Acute Myocarditis Complicated by a Huge Intra-VG Thrombus Responding Well to Corticosteroid Therapy: Report of a Case
Brahim Nassour Aware*, Asma Zouad, Imane Tlohi, Salim Arouss, Ghali Bennouna, Leila Azzouzi, Abdel Nasser Drighil and Rachida Habbal
Department of Cardiology, CHU IBN ROCHD of Casablanca, Morocco
Submission: December 19, 2022; Published: January 11, 2023
*Corresponding author: Brahim Nassour Aware, Department of Cardiology, CHU IBN ROCHD of Casablanca, Morocco
How to cite this article: Brahim N A, Asma Z, Imane T, Salim A, Ghali B, et al. Acute Myocarditis Complicated by a Huge Intra-VG Thrombus Responding Well to Corticosteroid Therapy: Report of a Case. J Cardiol & Cardiovasc Ther. 2023; 18(2): 555981. DOI: 10.19080/JOCCT.2023.18.555981
Abstract
Background: Myocarditis is a disease defined by the presence of myocardial inflammatory infiltrates associated with myocyte necrosis of non-ischaemic origin. Diagnosis is based on clinical presentation, cardiac MRI and myocardial biopsy. Acute myocarditis may be secondary to infectious, toxic or allergic cardiac disease or may be associated with a systemic disease.
Case report: We report here the case of a young male patient who was admitted with febrile de novo acute heart failure which revealed acute myocarditis complicated by a giant intra-VG thrombus which recovered well on corticosteroid therapy.
Conclusion: Myocarditis is pathology with very diverse clinical, histological and evolutionary forms.
Keywords: Myocarditis; Thrombus; Corticotherapy
Background
Myocarditis is a disease defined by the presence of myocardial inflammatory infiltrates associated with myocyte necrosis of non-ischaemic origin [1]. The fulminant form of the disease is defined by a rapid progression to cardiogenic shock. In autopsy series of sudden deaths in young people, histological signs of myocarditis are found in 10 to 42% of cases [2], making it one of the main causes of sudden death in young people, along with hypertrophic or dilated cardiomyopathy, coronary birth defects, arhythmogenic right ventricular dysplasia and ductal disease [3]. Diagnosis is based on clinical presentation, cardiac MRI and myocardial biopsy. Acute myocarditis may be secondary to infectious, toxic, or allergic cardiac injury or associated with a systemic disease. The emergence of the SARS-CoV-2 virus responsible for COVID-19 disease with poly visceral involvement, the first of which is cardiac involvement. This cardiac involvement can take the form of acute myocarditis. We report here the case of a young male patient who was admitted with acute de novo febrile heart failure which revealed acute myocarditis complicated by a giant intra-VG thrombus which recovered well under corticosteroid therapy.
Case Presentation
We report here a 29 years old patient who is a smoker and has a poor lifestyle and socioeconomic status, with a history of substance abuse. He presented with sudden onset of dyspnoea preceded by an influenza-like syndrome consisting of night-time fever, physical asthenia and headache with dry cough. The clinical examination on admission noted dyspnoea stage IV of the NYHA without chest pain, a dry cough and a feeling of fever with physical asthenia as functional signs. The physical examination revealed a blood pressure of 98/65 mmHg, heart rate of 120 bpm and signs of heart failure with crackling in the mid-fields and discrete oedema of the lower limbs rising to the mid-leg with spontaneous turgidity of the jugular veins. The ECG showed a sinus tachycardia at 125 bpm without any re-polarisation disorder. Biologically, there was a slight hyperleukocytosis with a slight lymphopenia, a CRP of 21 mg and a negative ESR; Troponin was positive at 300 ng/l; immunological work-up was negative, HIV, Hepatitis, EBV, Hemophilus Influenza and Siphilis serologies came back negative, a covid PCR came back positive contrasting with a strongly positive IgG serology at 270 IU for a normal of less than 30 IU. The other serologies, notably Coxakies, Parvovirus B19 are not feasible in our structure.
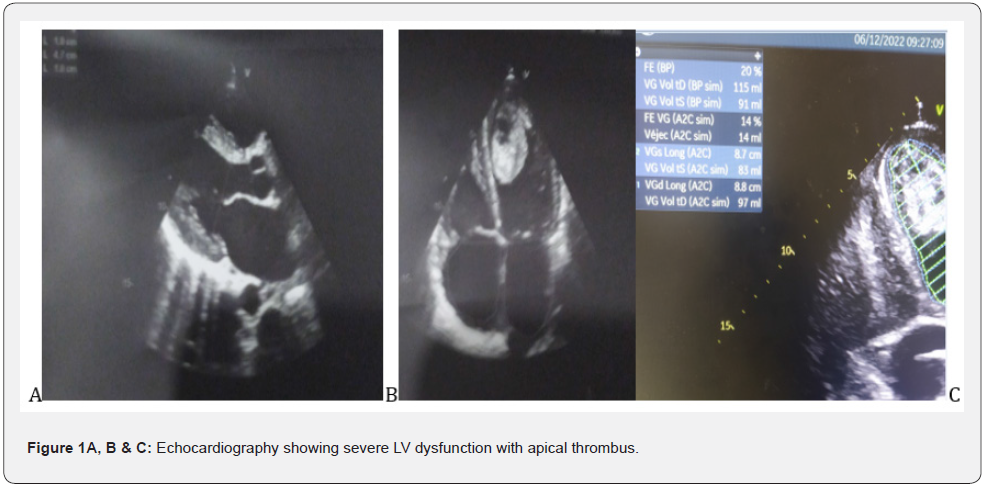
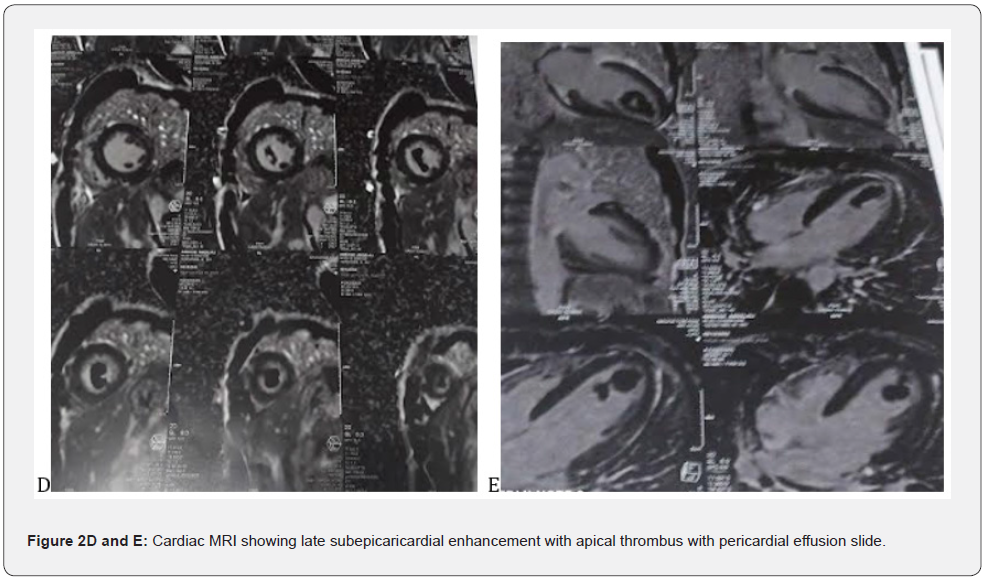
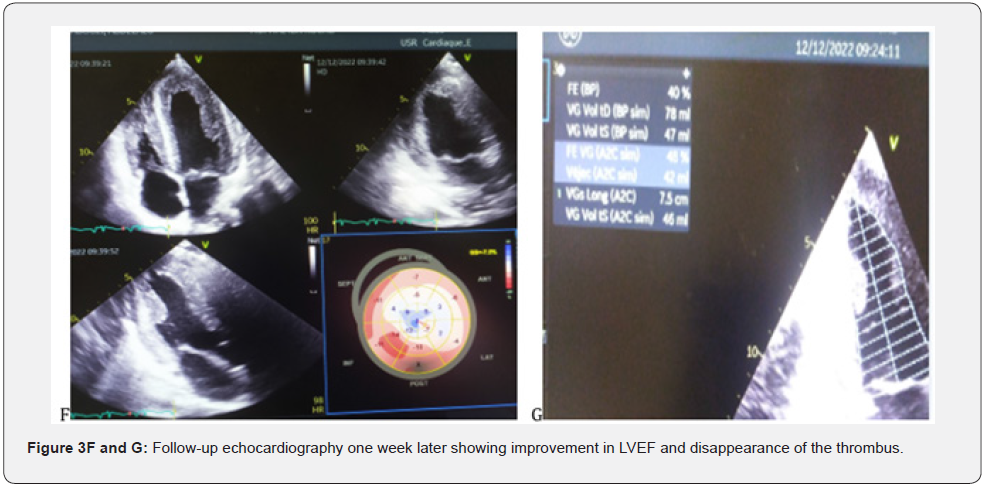
Echocardiography showed a non-dilated, slightly hypertrophied LV with severe dysfunction and 20% EF, with a huge mobile thrombus measuring 42 x 23 mm in the LV, no significant mitro-aortic valve disease.The MRI scan showed a late subpericardial enhancement in severe bi ventricular dysfunction with a huge mobile intra LV thrombus suggesting acute myocarditis. The patient was put on strict rest and an IV diuretic treatment with monitoring of the diuresis, an effective anti-coagulation, a bolus of solumedrole 120 mg over 3 days and per-os relay of 60 mg with progressive degression. The evolution was marked by a clear regression of the congestive signs, an improvement of the general state of the patient over 7 days and a recovery of the EF to 40% vs 20 at admission. A disruption of the thrombus after 7 days of anti-coagulation with a minimal migration giving a light splenic and hepatic infarction without significant clinical repercussions. The patient was discharged after 12 days in hospital on Coversyl 5 mg/d; Cardensiel 2.5 mg/d; Sintrom 7.5 mg/d and Solupred 60 mg/d with a 3 month tapering programme.
Discussion
Myocarditis is an inflammatory disease of the myocardium defined by the Dallas histological criteria. Diagnosis requires the demonstration of a predominantly lymphocytic myocardial inflammatory infiltrate defined by the presence of >14 leukocytes/mm3 including more than 4 monocytes > mm3 and 7 CD3+ T lymphocytes/mm3, associated with myocyte necrosis of non-ischaemic origin [4]. The pathophysiological hypotheses are variable and include both cell lysis related to direct viral toxicity, and inflammatory phenomena related to the activation of the innate immune response (production of pro-inflammatory cytokines) and then specific cellular response [5- 6]. In certain situations, this activation may be excessive and lead to significant destruction of the cardiomyocytes, causing left ventricular dysfunction as seen in our patient, which can evolve into a state of cardiogenic shock if not managed immediately, which worsens mortality in the most severe forms (fulminant myocarditis). In all cases, this cardiomyocyte necrosis is responsible for the elevation of troponin, as confirmed in our patient with troponin levels of 300 mg, which is a key element in the diagnostic suspicion without any electrical sign of myocardial suffering of ischaemic origin [7]. The clinical phenotype of myocarditis is very polymorphic, which makes its positive diagnosis difficult; the diagnosis is suspected in the presence of clinical symptoms associated with an elevation of the tropo-nine and possibly inflammatory markers. The picture of acute heart failure corresponds to the appearance of signs of heart failure over a period of less than two weeks. This picture of fulminant myocarditis is often preceded a few days before by an influenza-like episode, which is consistent with our presentation where we find a history of influenza-like illness favoured by an unfavourable socio-economic level in our third world countries. The left ventricular dysfunction can be severe and responsible for shock because of diogenesis. Echocardiography usually shows a non-dilated, hypertrophied left ventricle (in relation to myocardial oedema) in our patient we find a slight hypertrophy at 10 mm of the wall and 10 mm of the IVS (Figure 1 A & B) with altered systolic function [8] as well as severe LV dysfunction in our patient with an EF of 20% (Figure 1C). Myocardial magnetic resonance imaging (MRI) has become an indispensable non-invasive examination in the management and follow-up of myocarditis (Figure 1D & E). The diagnosis of myocarditis is based on the presence of two of the following three Lake Louise criteria [9] : Myocardial hyperhaemia, demonstrated by early global gadolinium enhancement of the myocardium in a T1-weighted sequence; regional or global myocardial oedema, demonstrated by hyper signal in a T2- weighted sequence; myocardial necrosis or fibrosis, most often multifocal, in the pericardium, as seen in the images of our patients (Figure 3 F and G), demonstrated by late gadolinium enhancement in a T1-weighted sequence. The presence of a pericardial effusion is an additional argument for the diagnosis of myocarditis which further supports the diagnosis in our patient with the pericardial effusion slide found on MRI. For the treatment in the general case, the recommendations of the ESC are to propose in first intention a symptomatic treatment of the cardiac insufficiency by the diuretic for the decongestion; the IEC and beta blockers for their effects anti-remodelling. Studies concerning the curative treatment of myocarditis mainly concern chronic forms, which are known to have an unfavourable evolution in the medium and long term, with progressive degradation of cardiac function. The diagnosis is then made during biopsies carried out in the context of recently discovered dilated cardiomyopathy. Various immunosuppressive treatments (prednisolone, cyclosporine, cyclophosphamide) have been tried in myocarditis. In a recent prospective randomised double-blind study comparing placebo versus prednisone and azathioprine in 85 patients with non-viral chronic lymphocytic myocarditis who had symptoms of heart failure for more than six months despite conventional medical treatment (TIMIC Study), In the TIMIC Study, an improvement in left ventricular ejection fraction (LVEF) and a reduction in left ventricular enddiastolic volume were found in 88% of the 43 patients treated, whereas cardiac function deteriorated in 83% of the 42 patients who received placebo [10-12]. In the light of these studies, we recommended that patients be treated with bolus corticosteroids (solumedrole 120) as an adjuvant to the corticosteroids, and we noted a favourable evolution under treatment with a good clinical and echocardiographic improvement (Figure 3 F and G).
Conclusion
Myocarditis is a pathology with very diverse clinical, histological and evolutionary forms that must be characterized as best as possible with the help of the clinical history, echocardiography, cardiac MRI and the results of end-myocardial biopsies. In acute and chronic myocarditis, immunosuppressive or immunomodulatory treatments, adapted according to the evolutionary form and histological analysis, are currently being evaluated and could make it possible to reduce the risk of evolution towards a dilated cardiomyopathy.
Consent for Publication
In accordance with international and academic standards, written consent for publication was obtained from the patient and retained by the authors.
Conflicts of Interest
The authors declared no conflicts of interest.
References
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382: 1708-1720.
- Basso C, Calabrese F, Corrado D, Thiene G (2001) Postmortem diagnosis in sudden cardiac death victims: macroscopic, microscopic and molecular findings. Cardiovasc Res 50(2): 290-300.
- Oliva A, Grassi VM, Campuzano O, Brion M, Arena V, et al. (2016) Medico-legal perspectives on sudden cardiac death in young athletes. Int J Legal Med 131(2): 393-409.
- Caforio ALP, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, et al. (2013) Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J 34(33): 2636-2648.
- Mason JW, O’Connell JB, Herskowitz A, Rose NR, McManus BM, et al. (1995) A clinical trial of immunosuppressive therapy for myocarditis. Themyocarditis treatment trial investigators. N Engl J Med 333(5): 269-275.
- Wei X, Fang Y, Hu H (2020) Glucocorticoid and immunoglobulin totreat viral fulminant myocarditis. Eur Heart J 41(22): 2122.
- Chen C, Zhou Y, Wang DW (2020) SARS-CoV-2: a potential novel etiology of fulminant myocarditis. Herz 45(3) : 230-232.
- Hinojar R, Foote L, Ucar EA, Jackson T, Jabbour A, et al. (2015) Native T1 in discrimination of acute and convalescent stages in patients with clinical diagnosis of myocarditis: a proposed diagnostic algorithm using CMR. JACC Cardiovasc Imaging 8(1): 37-46.
- Aretz HT, Billingham ME, Edwards WD, Factor SM, Fallon JT, et al. (1987) Myocarditis. A histopathologic definition and classification. Am J Cardiovasc Pathol 1(1): 3-14.
- Frustaci A, Russo MA, Chimenti C (2009) Randomized study on the efficacy of immunosuppressive therapy in patients with virusnegative inflammatory cardiomyopathy: the TIMIC study. Eur Heart J 30(16): 1995-2002.
- Escher F, Kühl U, Lassner D, Poller W, Westermann D, et al. (2016) Long-term outcome of patients with virus-negative chronic myocarditis or inflammatory cardiomyopathy after immunosuppressive therapy. Clin Res Cardiol 105(12): 1011-1020.
- Hu H, Ma F, XWei X, Fang Y (2021) Coronavirus fulminant myocarditis treated with glucocorticoid and human immunoglobulin Eur Heart J 42(2): 206.






























