A Rapid-Deployment Valve Implantation in A Complex Chronic Type A Dissection Reoperation
Alper Öner1, Catharina Neßelmann2, Ashraf A Abdallah2, Hüseyin Ince1 and Pascal M Dohmen2,3*
1Department of Cardiology, Heart Centre Rostock, University of Rostock, Rostock, Germany
2Department of Cardiac Surgery, Heart Centre Rostock, University of Rostock, Rostock, Germany
3Department of Cardiothoracic Surgery Faculty of Health Sciences University of the Free State, Bloemfontein, South Africa
Submission: January 18, 2023;Published: January 31, 2023
*Corresponding author: Pascal M Dohmen, Department of Cardiac Surgery, Heart Center Rostock, University of Rostock, Schillingallee 35, Rostock D-18057, Germany
How to cite this article:Alper Ö Catharina N, Ashraf A A, Hüseyin I, Pascal M D. A Rapid-Deployment Valve Implantation in A Complex Chronic Type A Dissection Reoperation. J Cardiol & Cardiovasc Ther. 2023; 18(2): 555983. DOI: 10.19080/JOCCT.2023.18.555983
Abstract
We present a 59-year-old female patient suffering from recurrent chest pain after acute Stanford type A aortic dissection (TAAD) with previously limited ascending aortic replacement and partial aortic root remodeling. Today, the angiography shows a residual TAAD of the ascending aorta and moderate aortic valve regurgitation. During urgent redo surgery a re-ascending, including arch replacement and frozen elephant trunk was performed, and a rapid-deployment valve system was used for aortic valve treatment. The postoperative course was uneventful and the patient could be discharged on postoperative day 14. At six months follow-up, the patient was completely stable, without recurrent cardiac symptoms.
Introduction
Acute Stanford type A aortic dissection (TAAD) is a devastating and life-threatening disease, with an incidence of 5 to 30 cases per 1 million patients per year [1]. Pre-hospital mortality is between 18-49%, upon hospital arrival 1-2% per hour, with a total mortality of 30-68% within the first 48 hours [2]. Surgical treatment is unavoidable, however the therapeutic strategy of TAAD is still controversy. Some surgeon prefer a limited approach by ascending or hemi-arch replacement and other total treatment of the complete thoracic aorta including using a frozen elephant trunk [3]. If the aortic valve is involved, aortic valve treatment is needed and generally valve repair preferred. We present a case with chronic TAAD, in which the partial root remodeling technique on the non-coronary sinus and limited ascending aorta replacement was performed initially during the acute phase.
Case Report
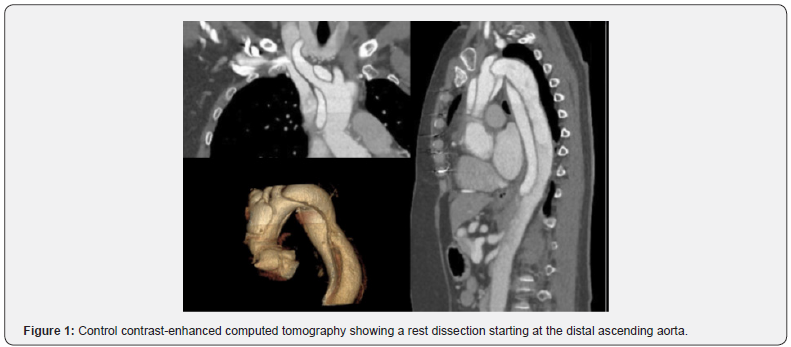
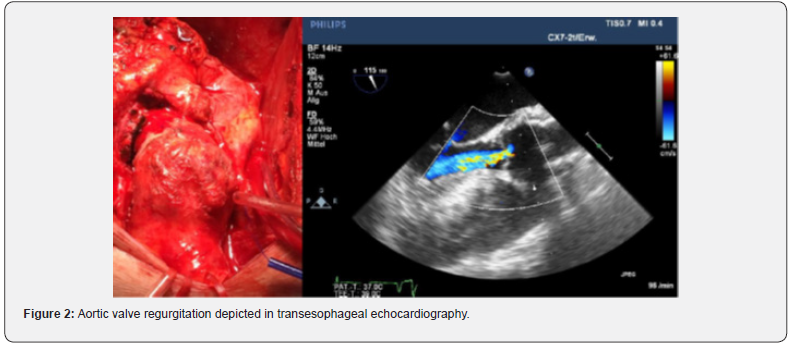
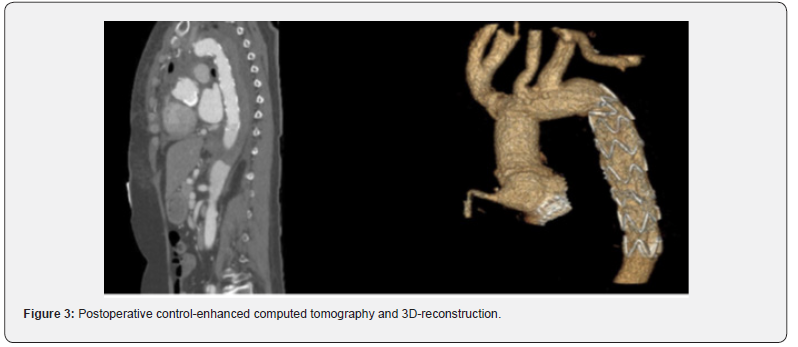
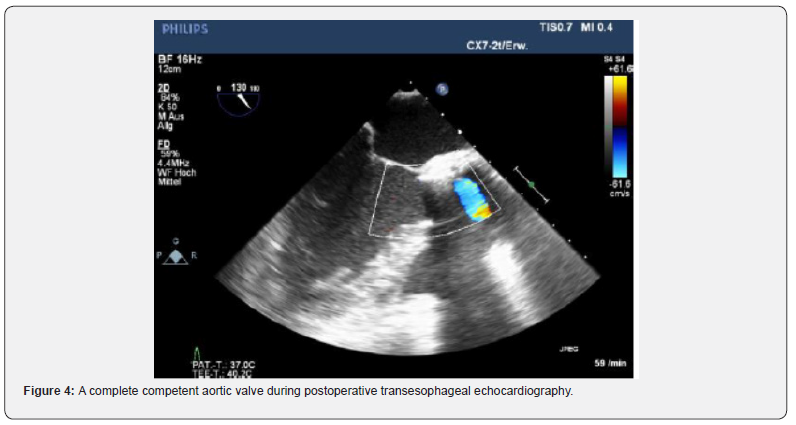
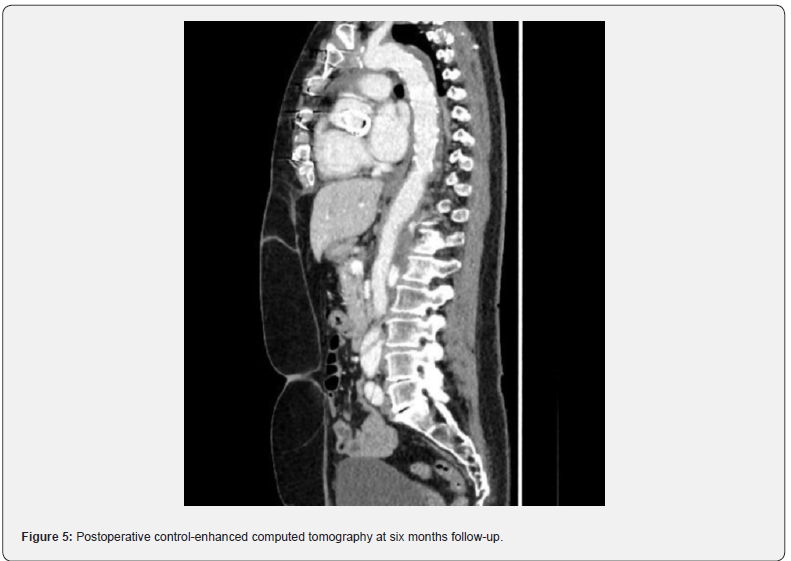
A 59-year-old female patient suffering from recurrent chest pain after acute Stanford Type A aortic dissection (TAAD) presented at our outpatient clinic. Four months prior to this consultation, the patient underwent emergency surgery with aortic root remodeling and replacement of the ascending aorta in deep-hypothermic arrest at another centre. The postoperative period was complicated by pulmonary insufficiency with prolonged ventilation. At the present visit in our department, a control contrast-enhanced computed tomography was performed showing a rest dissection starting at the distal ascending aorta was seen (Figure 1). Additionally a moderate aortic valve regurgitation was seen at transesophageal echocardiography (Figure 2). The patient was urgent taken to the operating theatre for complete open repair. Cardiopulmonary bypass was initiated by re-cannulation of the right axillary artery and the right femoral vein. Hypothermic circulatory arrest at 17.7°C was instituted for implantation of a frozen elephant trunk (E-vita OPEN PLUS Hybrid Stentgraft System 24mm with a stentgraft length of 130mm; Jotec GmbH, Hechingen, Germany), arch replacement and replacement of the aortic valve using a rapid-deployment valve system (23mm) after removing the native aortic valve leaflets. Antegrade brain perfusion was performed for 42 minutes and cross-clamp time was 93 minutes. The postoperative course was uneventful and respirator weaning was achieved within 5 hours. On postoperative day 2, the patient was transferred to the general ward. The patient was discharged home on postoperative day 14 showing excellent aortic valve function, without regurgitation and optimal aortic repair (Figure 3,4). On 6 months follow-up these data could be confirmed (Figure 5).
Comment
Chronic Stanford type A aortic dissection has been defined in the guidelines of 2014 as those TAAD over 90 days [4]. In the setting of a prior surgery for an acute TAAD persistent dissection of the ascending aorta was a rare finding.
Rapid deployment valve system was initially implemented in the therapy of isolated aortic stenosis as an alternative to transcatheter aortic valve implantation with the advantage of surgical inspection and removal of degenerated, calcified aortic valves. Compared to surgical aortic valve replacement, rapid deployment valves offer shortened aortic cross-clamp time and shorter duration of cardiopulmonary bypass. Today indications were extended to concomitant procedures or endocarditis and advantages such as the use of larger prostheses resulting in lower transvalvular gradients and higher indexed effective area have resulted in broad application of these prostheses [5,6]. Although some conflicting data exist in terms of perioperative stroke, need for permanent pacemaker implantation, and mean pressure gradients none of these were observed in our patient but favourable CPB and cross-clamp times were achieved.
Aortic regurgitation as an indication for rapid deployment prostheses is rare and there is only limited data on this indication especially in the setting of redo aortic root surgery such as case studies. Additionally experience with transcatheter aortic valves as an off-label use for pure aortic insufficiency showed no difference in in-hospital mortality compared to surgical aortic valve replacement after 2 years in an analysis of 14.720 patients from National Inpatient Sample database [7].
Reported hospital mortality for operation of the aortic root following previous surgery of the aortic root ranges between 0 and 12% [8] and these procedures undoubtedly are technically demanding. Partial root remodelling is employed in some centres for treating root involvement in aortic dissection with the intimal tear extending into the noncoronary sinus or additionally to the right coronary sinuses only [9]. Haung and colleagues reported a rate of re-operation of the aortic valve after partial aortic root remodelling of 8.6 % after 36.4 ± 31.6 months in a single-centre study of 40 patients [9].
In conclusion this case report highlights the importance of including all recent technologies into the surgical armamentarium in order to provide best practice and achieve strong results to the individual needs of patients. Rapid deployment prostheses showed excellent function in the reported redo surgery of the root and ascending aorta after initial partial root replacement and aortic ascending replacement.
References
- Mokashi SA, Svensson LG (2019) Guidelines for the management of thoracic aortic disease in 2017. Gen Thorac Cardiovasc Surg 67(1): 59-65.
- Gudbjartsson T, Ahlsson A, Geirsson A, Gunn J, Hjortdal V, et al. (2020) Acute type A aortic dissection - a review. Scand Cardiovasc J 54(1): 1-13.
- Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, et al. (2014) 2014 ESC guidelines on the diagnosis and treatment of aortic diseases. Eur Heart J 35(41): 2873-2926.
- Di Esanio M, Berretta P (2020) The sutureless and rapid-deployment aortic valve replacement international registry: lessons learned from more than 4,500 patients. Ann Cardiothorac Surg 9(4): 289-297.
- Rahmanian PB, Kaya S, Eghbalzadeh K, Menghesha H, Madershahian N, et al. (2018) Rapid Deployment Aortic Valve Replacement: Excellent Results and Increased Effective Orifice Areas. Ann Thorac Surg 105(1): 24-30.
- Öner A, Hemmer C, Alozie A, Löser B, Dohmen PM (2022) Introduction of the rapid deployment aortic valve system use in elderly patients with endocarditis. Front Cardiovasc Med 9: 774189.
- Alharbi AA, Khan MZ, Osman M, Khan MU, Munir MB, et al. (2020) Transcatheter Aortic Valve Replacement vs Surgical Replacement in Patients With Pure Aortic Insufficiency. Mayo Clin Proc 95(12): 2655-2664.
- Jassar AS, Desai ND, Kobrin D, Pochettino A, Vallabhajosyula P, et al. (2015) Outcomes of aortic root replacement after previous aortic root replacement: the "true" redo root. Ann Thorac Surg 99(5):1601-8; discussion 1608-1609.
- Huang F, Li L, Qin W, Su C, Wang L, et al. (2016) Partial aortic root remodeling for root reconstruction in patients with acute type A dissection. J Biomed Res 30(5): 411-418.






























