium (LA) and grade III spontaneous echocardiographic contrast (SEC) (Figure 1). The normal mitral valve area (MVA) is about 4-6 cm. When this area becomes less than 2 cm the stenosis starts becoming significant. A valve area below 1 cm makes it a critical MS. The pressure difference between the left atrial pressure and the end-diastolic pressure of the left ventricle is the gradient across the mitral valve. This gradient increases with an increase in the heart rate because diastole is shortened than the systole [3]. Wilkins scoring system evaluates leaflet thickening, mobility, calcification, and sub valvular involvement on a scale of 0-4 [4]. SEC indicates blood stasis in cardiac chambers and major vessels and is a known precursor of thrombus formation [5]. The patient had recurrent admission for acute decompensation, later she had paroxysmal atrial fibrillation.
After noting all the above factors, it was decided to proceed with percutaneous balloon mitral valvotomy.
The challenges of this case are:
i. Advanced age, fragile, 30 kg female
ii. An old case of esophageal stricture for which recurrent esophageal balloon dilatation was done hence TEE was contraindicated
iii. Giant LA as noted with a size of 10.3 cms
iv. SEC grade III but with no obvious visualized LAA clot in transthoracic echo
v. Spina issue with bent legs making positioning on the cath table difficult
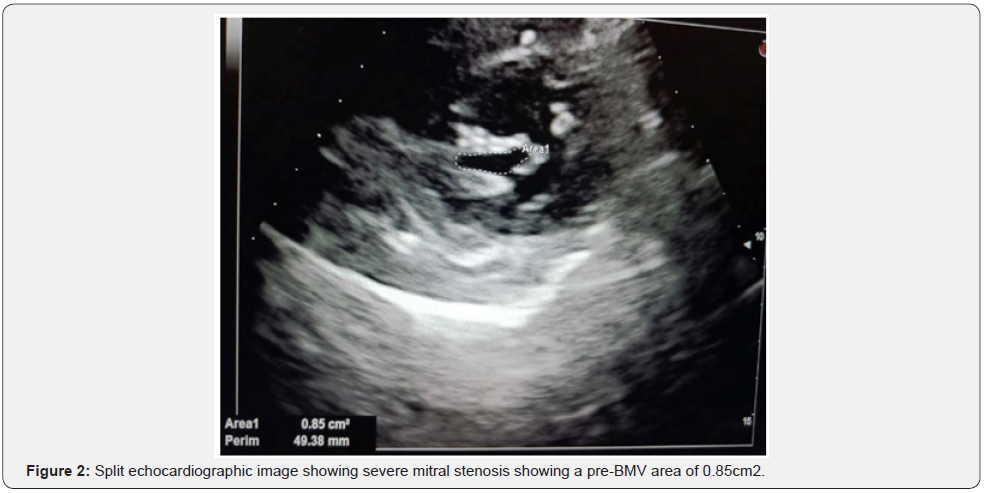
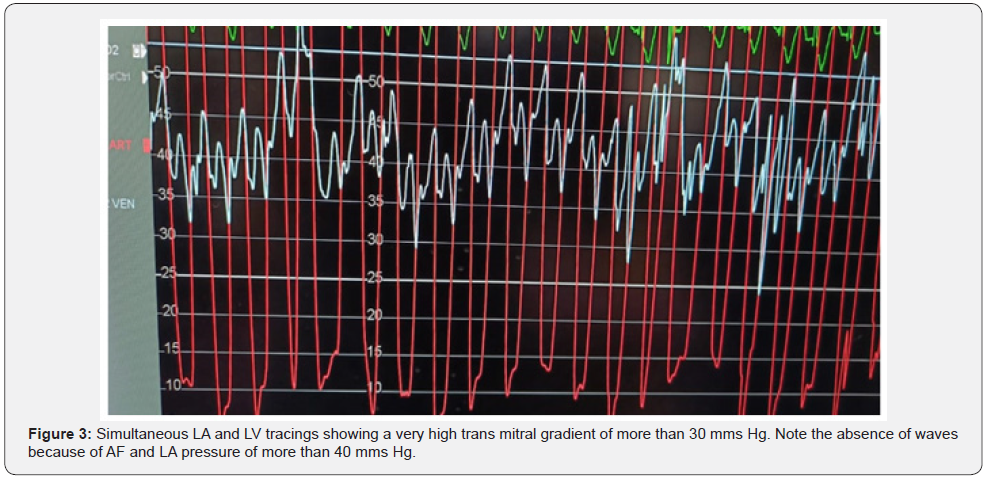
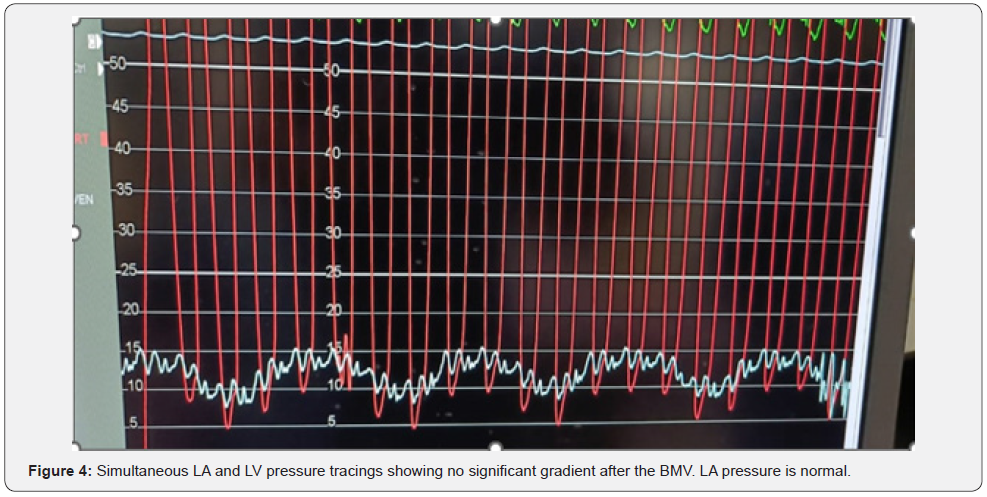
She was diagnosed with severe MS and a valve area of 0.85cm2 and after BMV valve area increased to1.5 cm with the commissures completely split and the patient was discharged on day 3 of post-BMV (Figure 2). The gradient across the mitral valve which was 32mms Hg came down to 2-3 mms Hg immediately after the procedure (Figure 3). The mean pulmonary artery pressure before BMV was 58 mmsHg, which came down to 32 mmhg. LA pressure before BMV was 42/26 mmHg and post BMV was 18/07 mmHg (Figure 4). There was minimal mitral regurgitation and no significant aortic valve disease. There was no vegetation or a clot seen on the transthoracic echocardiography. The left ventricular function was normal.
Discussion
BMV is an established non-surgical method of treating MS [4]. The results in elderly patients can frequently be sub-optimal because of the adverse anatomy with sub valvular disease, AF makes the LA very large making septal puncture difficult. The case shown in this report despite advanced age and several comorbidities had an excellent result of the BMV. The complications in such cases can be because of inadvertent perforation of the LA during the mal aligned inter atrial septum septal, embolism because trans thoracic echocardiography could have missed a LA clot. Stroke can be the commonest embolic complication encountered. There was no significant post-BMV mitral regurgitation. The elevated pulmonary pressures normalize in most such cases after BMV because of no permanent changes in the pulmonary vasculature. This was also seen in our patient.
The results in octogenarians are less impressive as compared to younger patients, because of the frequent presence of comorbidities in the very elderly. Although death is rare but patients can get complications like stroke, cardiac tamponade, emergency mitral valve replacement, or myocardial infarction, up to 10% [6- 9].
Conclusion
Chronic Rheumatic Heart Disease is seen frequently in the ages of 30-50 but when detected in octogenarians who become symptomatic it can be challenging because of comorbidities. Non-surgical procedures like BMV are the most accepted method of treatment. It does not need any general anesthesia, postprocedural ventilation, and very short hospitalization. Although this patient had a very good result even a sub-optimal result with a modest increase in valve area can be extremely palliative.
The case exemplifies that age is no bar for getting an optimal result for patients of severely symptomatic patients with rheumatic MS. The results however depend upon the morphology of the valve at all ages.
References
- Shaw TRD, Elder AT, Flapan AD (1991) Mitral Balloon Valvuloplasty for Patients Aged over 70 Years: An Alternative to Surgical Treatment. Age Ageing 20(4): 299-303.
- Sharaf M, Abodahab LH, Bahaa M (2017) Percutaneous Balloon Mitral Valvuloplasty in the Elderly. J Struct Heart Dis 3(2): 35-42.
- Omran AS, Arif AA, Mohamed AA (2010) Echocardiography in mitral stenosis. J Saudi Heart Assoc 23(1): 51-58.
- Soliman OII, Anwar AM, Metawei AK, Jackie S McGhie, Marcel L Geleijnse (2011) New Scores for the Assessment of Mitral Stenosis Using Real-Time Three-Dimensional Echocardiography. Curr Cardiovasc Imaging Rep 4(5): 370-377.
- Ito T, Susa M (2019) Left atrial spontaneous echo contrast: relationship with clinical and echocardiographic parameters. Echo Res Pract 6(2): 65-73.
- Tuzcu EM, Block PC, Griffin BP, Newell JB, I F Palacios IF (1992) Immediate and Long-term Outcome of Percutaneous Mitral Valvotomy in Patients 65 Years and Older. Circulation 85(3): 963-971.
- Palacios IF, Tuzcu ME, Weyman AE, Newell JB, Block PC (1995) Clinical follow-up of patients undergoing percutaneous mitral balloon valvotomy. Circulation 91(3): 671-676.
- Lung B, Cormier B, Farah B, Nallet O, Porte JM, et al. (1995) Percutaneous mitral commissurotomy in the elderly patients with mitral stenosis. Eur Heart J 16(8): 1092-1099.
- Sanati H, Firoozi A (2017) Percutaneous Balloon Mitral Valvuloplasty.






























